Abstract
Three species of tapeworms infect humans in their adult stage (Taenia solium, Taenia saginata and Taenia asiatica). The 3 are flat, opaque white or yellowish, and exceptional long segmented parasites, measuring 1 to 12 m in their adult stage. In this review, the development of the knowledge regarding the first species, mainly focused on understanding how the larval stage or cysticercus is transmitted to humans, is described. The second species is a cosmopolitan parasite that only causes taeniosis and not cysticercosis; therefore, it will not be included. Information on the third species, which is presently being produced, since this species was recognized as such only at the end of the 20th century, will be discussed at the end of this review.
-
Key words: Taenia solium, Taenia saginata, Taenia asiatica, control measure, cysticercosis, epidemiology, life cycle, parasite
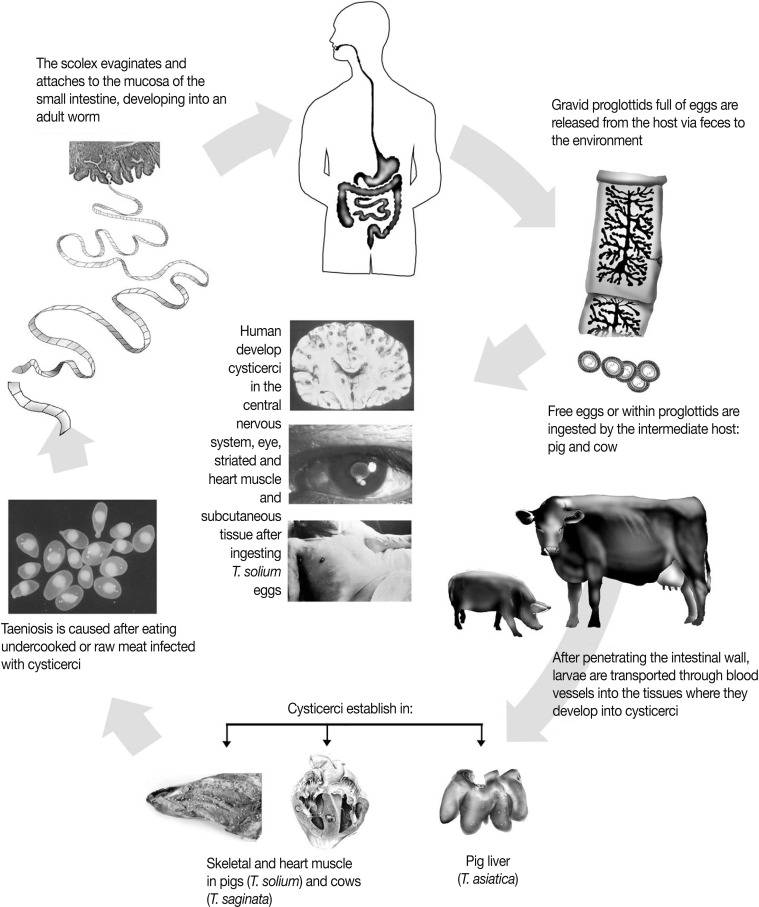
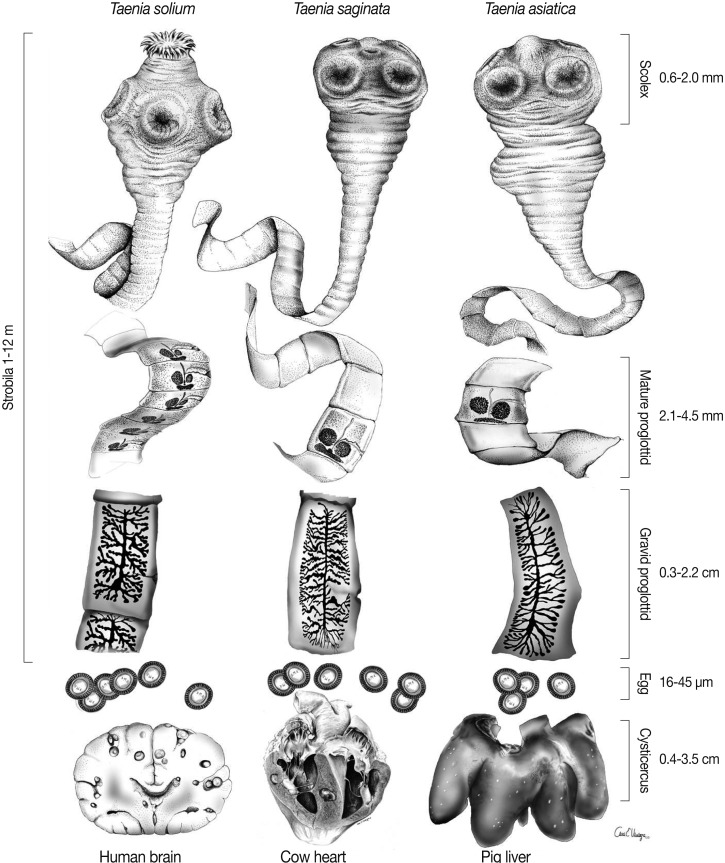
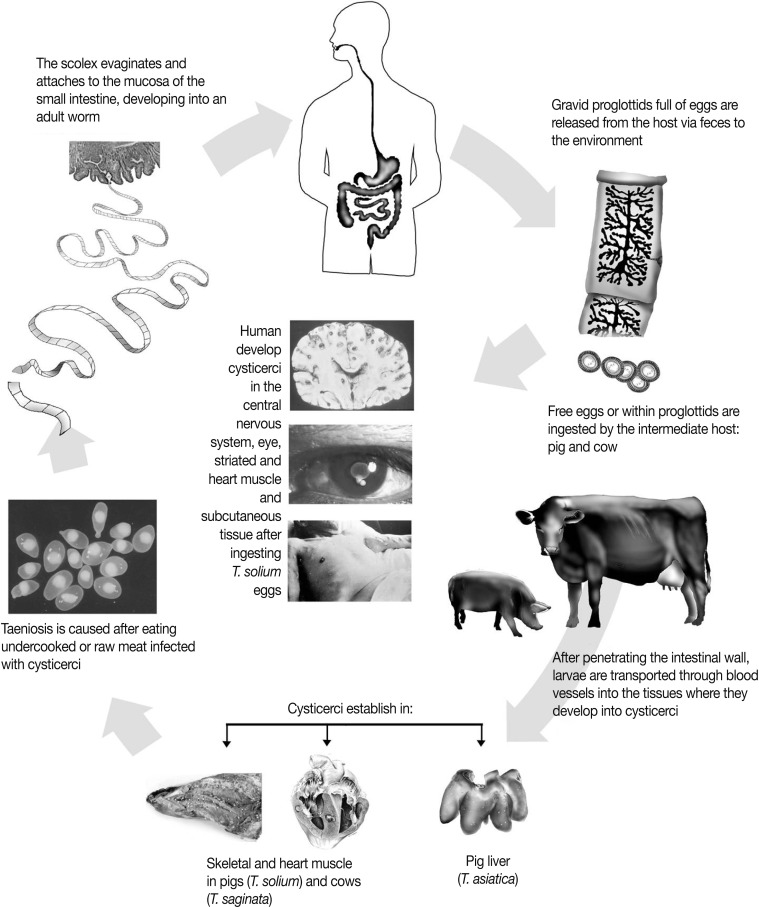
MORPHOLOGY AND LIFE CYCLE OF TAENIA SOLIUM
Taenia solium (
Fig. 1) is the parasite that causes human and swine cysticercosis. Human cysticercosis is a disease related to underdevelopment and poverty. It is found in countries and regions with inadequate sanitary infrastructure and insufficient health education. The life cycle of the parasite includes the adult stage, the egg, and the larval stage (cysticercus) [
1,
2]. When a person ingests raw or semi-cooked pork meat with cysticerci, the scolex evaginates and attaches with its double row of 22 to 32 hooks and its 4 suckers to the mucosa in the upper third section of the small intestine, which is the duodenum-jejunum, and in 3-4 months transforms into a fully developed adult tapeworm. Intestinal taeniosis almost never induces symptoms.
