Two Human Cases of Echinococcus ortleppi Infection in the Lung and Heart in Vietnam
Article information
Abstract
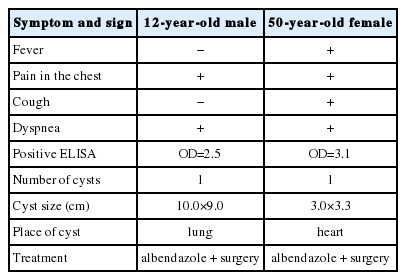
This is a report of 2 cases of human hydatidosis caused by Echinococcus ortleppi in Vietnam. The patients were a 12-year-old male (case 1) having a cyst of 10.0×9.0 cm size in the lung and a 50-year-old female with a 3.0×3.3 cm-sized cyst in the heart. Eosinophilia was 33.7% in the male and 45.8% in the female patient. C-reactive protein was increased to 16.5 mg/L in the male and 18.2 mg/L in the female. Both patients were positive for ELISA at OD=2.5 and 3.1, respectively. Echinococcus protoscolices were collected from the cysts by amniocentesis and surgery. The protoscolices were identified as E. ortleppi by morphology and analysis of mitochondrial NADH dehydrogenase 1 (nad1) gene sequence. Both patients were cured by surgical resection of the hydatid cyst combined with albendazole medication. The E. ortleppi infection in lung is the second report, and the other in the heart is the first in Vietnam.
INTRODUCTION
Family Taeniidae consists of 2 genera, Echinococcus and Taenia [1]. Echinococcosis is an important zoonosis caused by tapeworms of the genus Echinococcus. Human echinococcosis continues to be a substantial cause of morbidity and mortality in many parts of the world [2–5]. Human echinococcosis occurs in 4 forms: cystic echinococcosis (CE), also known as hydatid disease or hydatidosis, caused by infection with the species complex of Echinococcus granulosus; alveolar echinococcosis (AE) caused by infection with Echinococcus multilocularis; and 2 forms of neotropical echinococcosis (NE), including polycystic disease caused by Echinococcus vogeli and unicystic disease caused by Echinococcus oligarthrus [6]. The adult stage develops in the small intestine of carnivores, and the larval stage develops in the viscera of a variety of mammalian species, including humans.
E. granulosus sensu stricto (G1) and Echinococcus ortleppi (G5) are haplotypes of the parasite formerly known as E. granulosus sensu lato, which in its larval stage causes cystic hydatidosis [7]. Now E. granulosus sensu lato is considered to be a complex of at least 4–5 different species that encompass 10 genotypes [8]. They include E. granulosus sensu stricto (genotypes G1, sheep strain; G2, Tasmanian sheep strain; G3, buffalo strain), Echinococcus equinus (G4, horse strain), E. ortleppi (G5, cattle strain), and Echinococcus canadensis (G6, camel strain; G7, pig strain; G8 & G10, cervid strain) [7,8]. Humans or animals can be infected with the larval form (echinococcosis) in various organs; humans are incidentally infected [2–4]. Growing cysts may damage surrounding tissues, including blood vessels [4].
Of the 4 forms of echinococcosis, CE caused by the species complex of E. granulosus, including E. ortleppi, and AE by E. multilocularis are highly important [9,10]. CE occurs worldwide, whereas AE is restricted to the northern hemisphere. Two forms of NE have been identified in Central and South Americas [11]. Any associated clinical problems are dependent upon the number of cysts, their size, location, and the rate of growth. The organs most frequently affected are the liver and lungs, in approximately 65% and 25% of the cases, respectively [8], but may also be the kidneys, spleen, brain, heart, skeletal system, and musculature. Cysts are detected by ultrasound, X-ray, computed tomography (CT), magnetic resonance imaging (MRI), or other imaging techniques. Anti-echinococcal antibodies can be detected by serological tests, including indirect fluorescent antibody test, complement fixation test, ELISA, Western blot, and other techniques [12].
