A survey on head lice infestation in Korea (2001) and the therapeutic efficacy of oral trimethoprim/sulfamethoxazole adding to lindane shampoo
Article information
Abstract
Total of 7,495 children including 3,908 boys and 3,587 girls from a kindergarten and 15 primary schools were examined for head lice infestation (HLI). The overall prevalence of HLI in this study was found to be 5.8%. Head lice were much more commonly detected in girls than in boys with prevalence of 11.2% and 0.9%, respectively. Sixty-nine children with HLI were treated with 1% lindane shampoo alone (group 1), and 45 children with HLI were treated with 1% lindane shampoo and oral trimethoprim/sulfamethoxazole (group 2), and follow-up visits were conducted 2 and 4 weeks later. The children who still had HLI 2 weeks after the primary treatment were treated again. At the 2-week follow-up visit, the treatment success rates of groups 1 and 2 were 76.8% and 86.7%, respectively, and at the 4-week follow-up visit, the rates were 91.3% and 97.8%, respectively. No statistically significant synergistic effect was observed for the combination of a 1% lindane shampoo and oral trimethoprim/sulfamethoxazole.
INTRODUCTION
Head lice infestation (HLI) caused by Pediculus capitis, which has existed for more than 10,000 years, is a common, worldwide problem (Gratz et al., 1997; Chouela et al., 1999; Araujo et al., 2000; Ha et al., 2000). The prevalence of infestation is ubiquitous, particularly among children, however, it is also frequent among adults (Gratz et al., 1997). Therefore, up-to-date the information on the extent of lice infestation is important in order to determine the priority that should be given to control it (Gratz et al., 1997). The head louse is an obligate human parasite, which is transmitted directly by close contact with an infected individual's head or indirectly via fomites such as hair, hats, or combs (Speare, 2000; Bartels et al., 2001). This infestation readily spreads to co-dwelling adults and children, and therefore, presents a public health problem that is difficult to solve. Classmates, playmates, and family members of infested children should be inspected for head lice, and efforts should also be directed to the control of fomites and nits (Elston DM, 1999). Head lice feed by sucking blood and cause pruritus to host due to sensitization to louse saliva, and subsequent skin excoriation may lead to secondary bacterial infections. In addition, chronic irritation and secondary infection may disrupt behavior and school performance (Bailey and Prociv, 2000), and HLI may cause psychological distress (Dodd, 2001; Mumcuoglu, 1999), however, is not considered to be a serious health problem. Nevertheless, HLI consume considerable time and attention of the public and private health communities.
Mechanical removal and pediculocidal agents are often used to treat HLI (Kuwahara and Rasberry, 2001). However, resistance to pediculocidal agents has been reported (Schachner, 1997), and the high prevalence of head lice and consequent heavy use of insecticidal products may explain the rapid increase of resistant strains. Sublethal doses of residual pediculicides may also predispose to resistance (Bailey and Prociv, 2000; Meinking et al., 2001). Patterns of resistance will almost certainly vary geographically, therefore, it is not possible to make an overall estimate of the level of resistance to the various pediculicides in different areas. The choice of treatment depends on local resistance patterns, and whenever treatment failed this should be assessed on a case-by-case basis. It has been known that combination therapy of 1% permethrin with trimethoprim/sulfamethoxazole is effective in cases of lice-related resistance to therapy (Hipolito et al., 2001).
Lindane is a prescription product that kills lice by continuously stimulating the nervous system, but it is also neurotoxic to humans (Gratz et al., 1997; Bartels et al., 2001). On the other hand, trimethoprim/sulfamethoxazole has been reported as an effective treatment for HLI (Hipolito et al., 2001), and it kills lice by destroying symbiotic bacteria which synthesize B group vitamins in the lice gut (Burns, 1987).
Until better agents are available, clinicians may find that rotational or combination treatments with different agents may help to slow the emergence of resistance (Elston, 1999).
This study was undertaken to survey the recent status of HLI in Korean children and evaluate data on the therapeutic efficacy of oral administration of trimethoprim/sulfamethoxazole adding to lindane shampoo.
MATERIALS AND METHODS
Study population
Total of 7,495 children including 3,908 boys and 3,587 girls from kindergarten and 15 primary schools throughout the country were examined for head lice from April 2001 to October 2001. Two schools were in urban areas (one in Seoul and the other in Gyeonggi-do) and the remainder in rural areas (two in Gyeonggi-do, four in Gangwon-do, two in Chungcheongbuk-do, two in Chungcheongnam-do, one in Gyeongsangnam-do, and two in Jeollanam-do). HLI was identified by examining the scalp and hairs for the presence of adult lice, nymphs or viable nits. The viability of nits was confirmed by stereomicroscopic inspection. Viable nits were plump, shiny, and tan to coffee colored with an intact operculum and frequently a pigmented eye-spot. Nits that were empty, shriveled, misshapen, or indented, and those that contained air pockets were considered non-viable (Meinking TL et al., 1986).