T. solium tapeworms measure 1-5 m long, and the scolex is followed by the neck, from which the strobila is formed, resembling a ribbon formed by 700 to 1,000 immature, mature, and gravid proglottids. The immature proglottids have not yet developed sexual organs while the gravid proglottids resemble sacs full of eggs. Mature proglottids are found between immature and gravid ones. Tapeworms are hermaphroditic organisms because each mature segment contains 350 to 600 testes and 3 ovary lobes. Gravid proglottids are released with feces, starting at 3-5 months after infection, and each proglottid contains between 50,000 and 60,000 eggs, located inside the multilobulated uterus. As proglottids are located farther away from the scolex they become bigger; mature proglottids measure 2.1 to 2.5 mm long and 2.8 to 3.5 mm wide, while gravid segments measure 3.1 to 10 mm long and 3.8 to 8.7 mm wide. Eggs are spherical and have a radial appearance. They range in size from 26 to 34 µm while cysticerci and adult worms are macroscopic and have a similar scolex that measures 0.6 to 1.0 mm. Eggs are conformed by the oncoshpere, or hexacanth embryo, and the embryophore that surrounds it. When swine ingest eggs, bile and enzymes disaggregate the embryophoric blocks and digest the oncospheral membrane; in this way the oncosphere, with the aid of its hooks and enzymes, can cross the mucosa and circulate until it transforms into the larval stage.
Cysticerci establish primarily in the skeletal and cardiac muscles, as well as in the brain of pigs, a process that takes approximately 3 months. They remain viable for at least 1 year, when pigs are usually sent to slaughter. In humans, 2 morphologic types develop; cellulose and racemose type cysticerci [
3]. The former is a small, spherical or oval, white or yellow, vesicle that measures between 0.5 and 1.5 cm and has a translucent bladder wall, through which the scolex can be seen as a small solid eccentric granule. This type of cysticerci is generally separated from the host tissue by a thin collagenous capsule, within which it remains alive. Pigs contain only this type of cysticerci. The racemose cysticercus appears in the human brain either as a large, round, or lobulated bladder circumscribed by a delicate wall, or resembles a cluster of grapes, and measures up to 10 or even 20 cm and may contain 60 ml fluid. Interestingly, the scolex cannot be seen, and in some cases only detailed histological studies reveal its remains. Cellulose type cysticerci are conformed by 2 chambers; the inner one contains the scolex and the spiral canal and is surrounded by the outer compartment that contains the vesicular fluid, usually less than 0.5 ml. When a person ingests a living cysticercus, the first event that takes place is the widening of the pore of the bladder wall for the scolex and neck to emerge, leaving the bladder wall and vesicular fluid to disintegrate in the digestive tract [
4]. It becomes the definitive host (
Fig. 2).
The domestic pig is the intermediate host because it harbors the cysticercus; however, humans can acquire cysticercosis after accidentally ingesting
T. solium eggs. Cysticerci in humans develop mainly in the central nervous system, eyes, striated and heart muscles, and subcutaneous tissues. In the brain, parasites can be found in the parenchyma, subarachnoid tissues, and ventricles [
5]. Clinical manifestations are pleomorphic, and depend on the location, number, and stages of the lesions as well as characteristics of the immune response of the host. The most frequent are epilepsy and hydrocephalus. In skeletal muscles, parasites can be palpated when superficial, or seen in X-rays as white dots or nodules, but generally they do not interfere with the muscle function, except in massive infections, when they cause muscle pseudo-hypertrophy with intense inflammation and pain. In cardiac muscles, cysticerci may develop myocardiopathy. In the eye, parasites are found in the subretinal space, close to the macula, vitreous fluid, or anterior chamber. Inflammation may cause blindness or decreased vision secondary to proliferative vitreo-retinopathy and retinal detachment.
Although some books state that tapeworms can survive for about 25 years in the human intestine, recent experience indicates that
T. solium remains only for around 1 year releasing along this time a few gravid proglottids in feces 2-3 times a week [
2]. Interestingly, the prevalence of taeniosis among patients with neurocysticercosis (NCC) is higher than previously reported. In addition, a clear association between the presence of taeniosis and the severity of NCC has been reported, since most massive cerebral infections (with more than 100 cysticerci) were present in patients who harbored the adult tapeworm in the intestine. Therefore, the perception that tapeworms are silent guests, causing no harm to humans, is erroneous and tapeworm carriers should be regarded as potential sources of contagion to themselves and to those living in their close environment [
6].
