Extracorporeal Worm Extraction of Diphyllobothrium nihonkaiense with Amidotrizoic Acid in a Child
Article information
Abstract
Infection cases of diphyllobothriid tapeworms are not much in the below teen-age group. We report a case of Diphyllobothrium nihonkaiense infection in a 13-year-old boy. He presented with severe fatigue, occasional abdominal pain at night time. He also had several episodes of tapeworm segment discharge in his stools. By his past history, he had frequently eaten raw fish including salmon and trout with his families. Numerous eggs of diphyllobothriid tapeworm were detected in the fecal examination. We introduced amidotrizoic acid as a cathartic agent through nasogastroduodenal tube and let nearly whole length (4.75 m) of D. nihonkaiense be excreted through his anus. After a single dose of praziquantel, the child's stool showed no further eggs, and his symptoms disappeared. The evacuated worm was identified as D. nihonkaiense by mitochondrial cox1 gene analysis. Here we report a successful extracorporeal worm extraction from an infection case of D. nihonkaiense by the injection of amidotrizoic acid.
INTRODUCTION
Diphyllobothrium spp. are known to distribute in Northwest Europe and East Asia. Eighteen species in Diphyllobothrium have been reported to cause diphyllobothriasis in humans [1]. Human can contract with these tapeworms by eating the intermediate or paratenic (transport) fish hosts infected with plerocercoid larvae. Among them, Diphyllobothrium latum and Diphyllobothrium nihonkaiense have been mainly reported in Korea [2,3,4,5]. These 2 species appear to have similar morphologic features, and so it is difficult that clinicians distinguish these 2 worms with naked eyes. Nucleotide sequencing analysis studies can identify these species [3,6].
In 1919, Diphyllobothrium infection was first reported in 2 stool egg-positive residents in Jinju, Korea [7]. After then, a small number of sporadic cases have been reported. Recently, a study for molecular identification of D. nihonkaiense collected from 62 patients was reported in 2009 [3]. Among them, only 2 cases of children's D. nihonkaiense infection have been reported in Korea and the age of those were 6 and 13 years old each [3].
In Japan, 2 cases of D. nihonkaiense ejected by administration of intraduodenal amidotrizoic acid were reported in adults [8,9]. However, there has been no pediatric case report concerning extracorporeal whole body evacuation of this worm with this medicine in Korea. In that sense, our case report had focused on the extracoporeal extraction of the worm and measuring the total length of the tapeworm. We report here a case of evacuation of the whole length of D. nihonkaiense by using amidotrizoic acid.
CASE RECORD
A 13-year-old boy, who resides in Gapyeong, Gyeonggi-do was referred from another hospital. He and his family often ate various raw fish including salmon and trout, approximately 5 times a month. Three months before this visit, he noticed a whitish long flat parasite of about 70 cm in length out from the anus while he felt something inside a stool. Then, he took 1 tablet of albendazole. However, after a month, exactly 2 months before visiting our hospital, he experienced the same event of fecal discharge of segments of the parasite and he took mebendazole. Though, the worm came out again, the parents took him to the Department of Pediatrics, Hanyang University Hospital. He presented with fatigue and experienced several episodes of cramping abdominal pain at night. There was no weight gain during the 3 months' ill period. He looked thin, with height of 161 cm (50-75 percentile) and weight of 46.4 kg (25-50 percentile). In addition, he had no travel history to a foreign country within the past several months.
