Epidemiological survey of Giardia spp. and Blastocystis hominis in an Argentinian rural community
Article information
Abstract
The aim of this study was to relate personal data, socio-cultural and environmental characteristics, and the presence of symptoms/signs with the frequencies of Giardia spp. and Blastocystis hominis among a rural population in Buenos Aires Province, Argentina. Of the surveyed population (350), 3.7% were infected with only Giardia spp. or 22.9% with B. hominis, and 2.3% were infected with both protozoa. The frequency of infection according to sex; 6.1% of males were infected and 1.6% of females by Giardia spp., 26.7% and 19.5% by B. hominis, and 2.4% and 2.2% by both parasites, respectively. Giardia spp. was detected in only three adults (over 14 years), but B. hominis was more frequent in adults than in children. The prevalences of these protozoa in this community are lower than those reported by other Argentinean studies, which is probably associated with the low density of the studied population (5.95 inhab/km2). Statistical analysis revealed that a male sex, flooding of the home, the use of a latrine, and an abdominal pain were correlated with the presence of these parasites, which indicate the importance of these factors in rural communities.
INTRODUCTION
Protozoan intestinal infections caused by Blastocystis hominis and Giardia spp. are associated to climatic factors, basic sanitary conditions, and sociocultural characteristics (Gamboa et al., 2003). Traditionally, the prevalence of these infections was considered a "stable endemic characteristic" resulting from the dynamics of repeated re-infection (Atías, 1999).
According to Atías (1999), the frequency at which repeated infection occurs in a population depends on the "infection pressure" and host susceptibility. "Infection pressure" is defined as the number of host exposures at a given location over a certain period of time. The factors involved in "infection pressure" are of two types: environmental and socio-economic, which are intimately linked since the environment has a certain influence on the socio-economic conditions of a population and human activities also affect the environment (Soriano et al., 2001).
Environmental conditions (e.g. temperature, humidity, wind, soil) and socio-economic factors are responsible for spreading and for developing infectious forms of B. hominis and Giardia spp., and for polluting the environment with these agents.
Giardiasis is a cosmopolitan zoonotic infection, and predominates in mild humid climates. According to Crompton (2000), two hundred million are infected with Giardia spp. worldwide. And, 15% of the rural population in Latin America is estimated to be infected with these parasites; with a higher prevalence among children (Atías, 1999). In addition, the infection prevalence is lower in the upper strata of the population, and increases in day care centers attended by the children of poorer families (Fernández et al., 2002). On the other hand, B. hominis is an intestinal parasite that infects both in humans and animals. It also has a higher prevalence in tropical regions, reaching infection levels of 20-50%, especially in rural areas (Guignard et al., 2000). Moreover, both protozoan infections are associated with non-specific gastrointestinal symptoms (Miller et al., 2003) and diarrhea (Carbajal et al., 1997).
The purpose of this study was to relate personal data, socio-cultural and environmental characteristics, and the presence of symptoms/signs with the frequency of Giardia spp. and/or Blastocystis hominis among a rural population in the province of Buenos Aires, Argentina.
MATERIALS AND METHODS
Study area
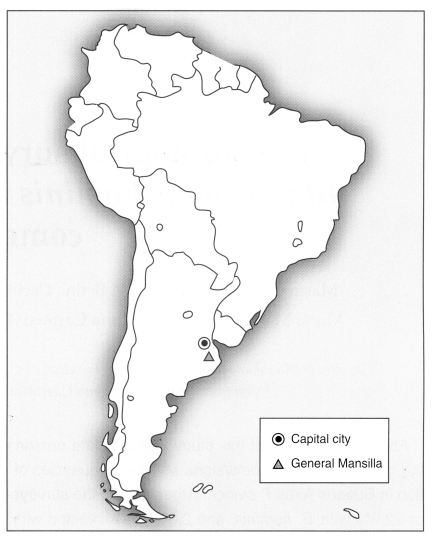
General Mansilla is a town situated in the northeast region of the Province of Buenos Aires, which lies in mid-west Argentina some 95 km from the capital city, Buenos Aires (Fig. 1). Six thousand people reside in an area of 1007.5 km2 (5.95 inhab/km2). The town has a commercial downtown or "urban region", surrounded by a rural area.
