Management of malaria in Thailand
Article information
Abstract
The purpose of treatment for uncomplicated malaria is to produce a radical cure using the combination of: artesunate (4 mg/kg/day) plus mefloquine (8 mg/kg day) for 3 days; a fixed dose of artemether and lumefantrine (20/120 mg tablet) named Coartem® (4 tablets twice a day for three days for adults weighing more than 35 kg); quinine 10 mg/kg 8-hourly plus tetracycline 250 mg 6-hourly for 7 days (or doxycycline 200 mg as an alternative to tetracycline once a day for 7 days) in patients aged 8 years and over; Malarone® (in adult 4 tablets daily for 3 days). In treating severe malaria, early diagnosis and treatment with a potent antimalarial drug is recommended to save the patient's life. The antimalarial drugs of choice are: intravenous quinine or a parenteral form of an artemisinin derivative (artesunate i.v./i.m. for 2.4 mg/kg followed by 1.2 mg/kg injection at 12 and 24 hr and then daily for 5 days; artemether i.m. 3.2 mg/kg injection followed by 1.6 mg/kg at 12 and 24 hrs and then daily for 5 days; arteether i.m. (Artemotil®) with the same dose of artemether or artesunate suppository (5 mg/kg) given rectally 12 hourly for 3 days. Oral artemisinin derivatives (artesunate, artemether, and dihydroartemisinin with 4 mg/kg/day) could replace parenteral forms when patients can tolerate oral medication. Oral mefloquine (25 mg/kg divided into two doses 8 hrs apart) should be given at the end of the artemisinin treatment course to reduce recrudescence.
INTRODUCTION
Antimalarial drug resistance can be prevented, or at least delayed. Malaria must be treated adequately and selective pressures should be minimised. Currently recommended methods for assessing drug resistance in high-transmission areas ignores low-grade resistance, however, this is the stage at which preventive measures are most effective. Experimentally, drug resistance can be induced most efficiently by repeatedly reducing the parasite load (in vivo or in vitro) with antimalarial drug treatment that is not sufficient to eradicate. This is what happens in vivo with inadequately treated malaria either as a result of the parasite load inappropriate prescription, poor compliance, or occasionally unusual pharmacokinetic properties of the drug. Factors that contribute to treatment failures depend on three major elements (the host, the agent and the drug) (Table 1). Complete treatment courses with adequate antimalarial doses must be given (Looareesuwan et al., 1992b). For example, in order to ensure eradication of all the parasites, short acting drugs such as artemisinin and its derivatives or quinine are necessary to be present at therapeutic concentrations for at least four asexual cycles (a 7-day treatment course). Drugs which persist for weeks or months at sub-therapeutic levels in the blood cannot offer complete protection no matter how well prescribed. In management of malaria, early diagnosis and treatment with potent antimalarials are the fundamental components of effective strategy. If patients deteriorate, they should be referred to a hospital. Correct use of an effective antimalarial drug will not only shorten the duration of malaria illness, but also reduce the incidence of complications and the risk of death. Antimalarial drug resistance has spread and intensified over the past 40 years leading to a dramatic decline in the efficacy of the most affordable antimalarial drugs (Table 3). Moreover, new drug development has not kept pace, and problems related to the distribution and use of existing drugs have wondered, thus compounding the situation. Therefore, the rational use of artemisinin derivatives in combination with long-acting drugs has now been promoted (Table 3, 4).
USE OF COMBINATION THERAPY
Many countries challenged by endemic malaria are beginning to face a situation in which there are no affordable, effective antimalarial drugs. Combination therapy offers hope for preserving the efficacy of existing antimalarial drugs and prolonging their useful therapeutic usage, although then may not necessarily provide better treatment for consumers. The development of artemisinin and its derivatives, the most rapidly acting of all the current antimalarial drugs, and the recognition of their potential role as a component of combination therapy have led to several large trials aimed at assessing different combinations of existing drugs and to the specific development of new combination drugs. In addition, several countries have been evaluating, drug combinations that do not include artemisinin as potential first-line treatments. These changes have provided the impetus for updating and rationalisation of antimalarial treatment policies.
The potential usefulness of drug combinations, notably those including an artemisinin derivative, to improve efficacy, delay development and selection of drug-resistant parasites, thereby prolonging the useful therapeutic life of existing antimalarial drugs, is widely adopted. Combination therapy is a standard practice in the treatment of other disease such as tuberculosis, various cancers and HIV. The reason behind the combination therapy is that resistance is due to mutations in genes controlling the structure/activity of the therapeutic target. The chance of emergence of a mutant that is simultaneously resistant to two drugs with different action mechanisms is the product of mutation rates to the respective drugs, multiplied by the number of cells exposed to the drugs. Combination of two antimalarial drugs with different modes of action often increases efficacy and protects against the emergence of resistance. Combinations that do not contain an artemisinin derivative could be a preferred option in some countries for the reasons of cost and accessibility. However, the combination of an artemisinin derivative with a long acting antimalarial is preferred, because artemisinin will act on the first part and the residual parasites are cleared by long acting drug (Table 4). Standard doses of both drugs are used. Although there is an increased potential for toxicity, this had not been proved to be a problem in practice. However, combination therapy is a viable option for countries that have already widespread resistance of P. falciparum to chloroquine, amodiaquine, and sulfadoxine-pyrimethamine, provided that the issues of cost and the complexity of implementation can be adequately addressed. More data on factors affecting access to treatment in endemic countries, including health-seeking behavior, should be explored. There is a need for an ongoing system of monitoring antimalarial sensitivity patterns in Southeast Asia, where more accurate information bases and international exchanges are also required. Efforts should be made to intensify the support for resistance monitoring and to develop improved easy-to-use tools, kits and methods to facilitate this activity.