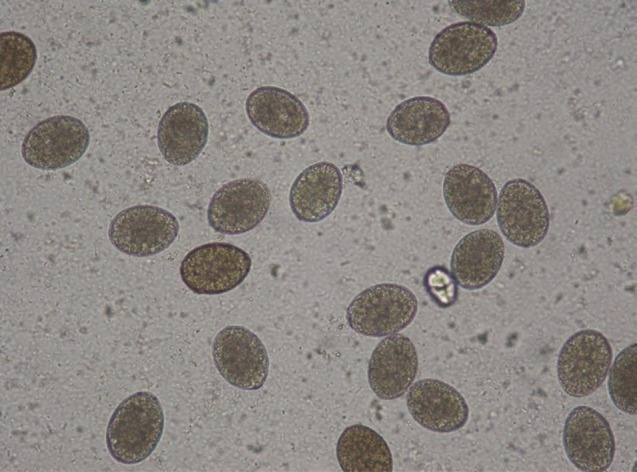
The eggs obtained from the feces were oval and brown in color. The eggs were approximately 59.7±2.3×43.8±1.4 µm in size (Fig. 1). When we confirmed eggs of Diphyllobothrium sp. from his stool, we recommended to perform a cathartic evacuation of the total length of Diphyllobothrium sp.
After his hospitalizations, blood chemistry, serology, and stool examination were done. CBC was in normal range without signs of anemia and eosinophilia (WBC 4,500/µl, total eosinophil count 150/mm3, Hb 15.2 g/dl, Hct 42.9%, MCV 81.9 fL, MCH 29.0 pg, and platelet 181,000/µl). Other blood biochemistry and serology tests were all within normal ranges (vitamin B12 459 pg/ml, folate 8.9 ng/ml, iron 99 µg/dl, and ferritin 68 ng/ml). We also performed gastrofiberscopy and colonoscopy to confirm Diphyllobothrium sp. There was no visible strobila of Diphyllobothrium sp. in the proximal duodenum and colon and no other specific findings.
On the next day, small bowel series using amidotrizoic acid (Gastrografin) was performed for diagnostic and therapeutic purposes. A nasogastroduodenal tube was inserted and its tip was advanced into the second portion of the duodenum by using a guidewire. Amidotrizoic acid of 200 ml was injected into the duodenum via a nasogastroduodenal tube to confirm and eject this tapeworm. However, there was no visible definite tapeworm in the small bowel series. After administration of an additional 200 ml of amidotrizoic acid, this examination ended up. Several hours later he felt something came out from the anus. Then, we observed Diphyllobothrium sp. coming out from his anus and carefully pulled it through the anus. However, he complained of abdominal pain during this work. It was impossible to remove it completely and the tapeworm cut its body by itself. The total length of the worm which was excreted extracorporeally (at initial trial) was about 475 cm. Fig. 2 shows the strobila of Diphyllobothrium sp. which was pushed out from the body by amidotrizoic acid injected into the duodenum. Unfortunately, however, the scolex was not detected. Another small segment of about 1 m long was also passed out in a few hours. The patient was administered with a single dose of praziquantel (15 mg/kg, 600 mg) in the evening.
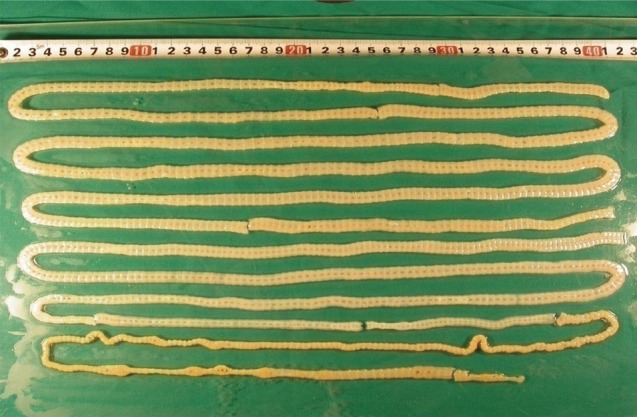
A whole strobila without scolex of D. nihonkaiense extracorporeally discharged by the injection of amidotrizoic acid. The total length of the specimens was about 475 cm.
On the next day, he was discharged without any complications. After 2 weeks, he visited our out-patient clinic, and the follow-up stool was free of any eggs. There was no evidence of recurrent Diphyllobothrium sp. infection after the treatment, and he looked healthy.