Selected population
Total 350 people (185 females and 165 males), with or without symptoms, who attended a Health Care Center during April and May of 2003, were studied. Of these, 201 people lived in an urban area (UA) (57.4%) and 149 in a rural area (RA) (42.6%); 249 were under 14 years old, and 144 lived in the UA. Each individual was surveyed for personal, environmental and socio-cultural data. Personal information - age, sex, and place of residence - was collected, as was socio-cultural and environmental information - type of home (i.e., built of cardboard or tin, wood, fibrocement, or masonry), type of floors in the home (dirt or cement), garbage disposal (open pit, burning, burying or city garbage collection), water supply (running water, home pump, community pump), tap (inside/outside, public), body waste disposal (sewage, well with a chamber, cesspool, or latrine), overcrowding (presence or absence, presence was defined as more than three people sleeping to a room), and house flooding (never, sometimes, frequent). In addition, subjects were asked about the presence or absence of the following symptoms/signs: anal itching, abdominal pain, sleeping disorders, diarrhea, vomiting, appetite loss, weakness, and inexplicable fever.
Parasite analysis
A serial coproparasitological analysis was performed, consisting of stool sampling from a daily spontaneous bowel movement, over five consecutive days; sample were stored in a jar containing 5% formaldehyde. To detect Giardia spp. and B. hominis, the samples were processed using a modified Telemann technique (Gamboa et al., 2003), and processed pellets were stained with lugol and observed under a microscope.
Statistical analysis
Significant associations were determined using the chi square test and Fisher's test. Odds ratios (ORs) were calculated for statistically significant associations.
Logistic regression models were adjusted by the backward conditional stepwise method to determine the presence of either Giardia spp. and/or B. hominis in all subjects (urban and rural). Socio-cultural and environmental characteristics, symptoms, age, and sex were used as (independent) explanatory variables. Logistic regression models were constructed to predict the probability of being infected in accord with identified variables. From this prediction, individuals were classified according to their risk of being parasitized, as high risk and low risk (probabilities of ≥ 0.5 and <0.5 respectively). Sensitivity (S), specificity (E) and global adjustment (i.e., total percentage of correct predictions) were estimated for each model. Models were used to obtain OR estimates for each variable. SPSS software, version 11.5 was used throughout.
RESULTS
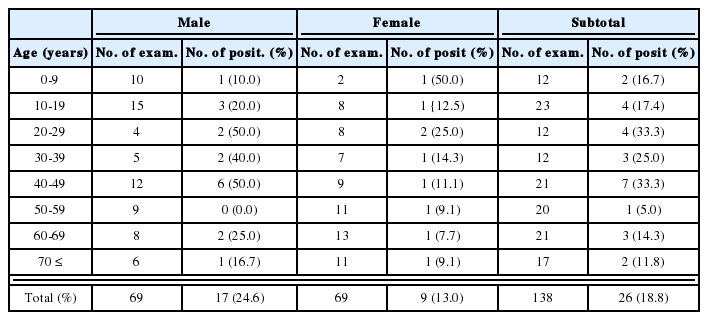
Sex, age, and place of residence in the analyzed population are shown in Table 1. In the studied population, 3.7% (13/350) of subjects were infected with Giardia spp. only, 22.9% (80/350) with B. hominis only, and 2.3% (8/350) were infected with both protozoa. Regarding Giardia spp. infection, 6.1% (10/165) of males were infected and 1.6% (3/185) of females, similarly for B. hominis, 26.7% (44/165) of males were infected and 19.5% (36/185) of females, and 2.4% (4/165) and 2.2% (4/185) were infected with both protozoa. These apparent differences between the sexes were not significant.
The prevalence of Giardia spp. was 3.5% (7/201) in the UA and 4.0% (6/149) in the RA. B. hominis prevalence was similar in both areas, i.e., 23.9% (48/201) in the UA and 21.5% (32/149) in the RA. Of the 8 people parasitized by both protozoa, 3 (1.5%) lived in the UA and 5 (3.4%) in the RA.
Distributions according age, sex, and place of residence are shown in Table 2. Analysis of the age distributions of both parasites in the populations revealed that the frequency of Giardia spp. infection was highest among those aged 2 to 7 years, peaking at 4 years of age. On the other hand, B. hominis less age dependent and was found to be present in subjects up to 73 years old, peaking between the ages 4 and 14. When the data of both parasite infections were evaluated, mean age for Giardia spp. infection was 7 years and for B. hominis infection 26 to 33 years.
