Reemerging vivax malaria: changing patterns of annual incidence and control programs in the Republic of Korea
Article information
Abstract
Changing patterns of the reemerging Plasmodium vivax malaria in the Republic of Korea (South Korea) during the period 1993 to 2005 are briefly analyzed with emphasis on the control measures used and the effects of meteorological and entomological factors. Data were obtained from the Communicable Diseases Monthly Reports published by the Korea Center for Disease Control and Prevention, and webpages of World Health Organization and United Nations. Meteorological data of Kangwon-do (Province) were obtained from local weather stations. After its first reemergence in 1993, the prevalence of malaria increased exponentially, peaking in 2000, and then decreased. In total, 21,419 cases were reported between 1993 and 2005 in South Korea. In North Korea, a total of 916,225 cases were reported between 1999 and 2004. The occurrence of malaria in high risk areas of South Korea was significantly (P < 0.05) correlated with the mosquito population but not with temperature and rainfall. Control programs, including early case detection and treatment, mass chemoprophylaxis of soldiers, and international financial aids to North Korea for malaria control have been instituted. The situation of the reemerging vivax malaria in the Republic of Korea is remarkably improving during the recent years, at least in part, due to the control activities undertaken in South and North Korea.
INTRODUCTION
Vivax malaria due to Plasmodium vivax, the only naturally occurring human malaria species in the Republic of Korea (hereafter referred to as South Korea), was endemic in South Korea until the late 1970s, when the country became malaria free (Paik et al., 1988; Chai, 1999). In particular, during the Korean War (1950-1953), 15,000 South Korean soldiers and more than 3,000 U.S. soldiers were reported to have contracted vivax malaria (Jones et al., 1953; Chai, 1999). Subsequently, malaria cases rapidly decreased, with the implementation of the National Malaria Eradication Service, which was established jointly by the South Korean government and the World Health Organization (WHO) in 1959 (Ministry of Health and Social Affairs, Republic of Korea, 1966). Consequently, after the 1970s, indigenous malaria cases were almost unheard of, though 2 such cases were reported in 1984 (Soh et al., 1985). During the same period a substantial number of imported malaria cases was reported (Chai, 2002).
However, indigenous vivax malaria reemerged in 1993; a South Korean soldier working at the western edge of the demilitarized zone (DMZ; the border between South and North Korea) in Kyonggi-do (Province), was confirmed to have contracted P. vivax malaria (Chai et al., 1994). Thereafter, the number of malaria cases increased exponentially year by year, peaking in 2000 (Feighner et al., 1998; Chai, 1999; Lee et al., 2002; Park et al., 2003). North Korea, which stated that it was free of malaria from the 1970s, also started reporting cases in 1998 from the northern part of the DMZ bordering South Korea (Chol et al., 2005). Since then, the number of malaria cases in North Korea has increased dramatically and reached around 300,000 in 2001. Therefore, in 1999, the North Korean government developed a national malaria control program in cooperation with WHO, to reduce the malaria burden (Chol et al., 2005).
In South Korea, during the period 1993-1996, the outbreak area was confined to the northern part of Kyonggi-do and northwestern Kangwon-do, near the DMZ (Chai, 1999). However, after 1997, the outbreak area extended in an easterly direction to the northeastern region of Kangwon-do and in a southerly direction in Kyonggi-do (Lee et al., 2002; Park et al., 2003), and it was feared that this southward trend would continue. To cope with this risk, the present national malaria control program was launched in 1997 (Korea Center for Disease Control and Prevention, Republic of Korea, 2002). This program includes early case detection and treatment, chemoprophylaxis of soldiers, vector control, personal protection, and financial aids to North Korea for malaria control.
In addition to control activities, meteorological (temperature and rainfall) and entomological factors (mosquito density) may have significant impacts on malaria transmission. For instance, the incidences of malaria were related to local climatic variables in China (Bi et al., 2003) and Rwanda (Loevinsohn, 1994). However, in South Korea, no published data is available concerning the relations between temperature, rainfall, the population density of the vector mosquitoes, and the incidence of malaria.
The aim of the present paper is to briefly summarize vivax malaria outbreaks over the period 1993 to 2005 in South Korea, and to analyze the efficacies of the control activities implemented since 1997, and the impacts of meteorological and entomological factors on disease occurrence.
