Recent Situation of Taeniasis in Mongolia (2002-2012)
Article information
Abstract
Epidemiological situation of taeniasis in Mongolia was assessed based on mitochondrial DNA identification of the parasite species. Multiplex PCR was used on a total of 194 proglottid specimens of Taenia species and copro-PCR and loop-mediated isothermal amplification (LAMP) assays were utilized for detection of copro-DNA of 37 fecal samples from taeniasis patients submitted to the Mongolian National Center for Communicable Diseases (NCCD) from 2002 to 2012. In addition, 4 out of 44 calcified cysts in beef kept in formalin since 2003 were evaluated for histopathological confirmation of cattle cysticercosis. All proglottid specimens and stool samples were confirmed to be Taenia saginata by multiplex PCR and by copro-PCR and LAMP, respectively. Cysts collected from cattle were morphologically confirmed to be metacestodes of Taenia species. T. saginata taeniasis was identified from almost all ages from a 2-year-old boy up to a 88-year-old woman and most prominently in 15-29 age group (37%, 74/198) followed by 30-44 age group (34.8%, 69/198 ) from 15 of Mongolia's 21 provinces, while cattle cysticerci were found from 12 provinces. The highest proportion of taeniasis patients was in Ulaanbaatar, the capital of Mongolia.
Mongolia has a population of around 2.8 million people and approximately 30% of the population is nomadic or semi-nomadic. Ulaanbaatar, the capital and the largest city of the country, is home to about 45% of the total population. Mongolia is divided into 21 provinces (Fig. 1).

A map of Mongolia showing the geographical origins of Taenia saginata detected from people and cattle. Numbers in open rectangle and open circle show human taeniasis cases and cattle cysticercosis, respectively.
A large proportion of the population is involved with the livestock industry, including approximately 300,000 herdsmen. As of the end of 2012, there were 40.9 million livestock in Mongolia, including 2.3 million horses, 2.6 million cattle, 17.5 million goats, 18.1 million sheep, and 305 thousand camels [1]. Meat makes up a large component of the Mongolian diet, with an average Mongolian consuming 97.6 kg of meat annually, of which beef and mutton make up approximately 61% [2].
The most popular human parasite is Enterobius vermicularis (National Center for Communicable Diseases, NCDD, Ulaanbaatar, unpublished). It is rather easy to speculate the reason why enterobiasis is so common in Mongolia, since the majority of Mongolian people, especially herdsmen and their family members live in 1 room of Gers and 24-hr daily life is completed in the room. Taeniasis is the second most common parasitic infection detected in humans in Mongolia. By questionnaire, 5.5% of individuals of Mongolian population tested were positive for Taenia saginata infection (Yondon D, Ph.D. thesis paper entitled "Distribution of taeniasis in Mongolia" submitted to Health Sciences University of Mongolia, 1973). A second questionnaire study found 13.4% and 7.2% of the Mongolian population infected with T. saginata in the forest-steppe and steppe regions, respectively (Dorjsuren T, Ph.D. thesis paper entitled "Prevalence of taeniasis and cysticercosis in Mongolia and usage of immunological methods for their diagnosis" submitted to Health Sciences University of Mongolia, 2003). The present study reports the distribution of T. saginata taeniasis cases identified through the National Center for Communicable Diseases, Ulaanbaatar, Mongolia between 2002 and 2012 and data from cattle mentioned above.
Between 2002 and 2012, parasite and stool samples of taeniasis patients were submitted to the Laboratory of Parasitology, National Center for Communicable Diseases, Ulaanbaatar from the local (district or province) health centers for species identification. This study was launched based on the ethical approval of NCCD, Ministry of Health, Mongolia. Therefore, we did not receive IRB (institutional review board) approval to use these samples. All data were handled for this study as anonymous. A total of 194 taeniid proglottids (19, 24, 23, 38, 14, 7, 25, 9, 9, 16, and 10 proglottids in each year from 2002 to 2012)and 37 stool samples (21 in 2010, 10 in 2011, and 6 in 2012) from 198 taeniasis cases were submitted to NCCD for species identification (Fig. 1; Table 1). The proglottid specimens and fecal samples were kept in 99.5% ethanol for molecular identification after collection. A total of 44 cattle cysts found from beef in slaughter house before 2003 have been kept in formalin.
