Ectopic Schistosomiasis Involving Axillary Lymph Nodes
Article information
Abstract
Axillary lymph node schistosomiasis is a form of ectopic schistosomiasis, in which the Schistosoma adult worms or eggs are infected in the axillary lymph nodes. A 53-year-old woman visited our hospital with a small mass in the right armpit, which had been present for over 1 month. Histological examination of biopsy samples from the right axillary lymph nodes revealed granulomas containing calcified Schistosoma eggs. This is the first authentic case of ectopic schistosomiasis identified in the axillary lymph nodes.
INTRODUCTION
Ectopic schistosomiasis is defined as the presence of adult worms and/or eggs outside the portal system, i.e., central nervous system, lungs, testis, kidney, and etc. [1]. It is occasionally detected in the lymph nodes related to the digestive system, such as in the gallbladder, gastric mucosa, ileocecum, and rectum [2–5], but rarely in the remainder of lymphoid tissue. We report a case of ectopic schistosomiasis in the axillary lymph nodes.
CASE DESCRIPTION
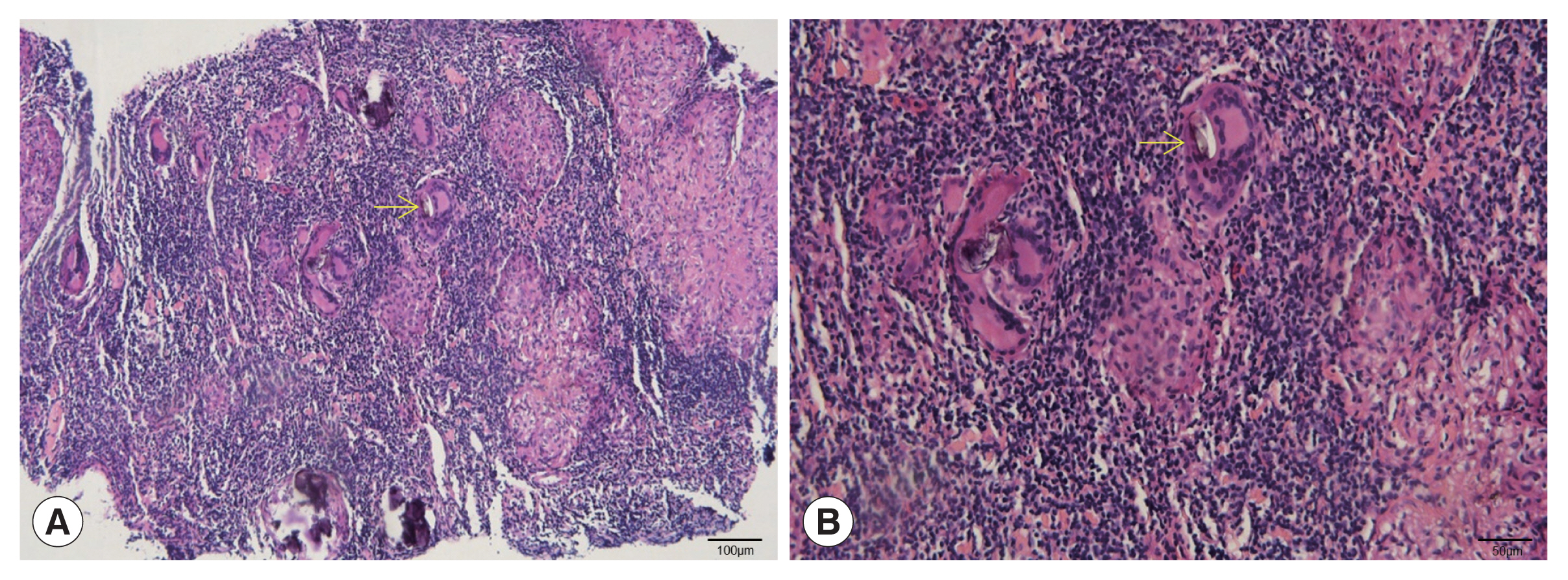
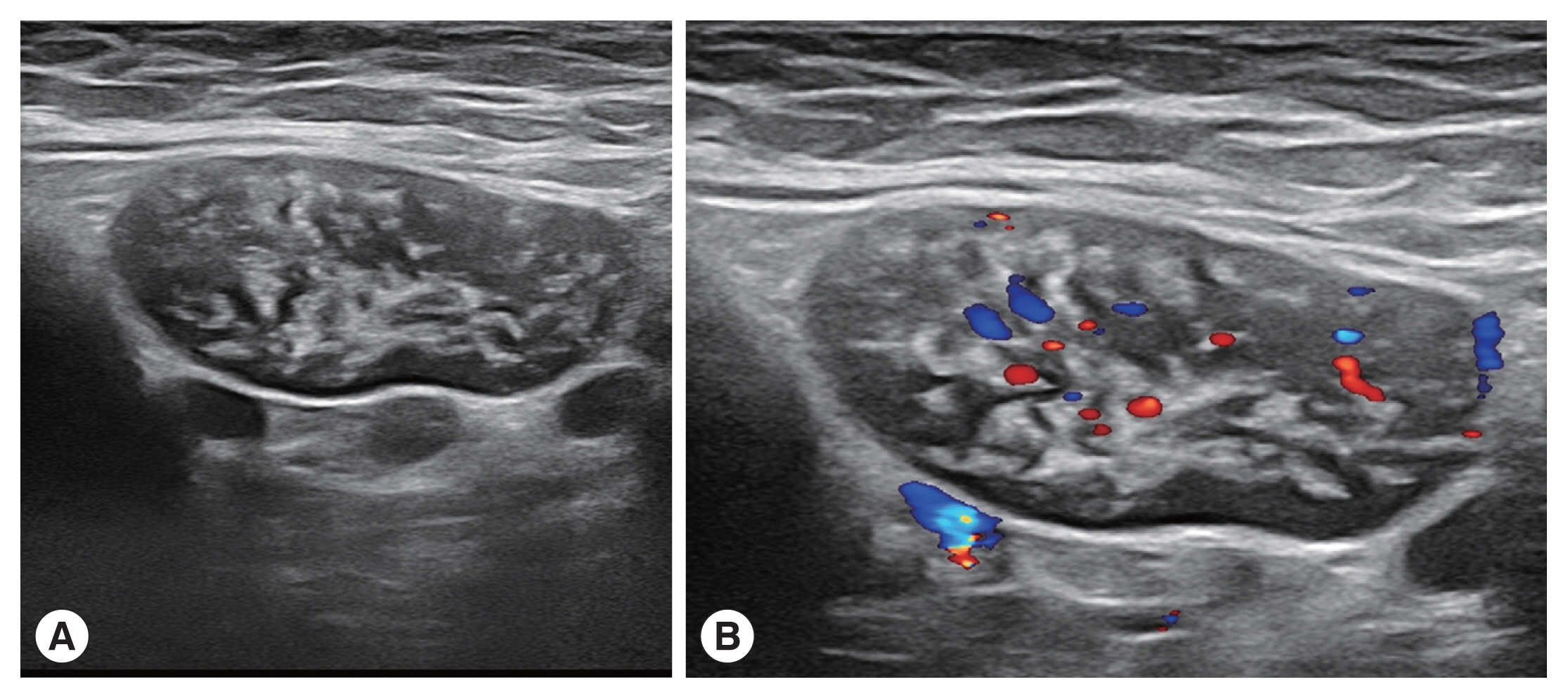
The patient was a 53-year-old woman living in Hefei City (Anhui Province). She was admitted to our department in 2022 with a small mass in the right armpit that had been persisted for over 1 month. The patient had no fever and no inflammatory manifestations in the right armpit. She