Echinococcosis is distributed almost worldwide and especially common in such areas as Australia, Tasmania, New Zealand, southern and northern Africa, and South America [13], and also in some other regions, such as Central America, the Middle East, China, Italy, Spain, Greece, Russia, and the western US (Arizona, New Mexico, and California) [2]. In Italy, chest X-rays and lung images were described in 24 (85.7%) of 28 confirmed patients most of which were with hepatic localization (96%) [5]. In Asia, echinococcosis has been reported in Japan, China, South Korea, Mongolia, Thailand, Indonesia, Bangladesh, and India [14]. High prevalences of CE have been recorded from South America, Northern and Eastern Africa, Eurasia, and Australia [15]. In Vietnam, the first report of human echinococcosis due to E. ortleppi involving 2 cases was published in 2017 [16]. In the present study, we report 2 additional cases of human E. ortleppi infection in Vietnam; one patient had a cyst in the lung and the other had a cyst in the heart.
CASE RECORD
Case 1
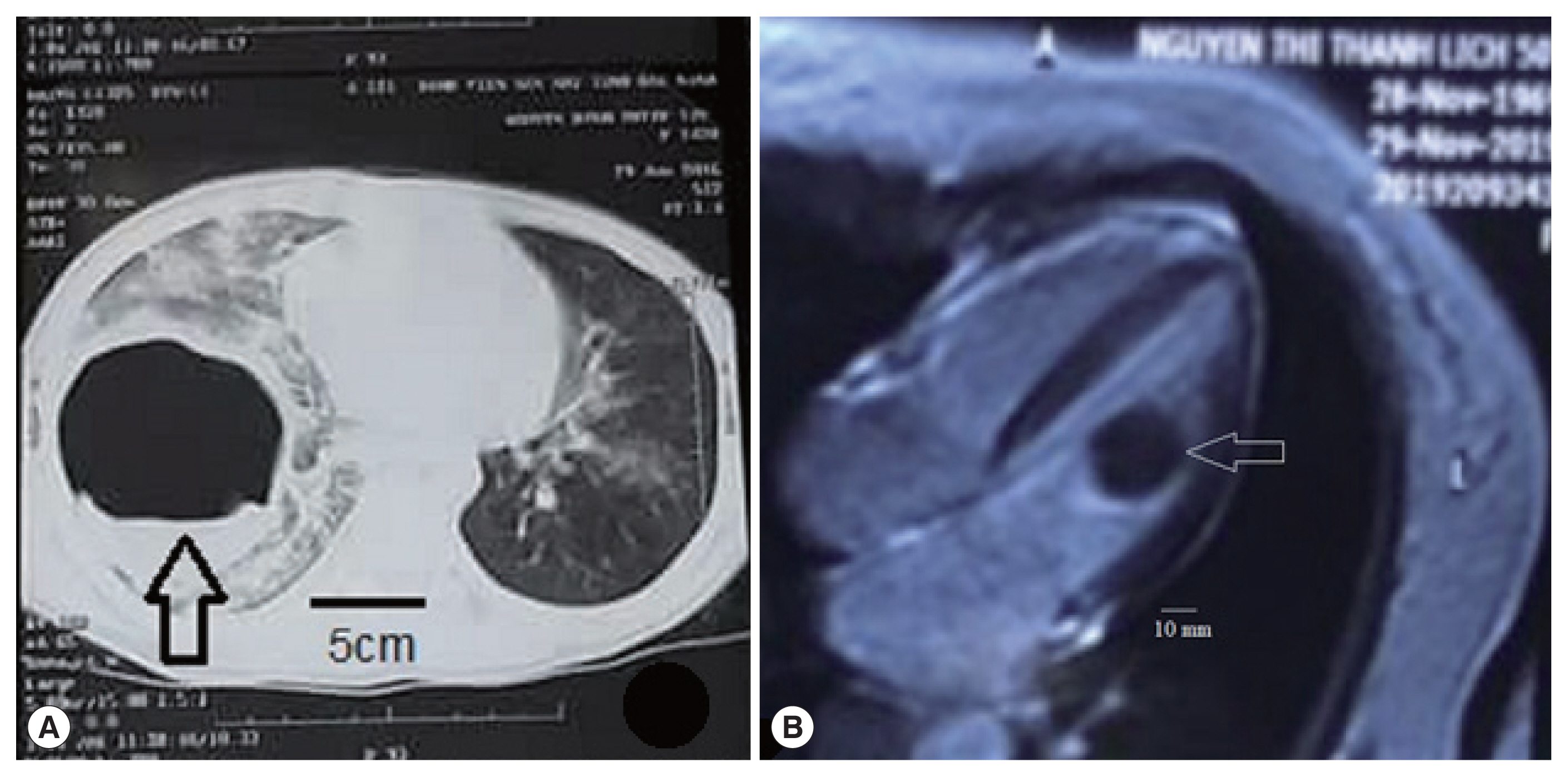
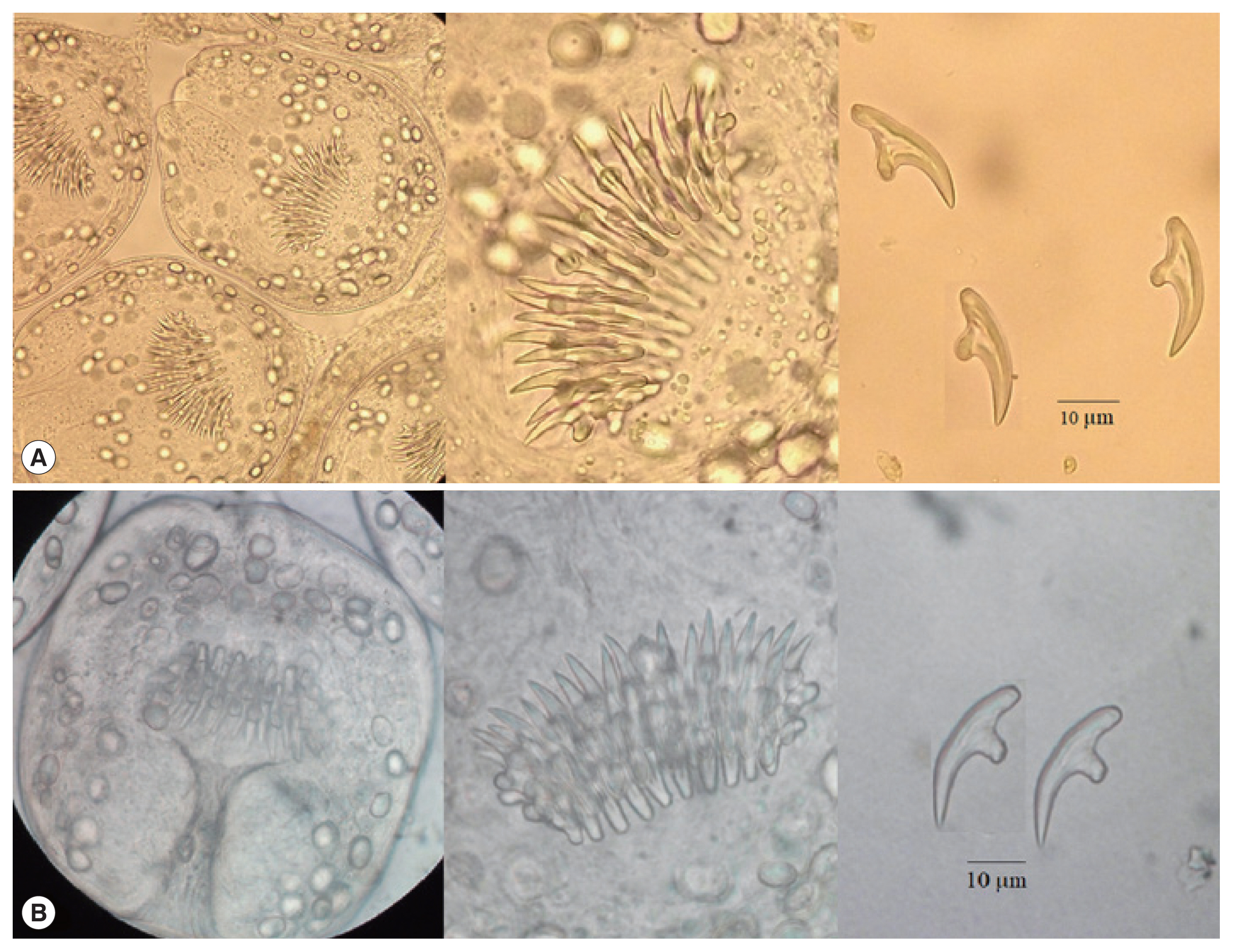
The patient was a 12-year-old male residing in Bac Ninh Province of Delta in north Vietnam. He was a schoolboy and had lived in his hometown. He complained of chest pain in the right side in January 2019, and the severity of this symptom increased for 