Visceral Leishmaniasis in Rural Areas of Alborz Province of Iran and Implication to Health Policy
Article information
Abstract
Visceral leishmaniasis (VL) or kala-azar mainly affects children in endemic areas. This study was conducted to determine the seroprevalence of VL using direct agglutination test (DAT) in children living in rural districts of Alborz Province located 30 km from Tehran capital city of Iran. Multi-stage cluster random sampling was applied. Blood samples were randomly collected from 1,007 children under 10 years of age in the clusters. A total of 37 (3.7%) of the studied population showed anti-Leishmania infantum antibodies with titers of ≥1:800. There was a significant association between positive sera and various parts of the rural areas of Alborz Province (P<0.002). Two children with anti-Leishmania infantum antibodies titers of ≥1:3,200 indicated kala-azar clinical features and treated with anti-leishmaniasis drugs in pediatric hospital. The findings of this study indicated that Leishmania infection is prevalent in rural areas of Alborz Province. Therefore, it is necessary to increase the awareness and alertness among physicians and public health managers, particularly in high-risk rural areas of the province in Iran.
INTRODUCTION
Visceral leishmaniasis (VL) or kala-azar is caused by various species of Leishmania donovani complex, and children are particularly most affected by this infection in endemic areas [1]. VL is distributed in 98 countries and 3 territories and approximately 200,000 to 400,000 cases of new types of human VL occur around the world annually [2]. Mediterranean or zoonotic VL is a form of VL found in Iran. In this type, VL, Leishmania infantum is transmitted from animals, mainly dogs, to humans by vectors [3].
VL is endemic in some parts of Iran including northwest (Ardebil and East Azerbaijan Provinces) and southwest (Fars and Bushehr Provinces) [4]. Currently, the endemic foci of this disease are spreading across other areas of Iran. Since 1949 to 2012, more than 6,000 cases of VL had been reported throughout Iran [4]. Domestic and wild canines with VL infection are considered to be the main reservoir hosts of Mediterranean VL in Iran [5]. Sandflies such as Phlebotomus major, Phlebotomus kandelakii, and Phlebotomus tobbi are the most important vectors of L. infantum protozoa in different parts of Iran [6].
Alborz Province is located in the south of Alborz Mountains, 30 km from Tehran, the capital city of Iran and has been considered as a touristic area because of its natural attraction. This province is 1,320 m above the sea level. Livestock and stray and domestic dogs are found in rural areas of the province. Two retrospective studies have reported 21 VL cases in children 6-92 months of age referred to Tehran Pediatric Medical Center Hospital belonged to Alborz Province between 1991 and 2011 [7,8]. However, there is no information on the prevalence of visceral Leishmania infection in various parts of Alborz Province, because most people infected by Leishmania parasites will remain asymptomatic and a very small fraction (around 10%) will develop the disease depending on predisposing factors. Therefore, in the present study, we conducted a seroepidemiological investigation of Leishmania infections in rural districts of Alborz Province.
Direct agglutination test (DAT) is a suitable serological test for the screening of Leishmania infection in field studies [9] and has been validated in most of the endemic areas [10,11]. Owing to the prevalence of Mediterranean visceral Leishmania infection in Iran and the fact that children are mostly affected by this infection, children were included in the present study. The aim of this study was to determine the seroprevalence of visceral Leishmania infection using DAT in children under 10 years of age in rural districts of Alborz Province, Iran.
MATERIALS AND METHODS
Study area
Alborz Province is located in the south slope of Alborz Mountains of Iran (Fig. 1), and has a population of approximately 2,412,510. It has a moderate weather, and its rural population is settled in 4 districts, including Savojbolagh, Nazar Abad, Chalous road, and Mahdasht/Eshtehard. The province has an area of approximately 5,122 km2 [12]. The study was conducted from March 2013 to June 2014.
Multi-stage cluster random sampling was applied for sample selection. A total of 50 villages (clusters) were selected from approximately 100 villages. Blood samples were randomly collected from 1,007 children under 10 years of age in the clusters. Approximately 200 µl of blood samples were collected from each child using an automatic lancet and heparinized hematocrit tubes. The capillary tubes containing the blood samples were centrifuged at 800 g for 5-10 min, and the obtained sera were stored at -70˚C. All the serum samples were analyzed using DAT in the Leishmaniasis Laboratory, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran. Also, a demographic questionnaire was used and various data, including age, sex, and place of residence were recorded.