DNA from each taeniid proglottid was extracted using a DNeasy tissue kit (Qiagen, Hilden, Germany) according to the manufacturer's instructions. DNA from fecal samples of tapeworm carriers was extracted using the QIAamp DNA Stool Minikit after disruption of embryophores with glass beads [3]. The extracted DNA was kept at -20℃ until further analysis could be performed.
Multiplex PCR and copro-PCR were performed using the cytochrome c oxidase subunit 1 gene (cox1) (984 bp for T. solium Asian genotype, 827 bp for T. saginata, and 588 bp for T. asiatica) for molecular identification of the proglottid specimens and fecal samples, respectively, as described previously [4]. For copro-PCR, bovine serum albumin (BSA) at a final concentration of 0.1 µg/µl was added to the samples for a total PCR mixture volume of 50 µl. An annealing temperature of 56℃ was used. For the nested PCR, 2.5 µl of the first PCR product was added to a second PCR reaction mixture, but without BSA. PCR-amplified products were electrophoresed on 1.5% agarose gels.
LAMP assays with cox1 primer sets were used for differential detection of Taenia species in the fecal samples. The same 37 copro DNA samples were used for the LAMP assays as analyzed by multiplex PCR. LAMP reactions were performed according to previously reported methods [5,6].
PCR products with molecular size of 827 bp were amplified from all proglottids (figure not shown). All stool samples from 37 taeniasis patients were amplified using copro-PCR for T. saginata. Of these samples, 29 (78%) and 8 samples (22%) were positive for T. saginata after the first and the second round of PCR, respectively, and all 37 samples were confirmed to be T. saginata by LAMP (figure not shown). Four cysts collected from cattle were histopathologically observed under a microscope and were confirmed as metacestodes of Taenia species (Fig. 2).
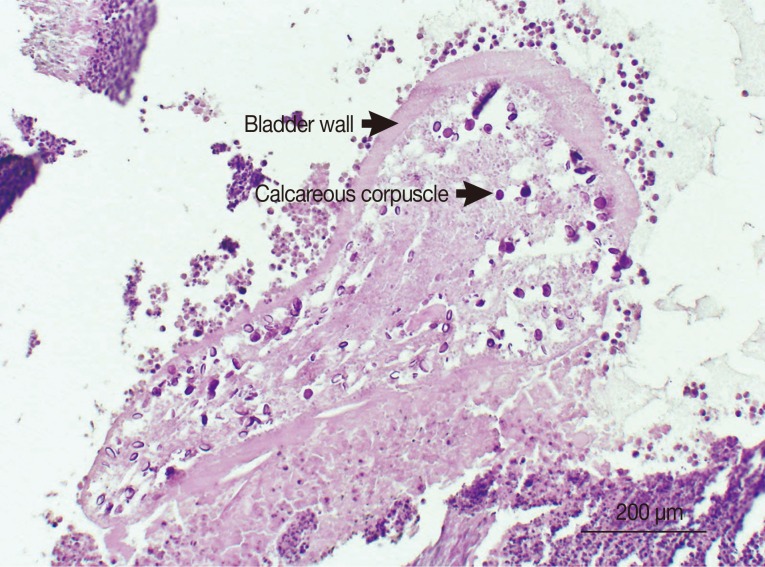
Histopathological image of a metacestode in beef (PAS stain). Calcareous corpuscles specific to cestodes are shown inside the bladder wall.
T. saginata taeniasis patients were identified from 15 of 21 Mongolian provinces (Fig. 1). The highest proportion of patients was reported from Ulaanbaatar, the capital of Mongolia (60.6%, 120/198). Fig. 1 and Table 1 are also showing the cattle cysticercosis found from beef in 12 provinces of Mongolia in 2003.
