High Prevalence of Haplorchiasis in Nan and Lampang Provinces, Thailand, Proven by Adult Worm Recovery from Suspected Opisthorchiasis Cases
Article information
Abstract
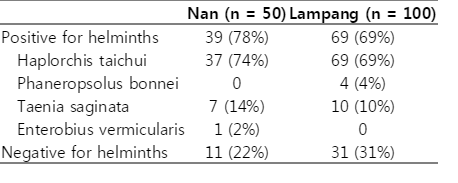
Opisthorchiasis, a risk factor for cholangiocarcinoma in humans, is of public health importance in Thailand. The Annual Surveillance Reports from Nan and Lampang Provinces, Thailand, for the year 2011 showed an opisthorchiasis prevalence of over 70% by recovery of eggs in the feces. This study investigated whether most cases are actually due to minute intestinal flukes (MIF) rather than Opisthorchis viverrini, as the eggs of both can hardly be differentiated by morphology. Fifty and 100 cases from residents in Nan and Lampang, respectively, had stools positive for eggs initially assumed to be those of O. viverrini. Each patient was given praziquantel at 40 mg/kg in a single dose. After 2 hr, 30-45 ml of the purgative magnesium sulfate was given, and stools were collected up to 4 times sequentially. The stools were examined for adult worms by simple sedimentation. It was found that 39 of 50 cases (78.0%) from Nan Province had Haplorchis taichui, with intensities ranging from 5 to 1,250 with an average of 62 worms/case. Taenia saginata (7 cases) and Enterobius vermicularis (1 case) were other helminths recovered as the co-infectants. In Lampang Province, H. taichui was recovered from 69 cases (69.0%). The number of flukes recovered ranged from 1 to 4,277, with an average of 326 worms/case. Four cases had Phaneropsolus bonnei, and 10 T. saginata as the co-infectants. Adult specimens of O. viverrini were not recovered from any stool. Clearly, MIF infection, especially haplorchiasis, is more common in northern Thailand. These findings should encourage the Public Health Office to employ more specific tools than Kato's method for surveillance of opisthorchiasis in Thailand.
Foodborne trematodiasis is a public health problem. A global estimate of 56.2 million people were infected with trematodes, resulting in DALY (disability-adjusted life year) of 0.5-0.9 million and 7,152 deaths per year [1]. One of these trematodes, Opisthorchis viverrini, is associated with cholangiocarcinoma, and about 10 million people in Thailand and Lao PDR are infected [1]. To control this liver fluke disease, the Ministry of Public Health, Thailand, has set a target of not exceeding 5% prevalence. A cross-sectional survey in 2009 demonstrated a national prevalence of 8.7% (based on the finding of eggs in stool samples), which was a decrease figure from 14% in 1971. The prevalence was the highest in northeastern (16.6%) and northern Thailand (10%) [2]. However, the true prevalence of opisthorchiasis may be overestimated in areas where O. viverrini coexists with minute intestinal flukes (MIFs). The eggs of Opisthorchis and of MIFs are easily confused under a microscope unless specific techniques are used [3-5]. A recent unpublished report from local health authorities stated that the prevalence of O. viverrini eggs in the stools of residents in Nan and Lampang Provinces, northern Thailand, was over 70%. This alarming finding prompted our study, which reports the adult MIFs recovered after anthelminthic treatment in subjects who had eggs in their stool that had been assumed to be those of O. viverrini.
Villagers were selected from Bo Kluea District, Nan Province (n=50), and Chae Hom District, Lampang Province (n=100), northern Thailand. These areas were under Her Royal Highness Princess Maha Chakri Sirindhon's Project for Remote Area Development. Cases with stools previously reported to contain O. viverrini eggs, identified by Kato's thick smear technique, were tracked from hospital records, District Health Office records, or both. Fresh stool samples were collected and re-examined. Praziquantel at 40 mg/kg was given to each patient in a single oral dose. Magnesium sulfate was administered 2 hr later to facilitate stool collection process. Stools were collected up to 4 times consecutively. After simple sedimentation in 0.85% sodium chloride solution, the sediments were examined under a stereomicroscope. Worms were collected, stained with carmine, and morphologically identified. Haplorchis taichui was identified based on the characteristics of spines in the ventro-genital complex, according to Pearson and Ow-Yang [6]. Phaneropsolus bonnei was identified based on the morphology described by Manning et al. [7]. Taenia proglottides were differentiated into T. saginata or T. solium by the India ink injection technique, and lateral uterine branches were counted [8]. Enterobius vermicularis was morphologically identified according to standard textbooks.
Results of the survey are summarized in Table 1. H. taichui was the only fluke found in Nan Province (intensity of infection 5-1520; mean 62 worms per case). In Lampang Province, both H. taichui (intensity of infection 1 to 4,277; mean 326 worms per case) and P. bonnei were discovered. The tapeworm co-infectant was T. saginata, 7 cases in Nan and 10 cases in Lampang, respectively, while the only co-infected nematode was E. vermicularis found in 1 case in Nan.
Surveillance of opisthorchiasis is required by the Ministry of Public Health, Thailand, under the Helminth Control Program. Consequently, diagnostic methods must be specific. Unfortunately, the Kato's cellophane thick smear technique is a method of choice for helminth surveys. It is cheap and permits detection of eggs of several common helminths. However, it is not specific for Opisthorchis eggs in areas where co-infection with MIFs is evident [9]. The present findings indicate that the reported high prevalence of opisthorchiasis in Nan and Lampang Provinces was spurious. In fact, anthelmintic treatment revealed that most of the cases had haplorchiasis. These results are supported by similar findings in a previous report, which showed that H. taichui eggs were found by the formalin-ether concentration technique in up to 48.4% of adult villagers and 14.9% of schoolchildren in Chaloem Phra Kiat District, Nan Province, during a 2002-2004 survey [10]. Infection was confirmed in that case by worm recovery after albendazole treatment [10]. Opisthorchis eggs were not detected in that study. Previously, a cross-sectional survey of schoolchildren in Bo Kluea, Nan Province, revealed O. viverrini eggs in 1.7% of them, but worm recovery was not carried out to confirm the findings [11]. Failure to find adult O. viverrini in our study, however, does not rule out the possibility that infected cases exist, but with low prevalence and intensity. Similarly, haplorchiasis is more prevalent than liver fluke infection in some areas of Laos [12,13]. Although clinically less important than opisthorchiasis, a link between haplorchiasis and irritable bowel syndrome has been suggested [14]. Thus, care must be taken when reporting O. viverrini eggs using Kato's thick smear technique. More accurate diagnostic techniques such as PCR may be essential in the future.
ACKNOWLEDGMENT
This study was supported in part by the TRF Senior Research Scholar Grant, Thailand Research Fund grant no. RTA5580004 to Wanchai Maleewong.