Taenia asiatica differs from
Taenia saginata and
T. solium in 4 aspects [
2]; 1) The scolex has 2 rows of rudimentary hooklets, which is considered as a wart-like formation. 2) The number of the lateral branches of the uterus is different and allows identifying if the proglottids belong to
T. solium (7-11 branches),
T. saginata (14-32 branches), or
T. asiatica (12-26 branches). 3)
T. asiatica cysticerci in pigs are not found in muscles, they can be recovered from the liver, omentum, serosa, and lung. 4)
T. asiatica does not cause NCC in humans.
ANTI-T. SOLIUM ANTIBODIES IN PEOPLE AND PIGS
Between 1940 and 1970, necropsy reports in Mexico indicated that around 2% of adults had NCC [
7,
8], and between 50 and 80% of them had no symptoms. In 1972, when I started my Ph.D. project, no computed tomography or magnetic resonance existed, and the only diagnostic procedure was using the cerebrospinal fluid, where antibodies by complement fixation and increase of eosinophils by differential count of blood cells, were the only methods to suggest cysticercosis in patients with neurologic symptoms such as convulsive crisis or hydrocephalus. Therefore, along the next 20 years, immunoelectrophoresis, enzyme immunoassays, including ELISA, and western blot were standardized with the aim of defining the real magnitude of
T. solium in Mexico by detecting specific anti-cysticercus antibodies in serum [
7,
9-
13].
Immunoelectrophoresis was the first technique used in communities [
14,
15]; 1,610 samples obtained from 9 communities, mostly rural, in the state of Chiapas were analyzed. Interestingly, in spite of the low sensitivity of immunoelectrophoresis (50%), its high specificity (100% because practically no echinococcosis is found in Mexico) allowed to identify a clear correlation. Communities with less than 4,000 inhabitants had 1-8% seropositivity, while populations with up to 35,000 citizens had 1% or less antibody frequency; indicating that the parasite was more frequent in small, and thus less developed, towns [
7]. Afterwards, a study performed in 20,000 samples from a national survey, we were able to identify by immunoelectrophoresis a central area in Mexico in which people had between 0.6 and 1% of anti-cysticercus antibodies; remarkably, this geographic area, called "El Bajio" is the most important pig breeding area in Mexico for national consumption of pork meat [
16].
A few years later in a small field practice for a group of epidemiology students, we identified the main risk factor for acquiring cysticercosis; the tapeworm carrier, probably my main contribution to science [
17]. This was recognized because there were "clusters" in the community (125 inhabitants) where people with convulsive crisis and/or antibodies by ELISA and pigs with cysticerci in the tongue lived close to a tapeworm carrier [
17]. This finding was confirmed in other studies.
A survey was performed in a soldier camp in Mexico City, blood and fecal samples from 1,000 militaries and their families were analyzed for
T. solium serum ELISA antibodies, copro-antigen ELISA, and coproparasitoscopic detection of eggs [
18]. Demographic results were gathered in relation to positivity to any assay; 86.7% of family members of positive soldiers ate in street food stores, as compared to 62.5% of family members of negative soldiers, while having a history of proglottid release was 12% vs 3.7% in the same family groups [
18]. These results confirmed the importance of a tapeworm carrier in the household.
Probably the study that was better known around the world, but certainly was not the first one, was that with the 4 families of Orthodox Jews that along 2 years each had a member that had convulsive crisis, which was confirmed at the Center for Disease Control, Atlanta, USA as due to NCC [
19]. It took a big effort to Dr. Peter Schantz to identify the risk factor, because being Orthodox they did not want to know anything about "the pig tapeworm". He found out that they spent the previous vacation together and took with them a maid from Mexico, and obtained the data from the maid; we fetched her in the state of Puebla and identified that she had a tapeworm, her brother and son had NCC; also 7 other asymptomatic members from the Jewish families were antibody positive by western blot [
19]. Thus, 1 tapeworm carrier in the household, who cooked and most probably had inadequate hygienic habits, infected 13 people.