There was no significant difference in the proportion of T. saginata taeniasis cases between males (45.4%, 90/198) and females (54.5%, 108/198). The largest proportion of T. saginata carriers were from the 15 to 29-year age group (37.3%, 74/198), followed by the 30 to 44-year age group (34.8%, 69/198), the ≥45-year age group (21.2%, 42/198), the 5 to 14-year age group (5%, 10/198), and the 1 to 4-year age group (1.6%, 3/198). The youngest T. saginata carrier was a 2-year-old boy and the oldest carrier was an 88-year-old woman. Middle-aged male and female population of ≥15 years old made up the largest number of T. saginata taeniasis cases. The taeniasis patients were distributed among people with various occupations but herdsmen made up the largest proportion of taeniasis cases (18.6%, 37/198).
Nomadic or semi-nomadic people set up a designated latrine area associated with the household. However, latrines are not readily available in open pastureland where the herdsmen actually spend most of time. Therefore, indiscriminate defecation due to lack of knowledge about the parasite life cycle and a nomadic life style are most likely contributing to the maintenance of the T. saginata life cycle in Mongolia.
Herdsmen periodically slaughter cattle for personal consumption or sale. Selling meat without veterinary inspection is common in rural areas, and it promotes transmission of Taenia species. Most Mongolian families prepare and preserve 1-2 whole beef in November or December for use during the cold season (December-April). The high meat content (mainly beef and mutton) of the Mongolian diet may increase the risk of being infected with T. saginata taeniasis through the possibility of increased exposure to the infective source, whereas consumption of pork, the risk factor of T. solium taeniasis and neurocysticercosis, is not so common in Mongolians. We have no T. solium specimens confirmed from either humans or pigs so far.
The highest proportion of taeniasis patients was in Ulaanbaatar. However, approximately 61% of human population in Mongolia is living in Ulaanbaatar. Their majority is transmigrants from other rural areas, and T. saginata is expected to survive for a long term such as 10-30 years. It is, therefore, not clear if residents in Ulaanbaatar got infection in Ulaanbaatar or not. We rather expect that taeniasis carriers got infection during their stay in out of Ulaanbaatar. In Mongolia, the source of infection for T. saginata remains largely unknown since the Mongolian people do not eat raw or undercooked meat. However, people may become infected with taeniasis as a result of tasting minced and seasoned raw beef when preparing traditional foods such as "buuz", "huushuur", and "bansh" (dumplings). Also, limited health education and poor hygienic practices such as cross contamination of raw meat and other food products most likely contribute to the number of T. saginata infections. Nomadic herdsmen who live in traditional tents called "Gers" without indoor latrine made up the largest number of cases. Thus, indiscriminate defecation is believed to contribute to the contamination of pastures by human feces.
The cysts in beef were histopathologically confirmed to be Taenia species (Fig. 2). However, we could not succeed in confirmation of T. saginata using molecular tools. It may be due to the poor quality of cysts fixed in poor quality formalin for a long term. Therefore, the weakest point of this study is the lack of most recent objective evidence for human infections. The molecular identification of T. saginata cysticerci from cattle remains to be confirmed for understanding the transmission ecology and future prevention of human taeniasis in Mongolia. In conclusion, this study revealed that T. saginata taeniasis patients were distributed widely in 15 of 21 Mongolian provinces. Molecular identification of both expelled parasite specimens and stool samples revealed that all the taeniasis cases were infected with T. saginata. This is the first report to utilize the copro-PCR and LAMP assays to confirm the Taenia species from taeniasis carriers in Mongolia and the second one using the PCR method [7].
ACKNOWLEDGMENTS
This work was supported by the Asian Science and Technology Strategic Cooperation Promotion Programs sponsored by the Special Coordination Funds for Promoting Science and Technology, MEXT for 3 years from 2010 to 2013, and Grants-in-Aid for Scientific Research (21256003, 24256002) to Akira Ito. We sincerely thank Dr. Christine Budke for her crucial comments and amendment of the manuscript.
Notes
We have no conflict of interest related to this study.