MATERIALS AND METHODS
Malaria is designated an important communicable disease and case details must be reported immediately to the Ministry of Health and Welfare in South Korea. In the present study, all cases reported since the first reemergence of indigenous vivax malaria case in 1993 were subjected to analysis. Patients' occupations, i.e., civilians, soldiers on duty, and retired soldiers, were obtained from the Communicable Diseases Information System (http://dis.cdc.go.kr) and from the Communicable Diseases Monthly Reports issued during the study period by the Korea Center for Disease Control and Prevention (KCDC), Ministry of Health and Welfare, South Korea. Information about malaria prevalence in North Korea and financial support for malaria control was obtained from the KCDC, World Health Organization (WHO) (http://www.who.int) and the United Nations Office for the Co-ordination of Humanitarian Affairs (OCHA), Pyongyang, Democratic Peoples' Republic (DPR) of Korea (http://www.humanitarianinfo.org/dprk) and from the United Nations (UN) (http://www.reliefweb.int).
The annual geographic distributions of malaria cases in South Korea over 12 years were determined by grouping cases by city and province where patients were located when a diagnosis of malaria was made. Information about the time required to make a diagnosis of malaria after the onset of symptoms, were obtained from the reports of patients admitted to local health centers and hospitals in Kangwon-do, South Korea.
Meteorological data, i.e., mean temperature and rainfall for the main transmission period (the 6 mo period from May to October), recorded at local weather stations in Cheolwon-gun, Kangwon-do, a malaria endemic area near the DMZ, were obtained from the Korean Meteorological Administration, South Korea.
The population densities of adult anopheline mosquitoes, over 90% of which is Anopheles sinensis, the main vector mosquito for vivax malaria in the Republic of Korea (Chai, 1999), were determined during the transmission period at one location in Cheolwon-gun, Kangwon-do, from 1993 to 2004 by two (WS Seok and YS Kim) of the authors. Adult anopheline mosquitoes emerged from the first week of May (1-10 mosquitoes/trap/night) and disappeared from the last week of October (0-14 mosquitoes/ trap/night). A black light trap (Nozawa type, Shinyoung Korea Co., Seoul, Korea) was hung from a fence about 1.5 m above the ground in shed housing one cow. Black light traps were operated without additional attractants from 18:00 to 06:00 hr twice a week during the study period. All captured mosquitoes were transported the following morning to the Kangwon Institute of Health and Environment, where they were identified, separated, and the number of anopheline mosquitoes was counted.
Mass chemoprophylaxis (1 chloroquine tablet; 300 mg base) has been administered by the Ministry of Defense to a total of 985,282 soldiers working around outbreak areas (northern parts of Kyonggi-do and Kangwon-do) weekly from 1997 to 2005. Chemoprophylaxis was also prescribed to a total of 12,189 US soldiers in South Korea during the period 1997-2000. Retiring Korean soldiers were advised to take primaquine 15 mg base daily for 14 days for chemoprophylaxis against the liver stage parasite at the time of their retirement.
Spearman's correlation analysis was used to examine correlations between the number of new malaria cases, year, climatic factors, i.e. annual mean temperature (℃) and rainfall (mm), and the annual mean number of mosquitoes trapped during May to October. The monthly mean number of anopheline mosquitoes, and the mean number of mosquitoes trapped weekly and annual totals were calculated from mean monthly numbers trapped during the 6 month transmission period. P values of < 0.05 were regarded as statistically significant.