EVALUATION OF INTERVENTION MEASURERS FOR CONTROL
Starting 1990 we performed studies with the support of the International Development Research Center, Ottawa, Canada in order to evaluate different intervention measures for control of human cysticercosis; health education related to the life cycle of
T. solium and the risk factors for acquiring cysticercosis, as well as mass treatment with praziquantel against taeniosis [
7,
20-
24]. A huge field study was established along 2 years in which all the inhabitants of 3 communities (around 3,000 in each) were asked for blood and fecal samples; in depth sociological interviews were performed in 10% of the people in order to develop the educational intervention. Praziquantel (kindly donated by Merck Mexico) was provided in 2 communities and health education in the other 2, in such a way that 1 community received only the cestocide drug, 1 only the education program, and 1 community both measures. Praziquantel was used at 5 mg/kg weight instead of 10 mg/kg in order to avoid neurologic exacerbation if cysticerci were lodged in the brain [
23]; but unfortunately its cestocidal effect was also reduced to 54% instead of the 95% expected [
20]. In contrast, health education was so effective that no pigs born after the intervention had cysticerci up to 40 month after this measure was implemented. This formidable effect could be due to the fact that people learned that if their pigs had no access to human feces (in latrines, garbage, or due to free roaming) they would not acquire the disease, and thus could be sold in a better price.
A recombinant vaccine against swine cysticercosis, named TSOL18, was produced by Dr. Marshall Lightowlers, and was evaluated in Mexico [
25,
26], and later on in Peru [
6] and Cameroon [
26]. This is, up to date, the vaccine against any parasite with the highest efficiency; 100% of immunized pigs did not develop cysticerci after experimental infections with
T. solium eggs or in spite of living in highly contaminated environments.
Another intervention was assessed in a jurisdiction of "El Bajio" with more than 750,000 inhabitants, in which doctors in health centers were given a small flask with some
T. solium proglottids, and invited to ask the patients that attended for any reason, if they or someone at home released segments as those in the flask [
27]. Patients were also asked if a member of the household had convulsive crisis or if they had "measly pigs" at home. To those with a positive answer, praziquantel at 10 mg/kg was offered. Announcements in walls, radios, newspapers, and short courses were provided in the entire jurisdiction. The year before and at the end of the year in which the intervention took place, annual data were obtained from the official disease notification system at the Ministry of Health; 7 cases vs 41 of taeniosis were detected before and after; also NCC increased from 16 to 68 cases and swine cysticercosis from 2 to 17, because people became aware of the disease. All tapeworm carriers were treated (4 worms were
T. solium, the remainings were
T. saginata), as expected only 10% of the tapeworms were
T. solium. Patients with NCC were transferred to second level hospitals.
I consider that I am closing my research circle on cysticercosis, since this disease has been controlled in Mexico [
6]. This reflection is based on the dramatic decrease in the frequency of human NCC and of human taeniosis that has been taking place in Mexico in the last 20 years, according to the official national notification system that is collected by the Ministry of Health [
8]. The explanation for this reduction is based on a sequence of events that started with the publications produced along the last 40 years by Mexican scientific and medical communities working on cysticercosis. The vast amount of information published most probably promoted the establishment of a national program for the control of
T. solium (Guidelines for the Prevention and Control of Taeniosis and Cysticercosis, NOM 021 SSA2-1994, 2004) that are obligatory to follow in the whole nation, lead by the Ministry of Health. Finally, in Mexico, a general improvement of living conditions has taken place, which has had a positive impact in the reduction of NCC and swine cysticercosis [
8].
T. SOLIUM AS COMPARED TO T. ASIATICA
The last aspect of this review is to focus towards comparing research related to
T. solium and
T. asiatica. The main concept is to understand the difference between having the disease and being a tapeworm carrier. Cruz et al. [
28], in their operational studies on the control of
T. solium taeniasis/cysticercosis in Ecuador, calculated that expulsion of a tapeworm by at least 148 carriers reduced the exposure to
T. solium eggs both for man and pigs in the study areas, and considered that with a relatively low reinfection rate, this human reservoir of infection would remain diminished for several years. In this way, the real disease, NCC, can be controlled.