Study design
Group 1
A total of 69 children with HLI from 3 schools (one in urban area, Seoul; two in rural areas, Gyeonggi-do) were treated with 1% lindane shampoo (Sinsin Pharm. Co., Seoul, Korea). A quantity sufficient to saturate the hair was applied directly to dry hair and a small amount of water was added to form a good lather. The hair was rinsed with clean water after 10 minutes and towel dried.
Group 2
A total of 45 children with HLI from the same school were treated with a combination of 1% lindane shampoo as described above and trimethoprim/sulfamethoxazole orally administered at a dosage of 8 mg/kg/day based on trimethoprim for 12 days in 2 divided doses.
Follow-up observations and subsequent treatment
Follow-up examinations were carried out 2 and 4 weeks after the initial treatment. Children who still had HLI 2 weeks after the primary treatment were treated again as described above and reexamined at 4 weeks later.
Questionnaire
In 8 of 15 primary schools, children were asked whether or not they were living with both parents. Children were also asked about academic qualifications and jobs of their parents.
Statistical analysis
Statistical analysis of results was performed using the chi-square test. Statistical significance was assumed at a P-value < 0.05.
RESULTS
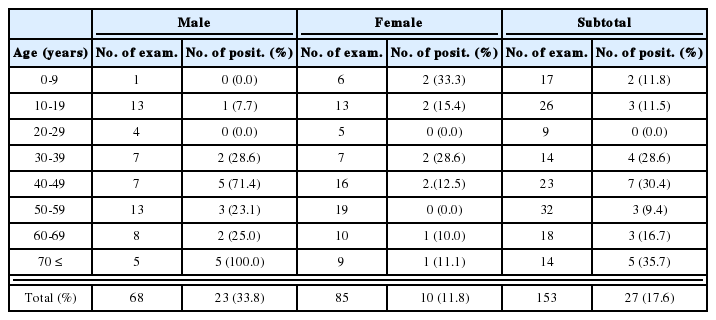
The overall prevalence of HLI was 5.8%, and the rate was higher in rural areas (10.6%) than that in urban areas (3.2%). Head lice were much more commonly detected in girls than in boys with prevalence of 11.2% and 0.9%, respectively (Table 1). The prevalence of HLI by province in urban areas was 2.3% and 4.2% for Seoul and Gyeonggi-do, respectively, and that in rural areas was 10.1%, 9.4%, 5.6%, 14.2%, 5.6%, and 20.2% for Gyeonggi-do, Gangwon-do, Chungcheongbuk-do, Chungcheongnam-do, Gyeongsangnam-do, and Jeollanam-do, respectively (Table 2).
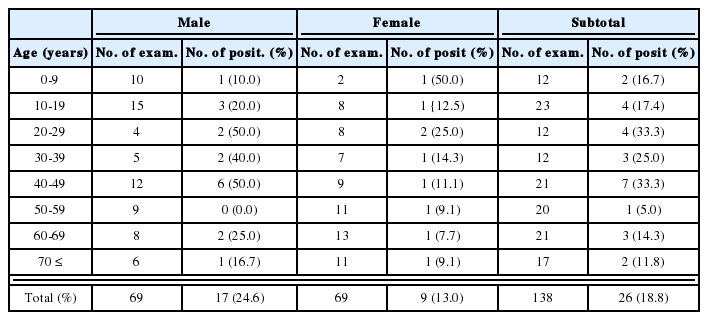
The prevalence of HLI by school grade was 8.0%, 2.9%, 5.4%, 6.4%, 7.6%, 7.9%, and 4.2% for kindergarten, first, second, third, fourth, fifth, and sixth grades, respectively (Table 3).
At 2 weeks after the primary treatment, the success rates of treatment in the groups 1 and 2 were 76.8% and 86.7%, respectively. The success rates of secondary treatment at the 4-week follow-up in the groups 1 and 2 were 91.3% and 97.8%, respectively (Table 4). No statistically significant difference was found between the two groups (P > 0.1). The success rate of the secondary treatment at the 4-week follow-up for each group was higher than that of the primary treatment at the 2-week follow-up (P < 0.05).