Later, the specimen was sent to the Department of Parasitology and Tropical Medicine, Kyungpook National University School of Medicine for genetic analysis of species as described by Song et al. [8]. Total genomic DNA was extracted from the specimen and analyzed by nucleotide sequences of mitochondrial cytochrome c oxidase subunit 1 (cox1) gene. The cox1 sequences (858 bp) of the worm showed similarity of 99.8% (856/858 bp) with D. nihonkaiense (GenBank no. AB781787).
DISCUSSION
D. nihonkaiense is known to distribute in Northwestern Europe and East Asia. Consumption of raw or uncooked fish leads to human infections with D. nihonkaiense. The intermediate hosts of D. nihonkaiense are salmons such as Oncorhynchus masou (cherry salmon), O. gorbuscha (pink salmon), and O. keta (chum salmon) available in the Pacific Ocean [10]. On the other hand, the intermediate hosts of D. latum are freshwater fish, such as the pike, perch, burbot, trout, and salmon [11].
The first worm proven as D. nihonkaiense was described in 1986 in Japan [12], this worm had been mostly known as D. latum in Korea [2]. In 2009, a study for genetic identification was performed against the "so-called" D. latum worms that were reported in Korea, and a total of 62 cases were first proved to be caused by D. nihonkaiense [3]. Recently, additional 3 cases of D. nihonkaiense have been reported [4,5]. However, children's cases of D. nihonkaiense are quite few in Korea. Four cases of children's D. latum and 2 cases of children's D. nihonkaiense have been reported in Korea [2,3].
In the past study, most of the cases of D. nihonkaiense infection had a few symptoms. The major symptoms of D. nihonkaiense infections were gastrointestinal problems such as abdominal pain, abdominal distension, vomiting, and diarrhea. In other cases, the symptoms such as anemia, fatigue, anorexia, fever, and myalgia were observed. In our case, the patient complained the colicky abdominal pain and fatigue.
In recent several cases, colonoscopy and capsule endoscopy were useful diagnostic methods for detecting D. latum and D. nihonkaiense infections [13,14,15,16]. However, in our case, D. nihonkaiense infection could not be detected by colonoscopy.
It remains unclear how amidotrizoic acid evacuates the tapeworm and how the scolex of tapeworm is detached from the intestinal surface though [17]. It is most possible that the polysorbate 80 in amidotrizoic acid is a hypertonic solution and has the effects of laxatives; therefore, it may play a role in evacuation of this tapeworm [18]. When amidotrizoic acid rapidly passed through the small intestine, the tapeworm was expelled from the small intestine to the colon by intestinal peristalsis. The advantage of this method is complete evacuation of tapeworms. Several studies in Japan reported that the body and scolex of tapeworms were ejected by administration of amidotrizoic acid [8,9]. In domestic cases, there was no report concerning the evacuation of whole tapeworm by using a cathartic agent like amidotrizoic acid through the duodenal tube. In that sense, the method for evacuation of tapeworm by using amidotrizoic acid in our case is thought to be one of the available methods to remove the whole body of D. nihonkaiense.
The medications such as atabrine, niclosamide, and bithionol have been used for treatment of Diphyllobothrium infections since 1971 [2]. However, from 1987 till present days, praziquantel has been used as the drug of choice. Tapeworms are completely removed by praziquantel and treatment failure cases were not reported [2]. In our case, the treatment with a single dose of praziquantel was effective as proved by the disappearance of eggs in the feces in 2 months. Through the nasoduodenal injection of amidotrizoic acid and extracorporeal acquisition of the worm, it could be possible for us to confirm what the worm was and how long it was, and to document the worm by a gene study.
ACKNOWLEDGMENTS
The authors thank Ms. Soo-Young Lee for her assistance in sample preparation.
Notes
We have no conflict of interest related to this work.