Direct agglutination test
The DAT antigen was prepared in the Parasitology Department, School of Health, Tehran University of Medical Sciences. The antigen was obtained via multi-stage procedure, which included mass production of promastigotes of the Iranian strain of L. infantum [MCAN/IR/07/Moheb-gh (GenBank accession no. FJ555210)] in RPMI-1640 medium (Biosera, South America) plus 10% fetal calf serum (Biosera, South America), following trypsinization of the parasites, staining with Coomassie brilliant blue R-250 (Sigma, St. Louis, Missouri, USA) and fixing with 1.2% formaldehyde [13].
The serum samples were diluted with 0.9% saline and 0.78% 2-mercaptoethanol at the ratio of 1:10-1:3,200 in a V-shaped microtiter plate. Then, 50 µl of the antigen suspension was transferred to each well. Negative and positive controls were used in each plate. The cut-off titer was determined after 18-24 hr of incubation in a wet room at room temperature. The cut-off titer of the sample was determined as the highest dilution at which visible agglutination occurred, when compared with the positive and negative control titres. Compact blue dots and large diffuse blue mats indicated the negative and positive samples, respectively. The cut-off titer was defined as ≥1:800 for Leishmania infection, in accordance with the previous study [14]. The seropositive children were referred to a pediatric infectious disease specialist for further clinical examinations. SPSS software ver.16 (SPSS Inc, Chicago, Illinois, USA) was used for data analysis. The chi-square and Fisher’s exact tests with confidence level of 95% were used to compare seroprevalence values relative to sex, geographical zones, and nationality. Frequency data were illustrated by number and percent within 95% confidence interval (CI).
Ethical considerations
Informed written consent was obtained from the parents of the children examined. This study was approved by the Research Ethical Review Committee of Alborz University of Medical Sciences, Karaj, Iran.
RESULTS
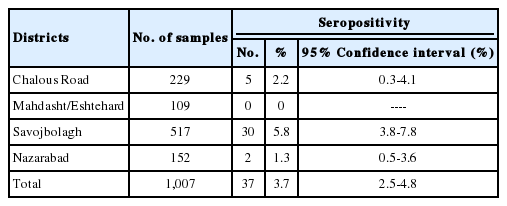
Among the total 1,007 children examined, 37 (3.7%) were positive for the specific antibody against Leishmania infection (Table 1). The findings of Leishmania seroprevalence in subjects in the 4 rural districts of the study area are indicated in Table 2. The seropositive rate was significantly different between the districts (P<0.002).
Seroprevalence of human visceral Leishmania infection by direct agglutination test in rural districts of Alborz Province, Iran in 2013
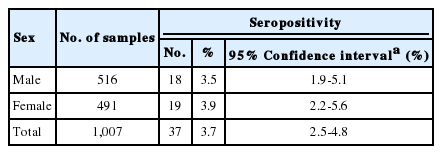
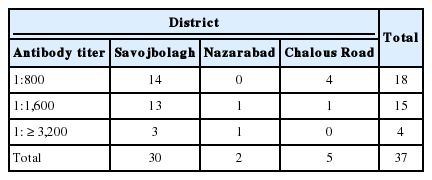
Among the 1,007 children, 516 (51.2%) were boys and 491 (48.8%) were girls (Table 3). Most of the children (79.2%) were Iranian, while 207 (20.6%) were Afghani and 2 (0.2%) had other nationalities. However, 20 (54.1%) and 17 (46.0%) children with anti-Leishmania antibodies titers of ≥1:800 were Iranian and Afghan nationals, respectively. These findings indicated a significant association between nationality and the rate of positive sera against Leishmania infection (P<0.002). However, no association between sex and titer of antibodies against Leishmania was noted. Two children with anti-L. infantum antibodies titers of ≥1:3,200 indicated kala-azar clinical manifestation and hospitalized in a pediatric hospital. Leishmania parasites were demonstrated in their bone marrow aspirations and both of them were successfully treated with anti-leishmanial drugs.
DISCUSSION
The present study is the first that examined the seroprevalence of Leishmania in rural areas of Alborz Province in Iran. Findings of this study indicated that, in 2013, approximately 3.2% of the randomly selected subjects had antibody titers of ≥ 1:800 against Leishmania infection. This rate of Leishmania infection was higher than that reported earlier using DAT among children in Baft, Kerman Province (2.5%) in south of Iran [15]. Similarly, the rate of Leishmania infection noted in the present study was also higher than those reported in Bojnord Khorasan Province (2.4%) and Germi, Ardebile Province (2.8%) of Iran [16,17]. Meanwhile, some studies reported that the Leishmania infection rates among subjects with antibody titer of ≥1:3,200 were 0.56%, 0.6%, and 3.1%, in 3 areas of Iran including Bojnord, Germi, and Booyerahmad, respectively [16-18] which are higher than findings of our study (0.4%). However, the study of Hamzavi et al. [19] demonstrated 0.33% Leishmania seropositive population at titers of ≥ 1:3,200 in Kermanshah Province in the west of Iran, which was nearly similar to ours.