had not experienced fever, chills, night sweats, or gastrointestinal, musculoskeletal, or neurologic symptoms. Her physical examination revealed a mass in the right armpit, approximately 4.0 cm×2.0 cm×1.0 cm in size. Breath sounds were normal. Complete blood counts showed a normal level of eosinophils (0.11×109/L), while red blood cell (3.66×1012/L), and hemoglobin (113 g/L). Hematocrit (0.332 L/L) levels were below the reference range. Blood coagulation functions were within the normal range. Ultrasonography of the liver, breast, thyroid gland, cervical lymph node, and inguinal lymph nodes revealed no specific lesions. Ultrasonography of the right axillary lymph nodes revealed more than 3 hypoechoic oval shaped nodules that had a clear edge. Strong-echo light spots were diffusely distributed in the hypoechoic nodules, the largest of which was 41 mm×17 mm (Fig. 1A). Color doppler ultrasonography showed that the dot-bar color doppler flow signal was relatively rich in these enlarged hypoechoic nodules (Fig. 1B). Histological examination of biopsy samples from the right axillary lymph nodes revealed granulomas containing multinucleated giant cells and elliptic calcified Schistosoma eggs (Fig. 2). In further questioning, the patient stated that 7 years prior to symptom onset, she had travelled through Yunnan province, where she had spent sometimes swimming in Lake Erhai, an endemic area for Schistosoma japonicum.