Comparison of therapeutic efficacies between 1% lindane shampoo alone (group 1) and a combination of 1% lindane shampoo and oral administration of trimethoprim/sulfamethoxazole (group 2) at 2 weeks and at 4 weeks
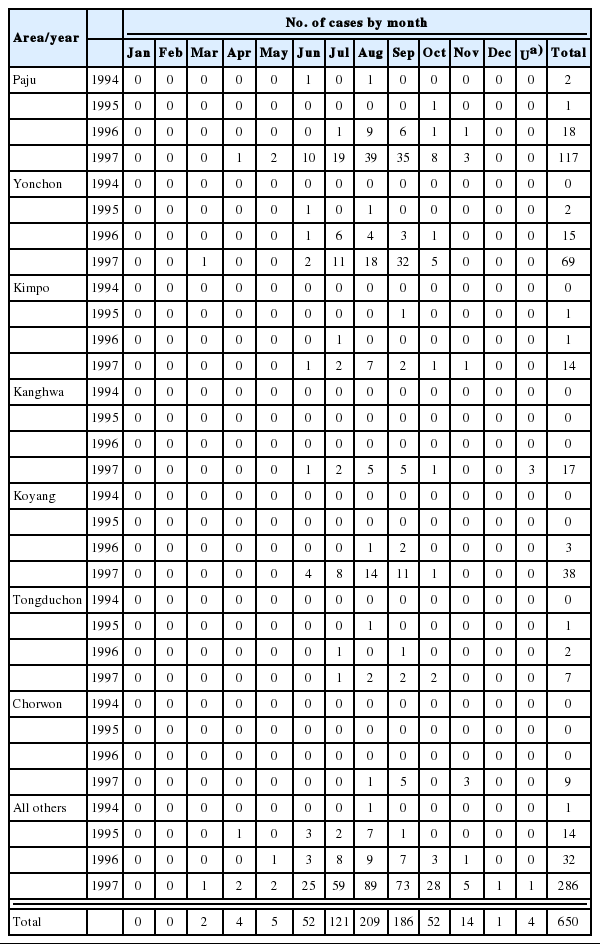
The prevalences of HLI in children living with both parents and those not living with both parents were 6.1% (233/3789) and 14.5% (25/172), respectively (Table 5). Other factors such as parents' academic qualifications and jobs had no statistically significant influence on the prevalence of HLI (P > 0.1) (data not shown).
DISCUSSION
The present study shows that the overall prevalence (5.8%) of HLI in Korea has decreased. In Korea, it was previously reported that the prevalence of pediculosis in urban areas was 5.0% to 40.5% and that in rural areas was 12.8% to 43.6% over the past 10 years (Ree et al., 1992; Huh et al., 1993; Hong et al., 1995; Ha et al., 2000). Improved hygiene, decreased birth rate which reduces the frequency of close contact in the classroom and home, increased economic status, and increased parental concern about children might have resulted in this decrease of HLI. Urban areas had lower prevalence of HLI than rural areas, which is attributed to better hygiene, less time to closely contact friends after school, and frequent change of hairstyles. Girls had a higher infestation rate than boys. Difference in behavior patterns between boys and girls might have affect transmission rates and susceptibility to HLI: These include frequency of personal grooming, close contact with friends and family, frequency of hairstyle changes, shared sleeping environment, shared hair accessories, and hair length.
The infestation rate of kindergarten children was higher than that of any other grade. Kindergarten children are organized into small learning groups and often clustered around a table, where cooperation and sharing are encouraged. This might increase the transmission chance, possibly explaining the higher prevalence among kindergarten children.
The prevalence of HLI among children living with both parents was lower than that among children not living with both parents (P < 0.001), which suggested that childcare was an important factor in the prevalence of HLI.
Of 114 children who received the treatment for HLI, 6 (5.3%) had side effect due to the treatment, one had a mild scalp irritation after application of 1% lindane shampoo, and 5 children had transient abdominal discomfort, diarrhea and/or dizziness due to oral trimethoprim/sulfamethoxazole. However, no major side effect was observed such as CNS toxicity, Stevens-Johnson syndrome, or aplastic anemia.
Pediculus capitis has an incubation period of 6 to 10 days to hatch out, and treatment with closely spaced applications of pediculicides appears to kill adult lice, but does not deal with the possibility of subsequent hatching (Mathias et al., 1984). The 1% lindane shampoo has incomplete ovicidal activity (Brandenburg et al., 1986; Meinking et al., 1986), therefore, we expected to observe a synergistic effect by adding oral trimethoprim/sulfamethoxazole. However, no such statistically significant synergistic effect was observed. In the both groups, the secondary treatment 2 weeks after the primary treatment had marked effect on HLI eradication and although these two applications are expensive, they may significantly reduce the recurrence of HLI.
Educational campaigns by community nurses, public health doctors, and teachers are expected to be helpful for head lice control. It is essential that school authorities and public health centers cooperate to successfully control HLI in primary schools.