Travelers' malaria among foreigners at the Hospital for Tropical Diseases, Bangkok, Thailand: a 6-year review (2000-2005)
Article information
Abstract
We retrospectively examined the charts of travelers admitted to the Hospital for Tropical Diseases, Bangkok, Thailand, with malaria during the years 2000-2005. Twenty-one cases of malaria were identified, of which 12 (57%) were Plasmodium vivax infections and 9 (43%) were P. falciparum infections. There was one mixed case with vivax and falciparum infection. Only 1 P. falciparum case had complications. All cases were successfully treated with standard antimalarial drugs. Only 3 of the 21 cases were thought to be acquired in Thailand, the rest were regarded to be imported.
INTRODUCTION
Malaria is the most important cause of fever in travelers returning from the tropics (Svenson et al., 1995; O'Brien et al., 2002). The exact risk of acquiring malaria in tropical regions is difficult to quantify and depends on a variety of factors including destination, location, travel duration, use of insect repellents, and use of chemoprophylaxis (Loutan, 2003; Askling et al., 2005). Previous studies have established that the risk is higher in travelers to Africa than in travelers to South East Asia (Keystone, 2001; Askling et al., 2005, Freedman et al., 2006). One study estimated at 1:12,254 of the risk of acquiring malaria in Thailand (Hill et al., 1996). However, the incidence and characteristics of travelers' malaria in Thailand has not been previously studied. We therefore systematically reviewed cases of travelers' malaria seen at the Hospital for Tropical Diseases in Bangkok during the years 2000-2005.
MATERIALS AND METHODS
We retrospectively reviewed charts from foreign patients seen at the Hospital for Tropical Diseases between the year 2000 and 2005. Records of non-Thai subjects diagnosed with malaria were reviewed and data on presenting symptoms, duration of fever, travel history, species of malaria, initial parasite count, treatment, and outcome were recorded. Initial parasite counts per microlitre blood were calculated by using the number of parasites per 1,000 RBC in a thin film or per 200 WBC in a thick film. We excluded immigrant patients from Laos, Myanmar, and Cambodia. They were not considered as true traveler in our study. The country where patients became infected was determined by travel history, particularly by the location of areas visited by the patient in the days and weeks before the onset of symptoms of malaria.
RESULTS
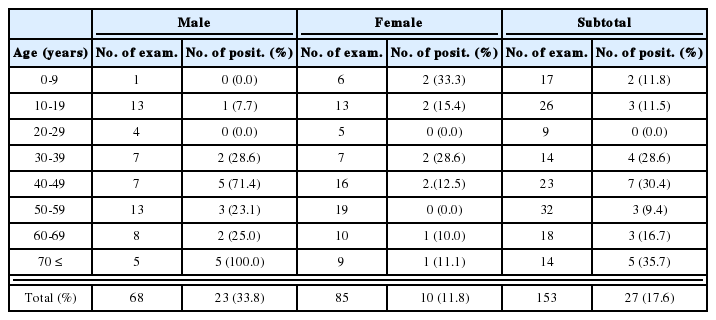
During the years 2000-2005, a total of 136 febrile foreigners were evaluated at the Hospital for Tropical Diseases in Bangkok. Malaria was diagnosed by the presence of plasmodial parasites on peripheral blood films in 21 patients (15%) (Table 1). All patients were males and the mean age was 35.0 years (SD; 13.6 years). Tourism (47.6%) was the most common reason for travel to Thailand. The majority of cases (18) were imported; only 3 patients (14.3%) were thought to have acquired malaria in Thailand. India appeared to be the most common country of infection (Tables 1, 2). Fever was the presenting symptoms in all cases. Median duration of fever was 3 days (range 1-12 days). Twelve of 21 (57.1%) patients were infected with P. vivax, while 9 patients were diagnosed with P. falciparum infection. There was one mixed infection with P. falciparum and P. vivax. Three out of 12 P. vivax patients had history of previous malaria. Median initial parasite count of P. vivax cases was 780/µl (range 80-15,000), whereas median initial parasite count of P. falciparum cases was 5,000/µl (range 160-800,000).
Treatment and outcome
Thirteen of the 21 patients (61.9%) required admission to hospital; 10 falciparum and 3 vivax cases. The mean duration of hospitalization was 3 days (SD; 1 day). No deaths occurred in cases with standard antimalarial therapy (Table 3). Only one patient had severe falciparum malaria. He was a 41-year old German male who had trekked in forested areas in Laos 2 weeks before developing fever. On admission, 16% of the patient's RBC contained malaria parasites. This rate of parasitemia is considered severe in non-immunes according to World Health Organization (WHO, 2000). In addition to hyperparasitemia, the patient also had oliguria and his creatinine was rising. He was admitted and treated with intravenous sodium artesunate. Renal function returned to normal with rehydration and no hemodialysis was required. Six days later the patient was aparasitemic, much improved, and was discharged.
DISCUSSION
The incidence of malaria in Thais is declining. Data from Thai Ministry of Public Ministry, in 2002 (fiscal year), there were 47,948 new malaria cases, which declined to 28,477 in 2005. The risks of acquiring malaria in Thailand are limited to a few well demarcated areas mainly along the mountainous border regions. The policy of the Thai Ministry of Public Health is not to recommend antimalarial chemoprophylaxis, because of very low risks for travelers and prevalence of multi-drug-resistant strains of P. falciparum. WHO and US Centers for Disease Control (CDC) advise that only travelers to high risk areas of Thailand should consider antimalarial prophylaxis (WHO, 2005; Centers for Disease Control, 2005).
Many details about travelers' malaria in Thailand are difficult to know with certainty. Some travelers have visited several different countries and it is not possible to be sure of the country where malaria was acquired. Other travelers are only diagnosed with malaria after their return home, so data from travelers found to have malaria in Thailand will underestimate the total number of cases of travelers' malaria. Malaria remains an important cause of fever in travelers returning from the tropics. The incidences of malaria in travelers vary according to studies. It was reported from a tropical center in France that as high as 75% of febrile cases were caused by malaria (Parola et al., 2005). The most recent study has shown that 13% of febrile travelers who returned from South East Asia were caused by malaria (Freedman et al., 2006).
In our study, 15% of febrile travelers presenting to our hospital had malaria and only 14% of these cases were thought to have been acquired in Thailand. More than half of the malaria cases were due to P. vivax, severe malaria was uncommon, and response to treatment was good. No mortality was found in our series. Out of 21 patients, 5 (23.8%) were from India and all of them were though to have acquired their infections in that country. This may be due to the widespread areas of malaria risk in India. WHO estimated that 95% of Indian population lived in malaria risk areas (WHO, 2000). However, the trend of malaria cases in India slowly declined. There were approximately 2 million new malaria cases in India each year. So the febrile Indian travelers should be screened for malaria even when they travel to a non-endemic country, since they can acquire malaria in their home country. Apart from Indian patients, in our series, we have 3 malaria cases from Papua New Guinea, Mozambique, and an African country that were thought to have acquired malaria in their home country and get sick in Bangkok. With the increase in international travels, travelers' malaria will be more important. Physicians should rule out malaria in all febrile patients who have been traveling or came from endemic areas of malaria.
ACKNOWLEDGMENTS
We thank Dr. George Watt, Faculty of Tropical Medicine Consultant, for helping to review this manuscript. We also thank the staffs of the Hospital for Tropical Diseases for their help and support.