1 month. He visited the National Hospital of Pediatrics in Hanoi, Vietnam. The main clinical symptoms were chest pain and dyspnea, without fever and cough (Table 1). In chest MRI, a big nodular shadow circle, 9.0×10.0 cm in size, was found with equal density in the left lobe of the lung (Fig. 1A). ELISA was positive for Echinococcus antigen (OD=2.5/0.3). Several hematological and biochemical values were increased; WBC of 12,000 cells/mm3, eosinophilia of 33.7%, and C-reactive protein (CRP) of 16.5 mmol/L (Table 2). The larvae (protoscolices) were collected from the cyst by amniocentesis (Fig. 2A). He was treated by surgery combined with albendazole medication at the dose of 400 mg×2 times/day for 2 months, and recovered after the treatment.
Case 2
The patient was a 50-year-old female residing in Phu Tho Province of mountainous north Vietnam. She was a farmer and had lived in her hometown. She felt chest pain in the left side in October 2019 and visited the Bach Mai Hospital for examination. Her main clinical symptoms and signs were chest pain in the left side, dyspnea, fever of 38.5°C, and severe cough (Table 1). In chest MRI, a nodular shadow (circle), 3.0×3.3 cm in size with equal density, was found in the left ventricle of the heart (Fig. 1B). ELISA was positive for Echinococcus antigen (OD=3.1/0.3). Some hematology and biochemistry titers were increased; WBC 