On the other hand, the group of Jeon et al. [
29] described that nationwide surveys conducted every 5 years in Korea revealed that the positivity rate for taeniid eggs decreased from 1.9% in 1969 to 0.02% in 1997, and human taeniosis was no more detected in the 2004 survey. Eom et al. [
30] also indicated that during the period of 1998 and 2002, a total of 19,894 Chinese inhabitants of 3 ethnic minorities in Guangxi Province, China were surveyed for
Taenia worms. A total of 927 (4.7%) persons discharged proglottids, and, in 2002, 108 were treated, and 117 adult tapeworms were recovered. Using surveys in order to retrieve tapeworms in Asian countries suggests that carriers do not attend health institutions for clinical symptoms, indicating that taeniosis does not cause a disease.
I personally consider that the 3 species of human tapeworms should be dealt as different concepts.
T. solium has to be eliminated from carriers because it is the main risk factor for NCC, a devastating disease;
T. saginata causes minor symptoms due to the discharge of proglottids [
22,
31]. If patients feel the need to be treated they can attend any health institution. The adult parasites of
T. asiatica do not cause disease, since they are not associated with symptomatology that requires medical treatment. Therefore, Asian scientists should not thrive towards its eradication.
The 2 most important justifications of my reasoning are: 1) In the last few years, clinical and basic studies are demonstrating with increased numbers of publications and of clinical successes that helminths participate in immunomodulating the intestinal milieu in order to reduce inflammatory bowl diseases (usually referred to as IBD), such as Crohn's disease, that are becoming very prevalent in developed countries around the world [
32-
37]. 2) The world's biodiversity is being threatened because of the huge human development; there is no need to further reduce it.
References
- 1. Flisser A, Viniegra AE, Aguilar-Vega L, Garza-Rodriguez A, Maravilla P, Avila G. Portrait of human tapeworms. J Parasitol 2004;90:914-916.
- 2. Flisser A, Craig PS, Ito A. In Palmer SR, Soulsby L, Torgerson PR, Brown DWG eds, Cysticercosis and taeniosis: Taenia solium, Taenia saginata and Taenia asiatica. Oxford Textbook of Zoonoses, Biology, Clinical Practice and Public Health Control. 2011, Oxford, UK. Oxford University Press; pp 627-644.
- 3. Rabiela MT, Rivas A, Flisser A. Morphological types of Taenia solium cysticerci. Parasitol Today 1989;5:357-359.
- 4. Rabiela MT, Ornelas Y, García-Allan C, Rodríguez del Rosal E, Flisser A. Evagination of Taenia solium cysticerci: a histologic and electron microscopy study. Arch Med Res 2000;31:605-607.
- 5. Flisser A. Neurocysticercosis in Mexico. Parasitol Today 1988;4:131-137.
- 6. Gilman RH, Del Brutto OH, García HH, Martínez M. the Cysticercosis Working Group in Perú. Prevalence of taeniosis among patients with neurocysticercosis is related to severity of infection. Neurology 2000;55:1062.
- 7. Flisser A, Gyorkos TW. Contribution of immunodiagnostic tests to epidemiological/intervention studies of cysticercosis/taeniosis in México. Parasite Immunol 2007;29:637-649.
- 8. Flisser A, Correa D. Neurocysticercosis may no longer be a public health problem in Mexico. PLoS Negl Trop Dis 2010;4:e831. (doi:10.1371/journal.pntd.0000831)
- 9. Flisser A, Woodhouse E, Larralde C. Human cysticercosis: antigens, antibodies and non-responders. Clin Exp Immunol 1980;39:27-37.
- 10. Espinoza B, Flisser A, Plancarte A, Larralde C. In Flisser A, Willms K, Laclette JP, Larralde C, Ridaura C, Beltrán F eds, Immunodiagnosis of human cysticercosis: ELISA and immunoelectrophoresis. Cysticercosis. Present State of Knowledge and Perspectives. 1982, N.Y., USA. Academic Press; pp 163-170.
- 11. Espinoza B, Ruiz-Palacios G, Tovar A, Sandoval MA, Plancarte A, Flisser A. Characterization by enzyme-linked immunosorbent assay of the humoral immune response in patients with neurocysticercosis and its application in immunodiagnosis. J Clin Microbiol 1986;24:536-541.
- 12. Correa MD, Plancarte A, Sandoval MA, Rodríguez-del-Rosal E, Meza-Lucas A, Flisser A. Immunodiagnosis of human and porcine cysticercosis. Detection of antibodies and parasite products. Acta Leidensia 1989;57:93-101.