RESULTS
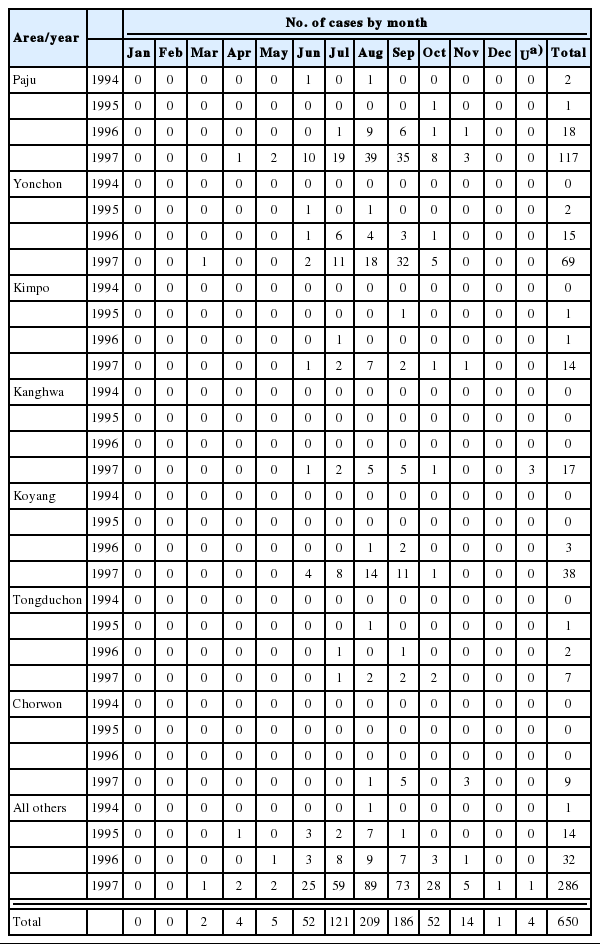
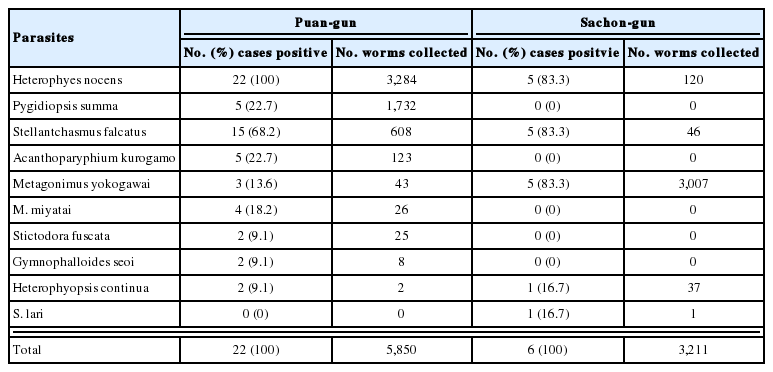
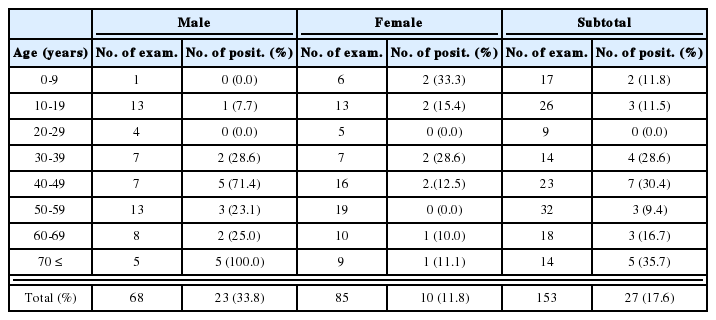
During the past 13 years (1993-2005), at least 937,634 indigenous vivax malaria cases have been reported in the Korean peninsula (South Korea and North Korea) (Table 1). Based on available data between 1999 and 2004 in South and North Korea, the number of cases reported peaked in 2001 with 298,058 cases in the Korean peninsula. In South Korea, during the period 1993-2005, a total of 21,419 indigenous vivax malaria and 488 imported malaria cases were confirmed (Table 1). The indigenous malaria patients included 8,353 (39.0%) civilians and 13,066 (61.0%) soldiers, including 5,626 retired soldiers (26.3%) who had retired from military service for less than one year at disease onset. The number of reported cases peaked in 2000 with 8.9 cases per 100,000 of the South Korean population. Thereafter, the number of reported cases declined sharply by approximately 26-40% per annum to 1.8-2.9 cases per 100,000 of the population in 2004-2005 (Table 1).
The annual incidence rate (including retired soldiers discharged < 1 year prior to onset and soldiers on duty) peaked at 457.3 cases per 100,000 soldiers in 2000. The incidence decreased by more than 84% between 2000 and 2004, but then increased by 35% in 2005 (Table 1). The same trend, i.e., peak in 2000 followed by a sharp decline until 2004 and a rise in 2005, was observed both among serving and retired soldiers. Among civilians, the annual incidence rate peaked at 3.3-3.4 cases per 100,000 in 1999-2000, and then decreased to 0.9 in 2004, but increased again to 1.9 in 2005 (Table 1).