It should be noted that it is not possible to differentiate the symptomatic disease, asymptomatic disease, and past infection using DAT [9]. In the present study, all of the individuals with anti-Leishmania antibody titers of ≥1:800 were assessed by a physician, and 2 of the 4 children (50%) from Nazarbad and Savojblagh with anti-Leishmania antibody of titers ≥1:3,200 indicated clinical manifestation of VL. Bone marrow aspirations were positive in both of them. Their age was 1.5 and 4.5 years, respectively. In a seroprevalence study conducted in 5 parts of Iran from 2002 to 2012, almost 75% individuals with anti-Leishmania antibody titers of ≥1:3,200 in an endemic area exhibited clinical signs and symptoms [4].
In Iran and elsewhere in the world, Leishmania infection has been noted to produce a wide range of clinical conditions from asymptomatic to fatal cases. In the present study, the majority of the seropositive cases presented no clinical symptoms and were considered as asymptomatic cases. The asymptomatic form of Leishmania infection has also been reported as the predominant form of Leishmania infection in other parts of Iran [4,19], as well as in India, Turkey, Croatia, and Brazil [20-23]. Although this form of Leishmania infection does not require treatment, longitudinal follow-up studies have indicated that some cases eventually develop clinical VL, but most will never develop the disease [1]. Fever, weakness, paleness, loss of appetite, weight loss, splenomegaly, hepatomegaly, and features of anemia were observed in 2 clinical cases of kala-azar in the present study. These clinical features were similar to findings of other studies conducted in the Mediterranean region [5,24-26]. Hematological findings including thrombocytopenia, leukopenia, and anemia were recorded, and both of them were hospitalized and treated successfully with antimonial drugs. In the present study, despite the occurrence of few signs and symptoms such as fever, anemia, and weight loss in 5, 9, and 2 other children with anti-Leishmania antibodies, during the follow-up examination for 15 months, none of them showed any progressive VL clinical signs. For better evaluation of these kinds of subjects, follow-up studies should be continued. Furthermore, no association was found between Leishmania infection and gender. This finding was in agreement with those reported in other parts of Iran [18,19].
Two retrospective studies have reported 21 VL cases in children 6-92 months of age referred to Tehran Pediatric Medical Center Hospital belonged to Alborz Province between 1991 and 2011 [7,8]. Another study on dogs using DAT showed that 3.6% (12/337) of the owned and stray dogs had VL infection [27]. In a recent study on Savojbolagh L. infantum, the major causative agent of leishmaniasis in Iran isolated from P. tobbi [6]. It seems that dogs with Leishmania infection as the main reservoir of Leishmania and the presence of various Phlebotomus species as the vectors of the infection in these areas have provided appropriate conditions for Leishmania transmission to humans. However, further studies on the reservoirs and vectors of Leishmania are required.
In the present study, most of the seropositive children belonged to Savojbolagh and Chalous road, respectively, implying that these areas have more suitable conditions for Leishmania transmission, where farming, livestock, and domestic and wild dogs are more prevalent than the other parts of the province. Alborz Province is one of the areas with more migrants and tourists owing to its close proximity to the capital city Tehran as well as appropriate climate. The emergence of visceral Leishmania infection in the province underlines the need for health and therapeutic achievements for prevention, diagnosis, and treatment of this disease. Furthermore, it is necessary to increase the awareness and alertness among physicians and public health managers, particularly in high-risk rural areas of the province.
It is important that eventually most of visceral leishmaniasis cases become fatal without treatment, but in the present study DAT successfully identified 2 children with clinical features of kala-azar. In conclusion, the findings of our study indicated that visceral Leishmania infection is prevalent in rural areas of Alborz Province, and DAT could be implicated to the health policy of the area for more precise control and treatment of VL cases.
Acknowledgements
This study was financially supported by Alborz University of Medical Sciences, Karaj, Iran and Tehran University of Medical Sciences, Tehran, Iran (project no. 17402). The authors are also grateful to Mrs. Moshki for her contribution to sampling. We would like to thank those individuals from the rural regions of Alborz Province who kindly contributed to this study.
Notes
We declare that we have no conflict of interest.