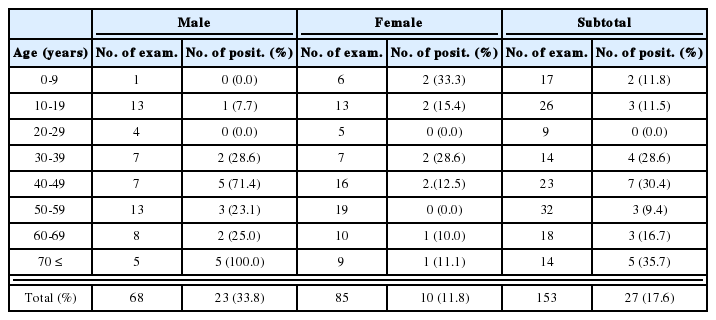
Frequencies of Giardia spp. and/or Blastocystis hominis infections in the General Mansilla population, with respect to sex, place of residence and age
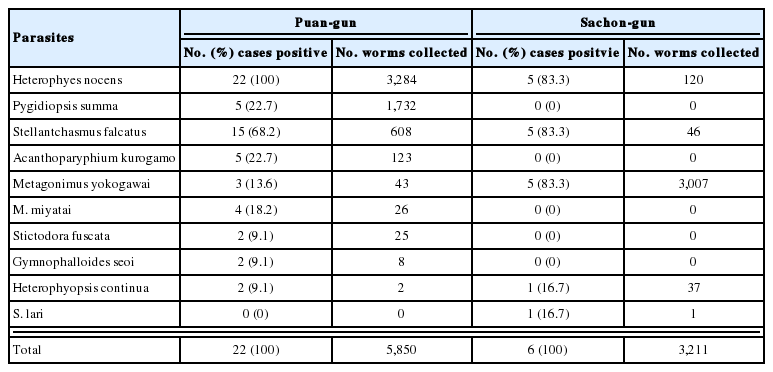
Socio-cultural and environmental data of the study population are shown in Table 3. When these variables and the presence/absence of symptoms/signs were correlated with parasite frequency, a statistically significant relation was found between:
- the presence of Giardia spp. (only) with; age (< 14 years old, p = 0.020, OR = 11.49), sex (male, p = 0.028, OR = 3.94), flooding of homes (frequent, p = 0.000, OR = 10) or the type of home (cardboard/tin, p = 0.001, OR = 7.08)
- the presence of B. hominis (only) with the home floor type (dirt, p = 0.002, OR = 2.36), sewage disposal (latrine, p = 0.003, OR = 2.85), or abdominal pain (presence, p = 0.011, OR = 1.94).
- the presence of both parasites with flooding of homes (frequent, p = 0.000, OR = 17.86), home floor type (dirt, p = 0.000, OR = 27.82), home type (cardboard/tin, p = 0.023, OR = 5.89), sewage disposal (latrine, p = 0.000, OR = 24.65), and a water tap (public, p = 0.000, OR = 17.72).
A significant association was found between people parasitized with these protozoa (101/350) and: sex (male, p = 0.014, OR = 1.79), flooding of the home (frequent, p = 0.000, OR = 6.02), type of home (cardboard or tin, p = 0.010, OR = 1.86), floor inside the home (dirt, p = 0.000, OR = 3.38), body waste disposal (latrine, p = 0.000, OR = 3.76), a water tap (public, p=0.039, OR=2.49), and abdominal pain (presence, p=0.001, OR=2.32)
No significant differences were found between Giardia spp. or B. hominis infection and the place of residence (i.e., urban or rural).
Logistic regression models identified the following variables: a male sex, frequent home flooding, body waste disposal by latrine, and the presence of abdominal pain as being significantly correlated with Giardia spp. and/or B. hominis infection. This model classified 17.2% of parasited individuals (S) and 95.1% of individuals not infected with these parasites (E). Globally, it classified the 72.9% of individuals correctly (Table 4).