In 1999, total 95,960 malaria cases were reported in North Korea, but this increased explosively 3-folds between 1999 and 2001 (1,331.4 per 100,000 North Korean population), and after 2002 decreased sharply to 208.2 and 151.7 per 100,000 population in 2003 and 2004, respectively (Table 1).
The annual numbers of malaria cases reported by nationwide administrative districts (provinces and large cities) are given in Fig. 1, as sums of 2 years, from 1994-1995 to 2004-2005. Of the total 21,419 cases registered during the 12 year period, most (85.4%) developed febrile illness in northern provinces and cities near the DMZ (the highest risk areas), including 10,411 cases (48.6%) in Kyonggi-do, 3,083 (14.4%) in Kangwon-do, 2,710 (12.7%) in suburban Seoul, and 2,089 (9.8%) in suburban Incheon (Fig. 1). In Kyonggido, the most serious outbreak area, the peak incidence occurred in 1998 with 2,197 cases, and decreased gradually afterwards. However, in Kangwon-do, the second most serious outbreak area, the peak incidence of 825 new cases, occurred in 2000. Small numbers of cases were reported from various Provinces and Cities countrywide through 12 years, although these cases were predominantly among retired soldiers who had served in northern parts of Kyonggi-do or Kangwondo about a year previously, thus indicating a long incubation period. The numbers of patients reported in other Provinces and Cities are shown in Fig. 1.
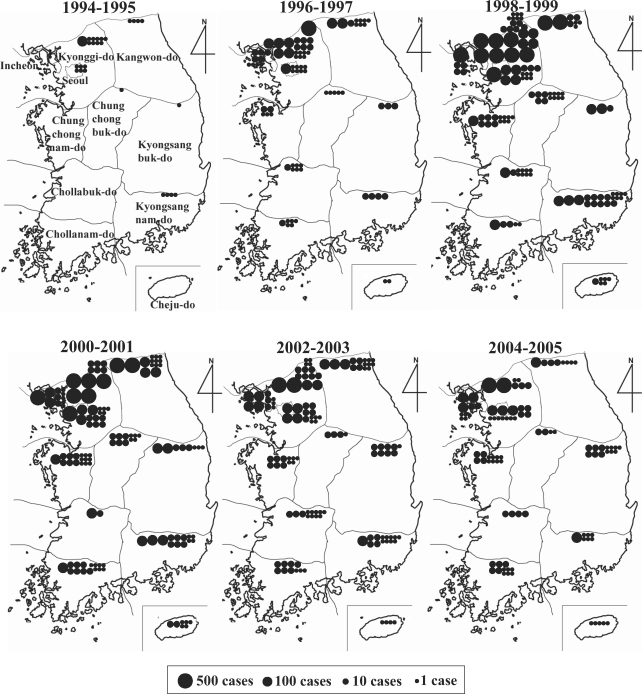
Maps of South Korea, showing the numbers of indigenous vivax malaria cases reported by administrative districts (Provinces and Cities, including Incheon and Seoul) from 1994-1995 to 2004-2005. The figure represents the number of patients who developed febrile illness and were diagnosed in the district, but does not necessarily mean actual contraction of malaria in each district.
Meteorological data, i.e., annual mean temperature and rainfall, and mean mosquito population densities, during 1993-2004, were analyzed in terms of their relationships with the annual total numbers of malaria cases reported in Kangwon-do, South Korea (Table 2). Spearman's correlation analysis showed that the occurrence of malaria in high risk areas was correlated with the mosquito population, only with low significance (P= 0.048), and no positive association was observed with temperature or rainfall (Table 2).
Mean annual temperatures, rainfalls, and anopheline mosquito population densities compared to annual malaria incidence rate in Kangwon-do, South Korea, from 1993 to 2004
The time required for a diagnosis of malaria from the onset of febrile paroxysm has reduced year by year in most outbreak areas of Kangwon-do. For example, 66 (44.0%) of 150 patients were diagnosed and treated within 6 days of symptom onset in 1999, but this increased to 61.7-73.6% during 2000-2002 (Table 3).