- 13. Allan JC, Avila G, García-Noval J, Flisser A, Craig PS. Immunodiagnosis of taeniasis by coproantigen detection. Parasitology 1990;101:473-477.
- 14. Flisser A, Tarrab R, Willms K, Larralde C. Immunoelectroforesis y doble immunodiffusión en la diagnóstico de la cisticercosis cerebral humana. Arch Invest Med (Mex) 1975;6:1-12.
- 15. Flisser A, Pérez-Montfort R, Larralde C. The immunology of human and animal cysticercosis: a review. Bull World Health Org 1979;57:839-856.
- 16. Woodhouse E, Flisser A, Larralde C. In Flisser A, Willms K, Laclette JP, Larralde C, Ridaura C, Beltrán F eds, Seroepidemiology of human cysticercosis in México. Cysticercosis. Present State of Knowledge and Perspectives. 1982, N.Y., USA. Academic Press; pp 11-23.
- 17. Sarti-Gutierrez EJ, Schantz PM, Lara-Aguilera R, Gómez-Dandoy H, Flisser A. Taenia solium taeniasis and cysticercosis in a Mexican village. Trop Med Parasitol 1988;39:194-198.
- 18. García-García MDL, Torres M, Correa D, Flisser A, Sosa-Lechuga A, Velasco O, Meza-Lucas A, Plancarte A, Avila G, Tapia R, Aguilar L, Mandujano A, Alcántara I, Morales Z, Salcedo A, Maňón MDLL, Valdespino-Gomez JL. Prevalence and risk of cysticercosis and taeniasis in an urban population of soldiers and their relatives. Am J Trop Med Hyg 1999;61:386-389.
- 19. Schantz PM, Moore AC, Muñoz JL, Hartman BJ, Schaefer JA, Alan AM, Persaud D, Sarti E, Wilson M, Flisser A. Neurocysticercosis in an Orthodox Jewish community in New York City. New Engl J Med 1992;327:692-695.
- 20. Sarti E, Schantz PM, Avila G, Ambrosio J, Medina-Santillán R, Flisser A. Mass treatment against human taeniasis for the control of cysticercosis: a population-based intervention study. Trans R Soc Trop Med Hyg 2000;94:85-89.
- 21. Sarti E, Flisser A, Schantz PM, Gleizer M, Loya M, Plancarte A, Avila G, Allan J, Craig P, Bronfman M, Wijeyaratne P. Development and evaluation of a health education intervention against Taenia solium in a rural community in Mexico. Am J Trop Med Hyg 1997;56:127-132.
- 22. Flisser A. Where are the tapeworms? Parasitol Int 2006;55:S117-S120.
- 23. Flisser A, Sarti E, Lightowlers M, Schantz P. Neurocysticercosis: regional status, epidemiology, impact and control measures in the Americas. Acta Trop 2003;87:43-51.
- 24. Flisser A, Rodríguez-Canul R, Willingham AL III. Control of the taeniosis/cysticercosis complex: future developments. Vet Parasitol 2006;139:283-292.
- 25. Flisser A, Lightowlers MW. Vaccination against Taenia solium cysticercosis. Mem Inst Oswaldo Cruz 2001;96:353-356.
- 26. Flisser A, Gauci CG, Zoli A, Martinez-Ocaña J, Garza-Rodriguez A, Dominguez-Alpizar JL, Maravilla P, Rodriguez-Canul R, Avila G, Aguilar-Vega L, Kyngdon C, Geerts S, Lightowlers MW. Protection against porcine cysticercosis induced by vaccination with recombinant oncosphere antigens. Infect Immun 2004;72:5292-5297.
- 27. Flisser A, Vázquez-Mendoza A, Martínez-Ocaña J, Gómez-Colín E, Sánchez Leyva R, Medina-Santillán R. Evaluation of a self-detection tool for tapeworm carriers for use in public health. Am J Trop Med Hyg 2005;72:510-512.
- 28. Cruz M, Davis A, Dixon H, Pawlowski ZS, Proano J. Operational studies on the control of Taenia solium taeniasis/cysticercosis in Ecuador. Bull World Health Org 1989;67:401-407.