(A) The right axillary lymph node exhibits numerous hypoechoic oval nodules with clear edges. Strong-echo light spots are diffusely distributed in hypoechoic nodules. (B) The dot-bar color doppler flow signal is relatively rich in the enlarged hypoechoic nodules.
DISCUSSION
Schistosomiasis of the axillary lymph nodes has rarely been reported. Our patient had no clinical symptom, but an axillary mass was confirmed by histopathological examination. Schistosoma eggs could be differentiated from those of Paragonimus and Fasciola by their shape, which was elliptic, and their eggshell thickness, which was uniformly distributed. The Paragonimus egg is ovoid, unembryonated, and thick-shelled, with an operculum at one end and opercular shoulders; similarly, the Fasciola egg is ovoid, unembryonated, large, and operculated. However, the Schistosoma egg is embryonated and do not have an operculum. The main ultrasonographic manifestations were lymphadenectasis and calcification, and the calcification pattern was the same as lymphoid reactive hyperplasia [6]. Ectopic schistosomiasis should be differentiated if there are ultrasound findings of lymphangiectasia and calcification in the lymph nodes in patients who have traveled to schistosomiasis endemic areas or have been in potentially contaminated water. The definitive diagnosis should be carried out by fecal egg examination and ultrasound-guided histological examination.
There may be 2 possibilities for pathogenesis of axillary lymph node schistosomiasis in this patient. First, adult worms might had been infected in the axillary vein and laid eggs. The adult worms mainly thrive in the mesenteric veins of definitive host. After mating, the females lay eggs at the ends of the veins. Some eggs penetrate the intestinal walls and are expelled with feces, while some eggs make their way into the liver via the blood and may become calcified. However, previous studies have reported that the adult worm might also inhabit other areas such as the right gastric vein, left gastric vein, pancreaticoduodenal veins, or parotid gland [7,8]. Therefore, we cannot rule out the possibility that the adult worms infected the axillary vein and laid eggs that migrated into the axillary lymph nodes. Another possibility may be that the eggs migrated from the breast. Previous studies have revealed that the breast is the most common ectopic site [9,10]. The lymph and venous blood flow though the breast into the axillary lymph nodes. Hence, the eggs might have reached the axillary lymph node by the way of lymphatic and/or venous flow. Our patient showed normal ultrasonographic finding of the breast, which suggest that the eggs came from the lymph and venous blood flow through the breast was relatively low. We thought that this patient may had an adult worm infection in the axillary vein and laid eggs that migrated to the axillary lymph nodes.
The egg granuloma was the primary pathological lesion associated with schistosomiasis, not only promoting the synthesis of extracellular matrix and fibrosis [11], but also causing dysplasia that stimulate the mucous membrane [3]. Some studies have reported clinical symptoms such as lymph node nodules, lymphoid tissue necrosis, fibrotic nodules, and piezoelectricity due to lymph node Schistosoma egg granulomas [4,5,12]. Since our patient had only calcified egg granuloma, it seems that she manifested only with lymphadenectasis with minimal damage.
In summary, although China is steadily moving toward schistosomiasis elimination, a few of new infections are still detected [13]. Therefore, when physician encountered patients with enclosed mass in the axillary, it is important to consider the possibility of ectopic schistosomiasis. Fecal examination for Schistosoma eggs, serological test, and pathological examinations should be carried out for an accurate and rapid evaluation of patient.
ACKNOWLEDGMENTS
This study was supported by Anhui Provincial Key Laboratory of Microbiology & Parasitology (No. BY-2022Z07), Anhui Medical University, China.
Notes
The authors declare that there is no conflict of interest.