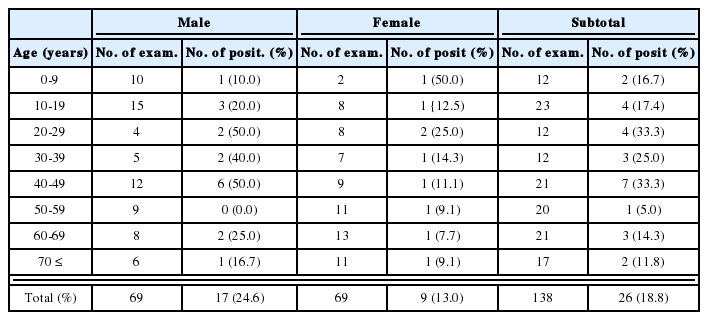
Days required for confirmation of malaria diagnosis after the onset of symptoms among civilians and veterans in risk areas of Kangwon-do, South Korea, from 1999 to 2002
In 2001, the South and North Korean governments started to provide budgetary supports for facilitating malaria control programs in both countries. In the case of South Korea, 2 northern provinces (Kyonggido and Kangwon-do) and one city (Incheon), received budgetary supports for mosquito control from the KCDC, and this was followed by fiscal support from provincial and city health bureaus from 2001 to 2004. The total expenditures over this 4 year period in South Korea was 5,154,700 USD (Table 5). In North Korea, during the period 2001-2004, international supports for malaria control have been provided by WHO (for education and assistance for technician training), the International Federation of Red Cross and Red Crescent (IFRC) (anti-malarial drugs) and South Korea. The total amount of anti-malarial aid given to North Korea over this 4 year period was 3,150,650 USD (Table 5). In South and North Korea, during the same period (2001-2004), 8,305,350 USD were spent on malaria control. Items of supports provided by South Korea to North Korea included anti-malarial drugs (chloroquine and primaquine), mosquito control related materials and equipments (insecticide impregnated-bednets, personal protection fabrics, insecticides, and insecticide spraying equipment) and laboratory supplies for prompt diagnosis (microscopes and staining reagents) in local health centers and hospitals, and small amount of cash for the education of health personnel(Table 5).
DISCUSSION
Our study demonstrated that the number of reemerging vivax malaria cases in South Korea increased exponentially during the years 1993-2000, but then decreased steadily until 2004 with a slight increase in 2005. This post 2000 decrease in malaria incidence was observed countrywide, and included high risk areas near the DMZ. Control programs were operated, including mass chemoprophylaxis, vector control, and financial aids to North Korea for malaria control, and are believed, at least in part, to have contributed to the reduction of malaria incidence.
Malaria transmission requires the combined presence of the Plasmodium parasite, the anopheline mosquito vector, and the human host. Both parasites and vectors are strongly affected by climate, for example,temperature determines parasite and vector development, and rainfall provides the water required for vector breeding. In Rwanda and China, monthly mean temperature was found to play an important role in malaria transmission (Loevinsohn, 1994; Bi et al., 2003). However, with regard to rainfall levels, reports are contradictory; some studies have reported that rainfall is a key factor (Lindblade et al., 1999; Bi et al., 2003), whereas others have reported negative effects (Singh and Sharma, 2002). In a previous South Korean study, increases in temperature and precipitation were found to be correlated with seasonal vector mosquito population densities, and with the subsequent seasonal incidence of malaria (Lee et al., 2002). In this previous study, 2 climatic factors were compared with averaged data collected over a 30-year period, though no statistical analysis was performed (Lee et al., 2002).
In our study, low grade statistical significance (P=0.048) was observed in the correlations between anopheline mosquito densities and the annual malaria incidence during the 1993-2004 period in Kangwondo, but none between the climatic variables and malaria incidence. Although mosquito densities during 1998-2001 could not be clearly correlated with malaria incidences, mosquito densities during these years were significantly (P < 0.05) higher than those before 1998 when malaria incidence was comparatively low (Table 2). Nevertheless, detailed ecological and epidemiological studies are needed to assess the true impact of climatic variables on malaria outbreaks in South Korea.
Regardless of the control strategy adopted, the early diagnosis and proper treatment of those infected is essential (Lee et al., 2003). In South Korea, the average duration between the onset of malarial fever and diagnosis at a health center or a hospital was 23.6 days in 1995, 9.5 days in 1997, and 8.0 days in 2000 (Park et al., 2003). Since 2000 about two-thirds of malaria patients have been more quickly diagnosed and treated, within 6 days, for example, in Kangwon-do (Table 3). Moreover, in 2004, the average detection time became as short as 3-4 days in highly endemic areas in Kangwon-do (data not shown), and it is speculated that early case detection substantially reduced the malaria transmission from patients to mosquitoes.