- 29. Jeon HK, Kim KH, Chai JY, Yang HJ, Rim HJ, Eom KS. Sympatric distribution of three human Taenia tapeworms collected between 1935 and 2005 in Korea. Korean J Parasitol 2008;46:235-241.
- 30. Eom KS, Jeon HK, Rim HJ. Geographical distribution of Taenia asiatica and related species. Korean J Parasitol 2009;47:S115-S124.
- 31. Flisser A. In Farthing MJG, Keusch GT, Walekin D eds, Taenia solium, Taenia saginata and Hymenolepis nana. Enteric infections. 2: Intestinal Helminths. 1995, London, UK. Chapman and Hall Medical; pp 173-189.
- 32. Elliott DE, Summers RW, Weinstock JV. Helminths as governors of immune-mediated inflammation. Int J Parasitol 2007;37:457-464.
- 33. Elliott DE, Weinstock JV. Helminthic therapy: using worms to treat immune-mediated disease. Adv Exp Med Biol 2009;666:157-166.
- 34. Elliott DE, Weinstock JV. Helminth-host immunological interactions: prevention and control of immune-mediated diseases. Ann N Y Acad Sci 2012;1247:83-96.
- 35. Maizels RM, Pearce EJ, Artis D, Yazdanbakhsh M, Wynn TA. Regulation of pathogenesis and immunity in helminth infections. J Exp Med 2009;206:2059-2066.
- 36. Weinstock JV. Helminths and mucosal immune modulation. Ann N Y Acad Sci 2006;1072:356-364.
- 37. Weinstock JV, Elliott DE. Helminths and the IBD hygiene hypothesis. Inflamm Bowel Dis 2009;15:128-133.
Fig. 1Three human Taenia tapeworms showing details in morphologic features and size range (This figure has been modified from Fig. 1 of Flisser et al., Portrait of human tapeworms. J Parasitol 2004; 90: 914-916).
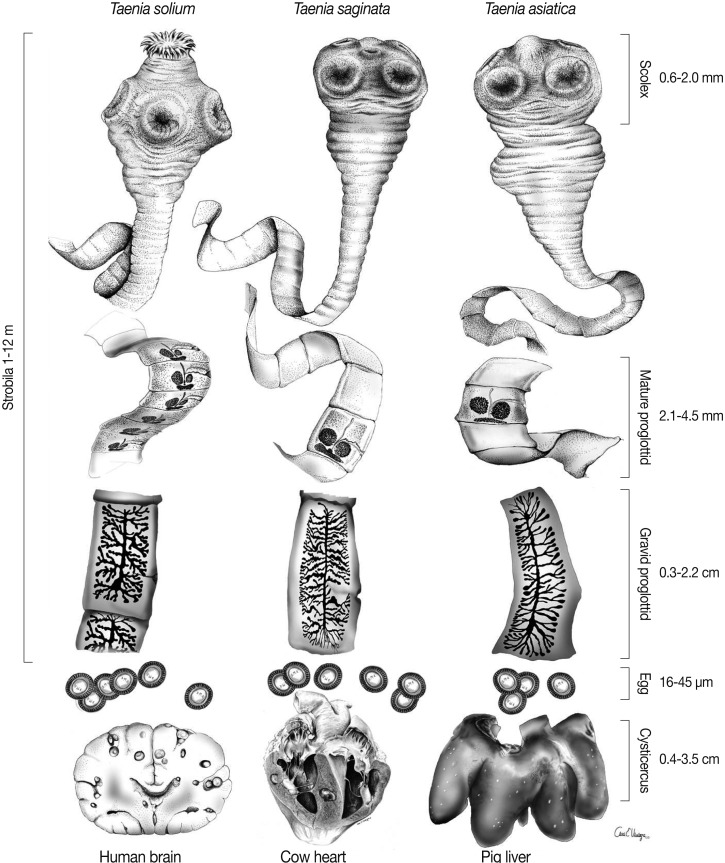
Fig. 2Life cycles of the 3 human Taenia tapeworms (This figure has been modified from Fig. 1.2 of Flisser et al., Biology of Taenia solium, T. saginata, and T. asiatica. In Murrell KD ed, WHO/FAO/OIE Guidelines for the surveillance, prevention, and control of taeniosis/cysticercosis. 2005, pp 1-9).