DISCUSSION
The overall frequency of Giardia spp. infection found in the present study was higher than those reported for similar studies in Italy (3.5%, Giacometti et al., 2000); but it is lower than those reported in Venezuela (21%, Miller et al., 2003), Chennai (16%, Fernández), Pakistan (23.78%, in Siddiqui et al., 2002), and in Brazil (27.4%, Newman et al., 2001). Similar results were obtained in studies carried out in Thailand (5.3%, Waikagul et al., 2002), and Spain (5.05%, Perez Armengol et al., 1997).
Other studies carried out in Argentina have reported higher rates of these parasitoses. Thus, Gamboa et al. (2003) reported 34% for a shantytown, Guignard et al. (2000) 23% in a population living in temporary homes, and Borda et al. (1996) who reported 29% in shantytown.
As regards studies carried out on the prevalence of B. hominis in similar populations in other countries, our results are higher than those published by Wang et al. (2002) in China (1% and 5.96%), Windsor et al.(2002) in the United Kingdom (6.9%), Carbajal et al. (1997) in Spain (16.5%), Waikagul et al. (2002) in Thailand (0.8%), and Miller et al. (2003) in Venezuela (16%).
Percentages similar to those of the present study were found by Taamasri et al. (2000) in members of the Thai Army and their families (21.9%). As regards data collected in Argentina, Gamboa et al. (2003) report 48% in a shantytown, Guignard et al. (2000) 44.4% among those living in temporary homes, Pezzani et al. (1996) 65.8% among a suburban population, and Soriano et al. (2001) 24.6%.
A compared with previous Argentinean figure our prevalence rates for both parasites are notably lower. This may be due to the rural nature of our study population, and socio-economic, cultural, and demographic (less inhabitants per square km) differences, which would be expected reduce infection pressure. Although in this study the population was divided into RA and UA, the latter did not have access to the modern sanitary and building infrastructure facilities characteristic of the large cities in Argentina. Thus the present study found no significant parasite frequency differences between the two areas.
Regarding sex, these protozoa were markedly more prevalent among males in the UA group, with an outstanding higher frequency in under 14-year olds. This is probably because the direct transmission of these parasites is related to higher population densities in the urban area, and because of the different hygiene habits of males and females in the same setting, which is reflected by the relatively low/high prevalence observed in the infant population.
Only three adult individuals had Giardia spp. infection. The category "< 14 years old" was a risk factor for this infection. On the other hand, B. hominis was found in adults and children of both sexes. These results agree with the development of acquired immunity to Giardia spp. consequent to repeated infections in childhood (Faubert, 2000). Thus, this response is unlike to B. hominis infection, which was found at markedly higher levels in adults (Stenzel and Boreham, 1996).
Of the socio-cultural and environmental variables studied, frequent flooding, dirt floor inside the home, cardboard/tin homes, and body waste disposal by latrine were associated with the prevalences of these parasites. Our logistic regression models selected frequent flooding of the home and latrine use by parasitized people as significant risk factors of Giardiasis and/or blastocystis. Therefore, the presence of these conditions could be used to estimate the risk of infection by these parasites. These data reinforce the existing strong relation between deficient sanitary conditions and intestinal parasitism, as has been mentioned by several Argentinean authors (Borda et al., 1996; Soriano et al., 2001; Gamboa et al., 2003).
Several authors reported a correlation between diarrhea, abdominal pain, flatulence, itching, vomiting, or appetite loss, and the presence of both protozoan infections (Carbajal et al., 1997; Miller et al., 2003). In this study only abdominal pain was found to be significantly associated with the presence of B. hominis and/or Giardia spp.
The present study is one of the first to associate the prevalence of Giardia spp. and/or B. hominis with socio-cultural and environmental conditions, and with the clinical features of an Argentinean rural population. We conclude that the low population density of the area studied substantially creates a lower infection pressure, and explains the lower infection prevalences of the present study. Nevertheless, the significances of home flooding, body waste disposal, gender, and abdominal pain persisted and maintained a direct and constant relationship with the presence of Giardia spp. and B. hominis.
ACKNOWLEDGEMENTS
The authors acknowledge the contribution made by Dr. Roberto Zungri for his "field work" contribution to this study and to Miss Laura Cipolla for translating the manuscript.
Notes
This study was financed by the Agencia Nacional de Promoción Científica y Técnica de la Argentina, the Alberto J. Roemmers Foundation, and the Universidad Nacional de La Plata. The study was also declared of Municipal Interest by the town of Magdalena, province of Buenos Aires, Argentina.