Mass chemoprophylaxis is another major contributor to the observed recent reduction in malaria cases. Before 1997, more than 80% of malaria cases occurred in northern parts of Kyonggi-do and Kangwon-do, the major outbreak areas (Chai, 1999; Park et al., 2003), and most patients were soldiers stationed near the DMZ. Therefore, mass chemoprophylaxis was administered to soldiers located in these endemic areas in 1997 and has continued ever since (Table 4). From 1997 to 2005, a total of 985,282 soldiers received chloroquine and primaquine prophylaxis. As a consequence, malaria incidence among soldiers on duty and retired soldiers decreased rapidly during 2001-2005. This prophylaxis program must have been largely responsible of the observed reduction in the malaria incidence.
However, it should be noted that the proportion of civilian cases among all malaria cases has increased from 38.2% in 2000 to 50.6% in 2004. This increase in the proportion of civilian cases suggests an increase in local transmission away from the DMZ (civilians usually live some distance from the DMZ). This increase in local transmission is also suggested by the fact that outbreak areas have expanded in southerly and easterly directions since 1998 (Chai, 1999; Park et al., 2003; Yeom et al., 2005).
It is also of note that a substantial number of cases (more than 30% of all patients during the period 1998-2004) have been reported in Pusan, Taegu, Kyongsangbuk-do, and Kyongsangnam-do regions, which are considerably removed from major outbreak areas. Such cases may include retired soldiers, travelers to major outbreak areas, and locally infected civilians. In the case of retired soldiers living in these areas, the majority were probably infected while working in major outbreak areas, and developed febrile illness after a long incubation period of 5-13 mo (Chai, 1999), whereas travelers may have developed fever after a short (within 1 mo) or a long incubation period. It is unfortunate that no study has yet reported firm evidence of local malaria transmission in areas remote from the major outbreak areas.
There is no doubt that vivax malaria reemergence in South Korea was originally caused by infected mosquitoes originating from North Korea and the DMZ (Chai, 1999; Park et al., 2003). In this regard, it is worth mentioning that genotypes of circumsporozoite protein (Kho et al.,1999), merozoite surface protein (MSP)-1 (Zakeri et al.,2003), Duffy-binding protein (Kho et al.,2001), apical membrane protein antigen-1 (Han et al.,2002), and MSP-3α (Han et al., 2004) of the reemerging vivax malaria in South Korea are similar to those found in the North Korean (NK) strain. Infected mosquitoes probably constantly migrate from North to South Korea (Cho et al., 2002), and we suggest that a large proportion of malaria cases in South Korea have resulted from this influx. Moreover, it is evident that the malaria situation in northern South Korea will be influenced by that in North Korea.
With regard to the malaria situation in North Korea, no data was available before 1997. However, recently some occurrence data has become available (Global Funds to Fight AIDS, Tuberculosis and Malaria, 2003; United Nations, 2003; United Nations Office for the Co-ordination of Humanitarian Affairs DPRK, 2003, 2004; World Health Organization, 2004; Chol et al.,2005). Indigenous cases have now been reported from 1997 (Chol et al., 2005), and nationwide patient numbers increased sharply prior to 2001, but then dramatically reduced to 2004. Several factors may have facilitated the increase in malaria cases during 1999-2001 in North Korea. Such factors may include changes in agricultural practices, such as, reduced use of pesticides and changes in rice field irrigation, intermittent big flooding, increased vector host densities, and inadequate health care delivery system.
However, a malaria control program was implemented in endemic areas of North Korea, in South and North Hwanghae-do (Provinces) during 2001-2003 by the National Program Office of WHO, in North Korea (Chol et al., 2005). It has been stated that the prevalence of malaria began to decline immediately after implementing this control program, and individual awareness regarding malaria increased rapidly. However, more precise data are required to better assess the situation of vivax malaria in North Korea.
References
Notes
This study was supported by a Korea Research Foundation Grant (KRF-2003-003-E00043), Ministry of Education, Republic of Korea.