15,000 cells/mm3, eosinophilia 45.8%, and CRP 18.2 mg/L (Table 2). The cystic fluid was collected by amniocentesis, and the protoscolices were found under microscopy (Fig. 2B). She was treated by surgery combined with albendazole 400 mg×2 times/day for 2 months, and cured after the treatment.
Molecular analysis of protoscolices from the cystic fluid
The cyst (hydatid cyst) surgically excised contained numerous protoscolices, each of which had hooklets (Fig. 2A, B). The protoscolices had a spherical body of about 0.16×0.14 mm in size with an invaginated scolex armed with 30 hooklets; each hooklet was 21 μm in its longest diameter (Fig. 2A, B). These protoscolices were identified as E. ortleppi by a molecular method using mitochondrial NADH hydrogenase 1 (nad1) with 99–100% homology compared with E. ortleppi in GenBank; however, the homology with E. granulosus was only 93–94% (Table 3). The phylogenetic tree of E. ortleppi Vietnam isolates and other strains constructed from partial nad1 sequences by the neighbor-joining (NJ) method using the MEGA5.1 program employing Tamura-nei model of nucleotide substitution with 1,000 bootstrap replications showed that the present isolates of Vietnamese E. ortleppi (Eorvn1 and Eorvn2) are one group with other geographical isolates of E. ortleppi available in GenBank (from The Netherlands, Sudan, and an unknown country) (Fig. 3).
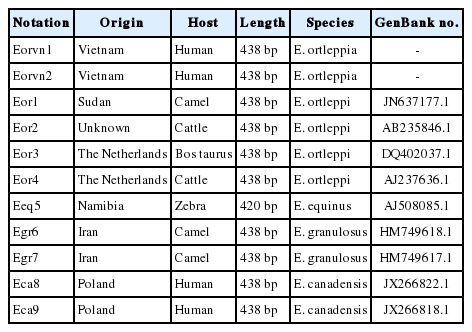
Sequencing of mitochondrial NADH dehydrogenase 1 (nad1) gene of different Echinococcus species from GenBank compared with Echinococcus ortleppi from Vietnam
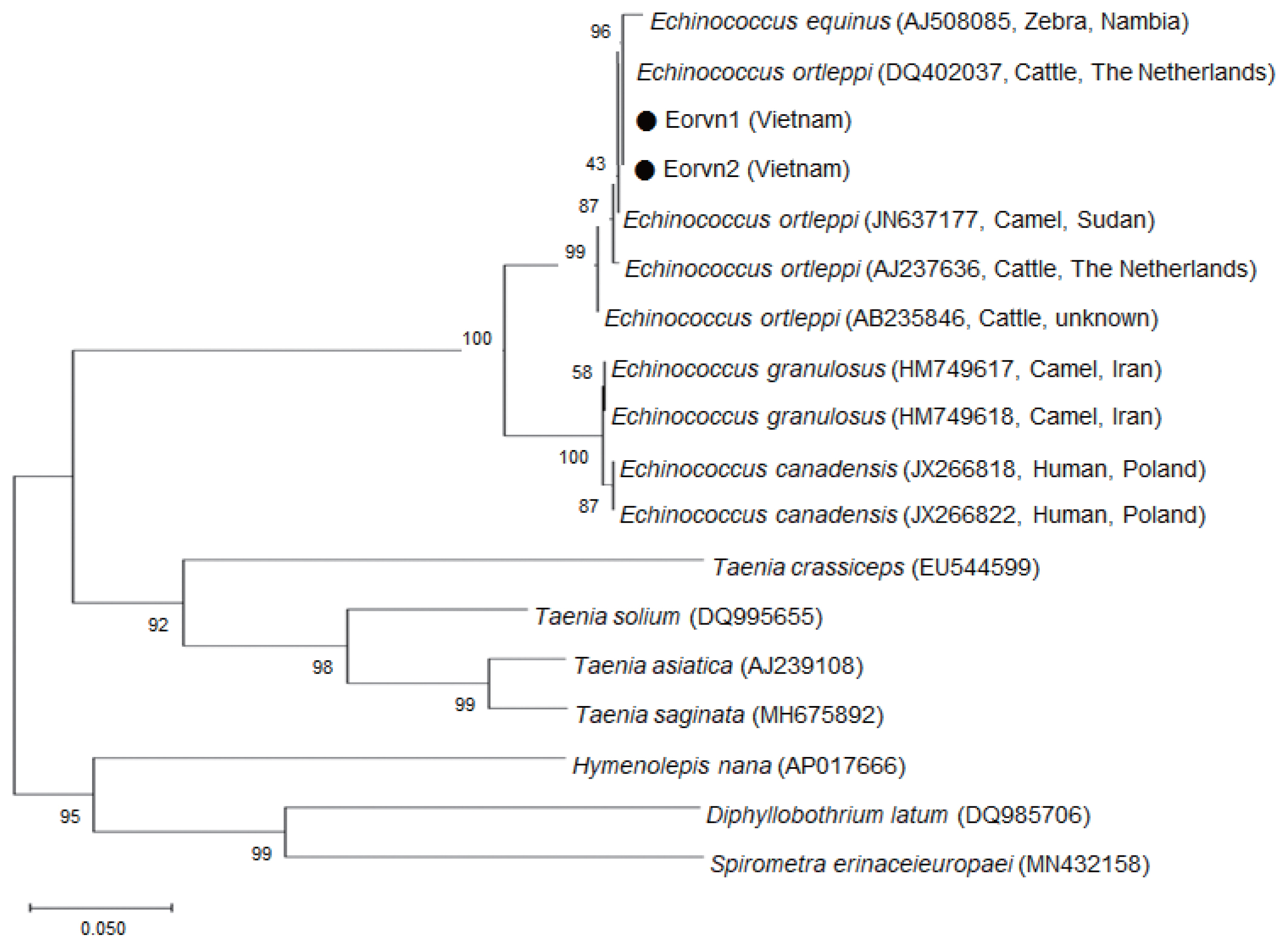
A phylogenetic tree of Echinococcus ortleppi from 2 Vietnamese cases in comparison with reports from other countries based on a part of NADH dehydrogenase 1 (nad1) nucleotide sequences estimated by neighbor-joining method using the MEGA5.1 program. (●), Eorvn1 and Eorvn2, Vietnamese E. ortleppi obtained in this study.
DISCUSSION
The present report of 2 cases of human echinococcosis is based upon the diagnosis of larvae from the surgically excised cysts. MRI clearly showed 1 cyst each, in the lung and the heart, in the 2 patients, respectively. The larval form of E. ortleppi was detected from bovines (cattle and buffaloes) in Italy in 2008 [7] and also in Southern Brazil in 2012 [6]. The geographical distribution of E. ortleppi is extended from Africa, to Central and South America, Central Europe, and Asia [7]. Human E. ortleppi infection has been detected in Brazil [10], France [8], Poland [12], Chile [13], and China [14]. Animal E. granulosus hydatid cysts are usually found in the liver or lungs of cattle, but E. ortleppi cysts are found in the lungs of cattle [17]. Animal E. ortleppi infection was also detected in one-humped camels in Sudan [15] and crested porcupines in Bosnia and Herzegovina [18].
Echinococcosis is very rare in Vietnam, and recent years, some cases were suspected as echinococcosis with watery cysts in the liver by ultrasound; however, no larvae or hooklets were collected in the cystic fluid [19]. In Vietnam, human cystic hydatidosis due to E. ortleppi infection was reported for the first time in 2017 with 2 cases, including a 42-year-old male and a 48-year-old female, both in the lungs with a single cyst of 6.0×7.0 cm in size and 4 cysts of 5.0×6.0, 4.0×4.0, 3.5×3.0, and 2.5×2.0 cm in size, respectively [16].
Animal E. ortleppi infection was first detected in red-shanked douc langurs in Vietnam [20]. In addition, in Southern Vietnam, Hoa and Tan [21] reported dogs (the reservoir host) infected with E. granulosus in 1967. In the present study, we detected 2 E. ortleppi patients treated with surgery combined with albendazole medication, 400 mg/kg×2 times/day for 60 days, and both patients were cured. The mode of infection in these patients is unknown.
Dehkordi et al. [22] showed that the treatment of hydatid cysts with albendazole may be associated with the prevention of recurrence and reduction of the size and death of the hydatid cysts. The treatment is multimodal, including surgery and medication; albendazole has a central role in the medical therapy of this disease [23]. Both albendazole and mebendazole have favorable effects in patients suffering from multi-organ and multi-cystic diseases, particularly in inoperable primary liver or lung cases, and these medications can also prevent secondary echinococcosis; the best efficacy of medication is observed with the liver, lung, and peritoneal cysts [24]. Albendazole 400 mg twice a day, in 3 cycles of 6 weeks with 2 weeks between cycles could cure 80% (18/22) of the cases [25], whereas surgery remains the mainstay of the treatment for large, active, complicated, or symptomatic hepatic hydatid cysts [26]. Termed puncture, aspiration, injection, and re-aspiration (PAIR) of hydatid cysts combined with chemotherapy with albendazole or mebendazole may also be applied [27].
In conclusion, 2 human cases with E. ortleppi infection in the lung and heart each have been diagnosed morphologically and molecularly in Vietnam. Both patients were cured by surgery combined with albendazole treatment. In Vietnam, human E. ortleppi infection in the lung is the second report, and the cyst in the heart is the first one.
ACKNOWLEDGMENTS
This research was funded by Vietnam National Foundation for Science and Technology Development (NAFOSTED) under a grant no. 106-YS.05-2014.08, and collaborated with the National Hospital of Pediatrics and Bach Mai Hospital, Hanoi, Vietnam.
Notes
CONFLICT OF INTEREST
We have no conflict of interest related to this work.