NEW ANTIMALARIAL DRUG TRIALS IN THAILAND
New antimalarial drugs that have been investigated in recent years at the Hospital for Tropical Diseases, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand are as follows (Looareesuwan et al., 1998a; Looareesuwan et al., 1998b): Atovaquone, a hydroxynaphthoquine, was evaluated and it was found that atovaquone alone proved to be safe and effective. All patients treated had clinical cure, however, one third of the patients had late recrudescence (RI). When atovaquone was combined with proguanil, the cure rate increased to 100% (Looareesuwan et al., 1999a; Looareesuwan et al., 1999b). This combination has been developed as a fixed combination drug (Malarone®). Artemisinin derivatives such as artesunate, artemether, arteether and dihydroartemisinin were also tested. Artesunate and artemether alone at a total dose of 600 to 750 mg given over 5-7 days produced 80% to 95% cure rates. However, when combined with mefloquine (1,250 mg total dose) the cure rates increased to 95-100% (Looareesuwan et al., 1992a; Bunnag et al., 1992; Looareesuwan et al., 1997a; Looareesuwan et al., 1997b). Artesunate and dihydroartemisinin suppositories have proved to be successful for the treatment of severe malaria (Looareesuwan et al., 1997c; Looareesuwan et al., 1995; Wilairatana et al., 1997; Wilairatana et al., 2000). The artemisinin derivatives (600-750 mg), when used in combination with mefloquine (1,250 mg) over 3 days in adults, improved cure rates (95-100%). Dihydroartemisinin alone with a total dose of 480 mg given over 5 days gave a cute rate of 90% (Looareesuwan et al., 1996a; Wilairatana et al., 1998). Arteether, a WHO/TDR-supported drug, has been evaluated in the hospital and now has been licensed as Artemotil® for the use in severe malaria (Looareesuwan et al., 2001). Other combinations (artemisinin derivatives combined with lumefantrine or doxycycline and mefloquine combined with tetracycline or doxycycline) have also been evaluated with improvement of cure rates (Looareesuwan et al., 1994a; Looareesuwan et al., 1994b). Recently, a fixed combination drug (artemether puls lumefantrine) named Coartem® (given as six doses on 72 hours) has proved to be a safe and effective drug for the treatment of falciparum malaria and has been authorized for the use in many western countries (Looareesuwan et al., 1999c; van Vugt et al., 1999). At present, studies with combinations of artemisinin derivatives plus mefloquine (in various doses and duration of treatment) are being investigated. In general, artemisinin derivatives (12 mg/kg given over 2-3 days) combined with mefloquine (25 mg/kg total dose) has been a standard regimen for the treatment of multidrug resistant falciparum malaria in Thailand. Until proven otherwise, drug combinations are still remaining the recommended agents for treating patients suffering from acute uncomplicated falciparum malaria contracted in multidrug resistant areas.
MANAGEMENT OF SEVERE MALARIA
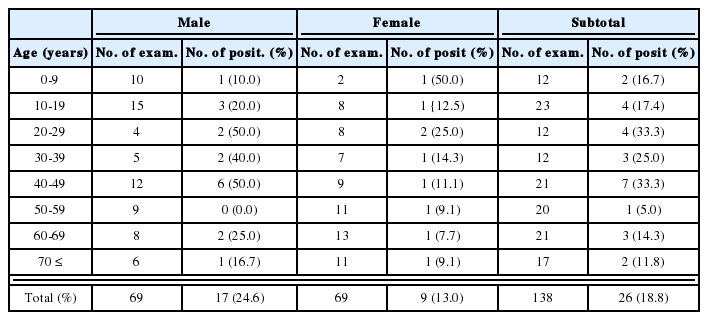
Hospital based data indicates that death from severe falciparum malaria varies from 10-40% depending upon the time lag between initial symptoms and effective treatment and hospital facilities for the management of its complications (WHO, 2000). The disease can progress so rapidly that survival of a patient who is rapidly evolving from uncomplicated malaria and can no longer take oral drugs normally available at the periphery depends upon speedy access of facilities where treatment can be given through the parenteral route. Clinical criterias for referral to a higher level of health care are shown in Table 2. Symptoms associated with malaria where a patient no longer can take drugs by mouth include: repeated vomiting, prostration, obtundation, change in mental status (unable to localize pain or recognize mother), deep breathing, severe anemia, generalized convulsions and coma. Unfortunately facilities for providing parenteral treatment, safely and effectively are not usually quickly accessible to patients.
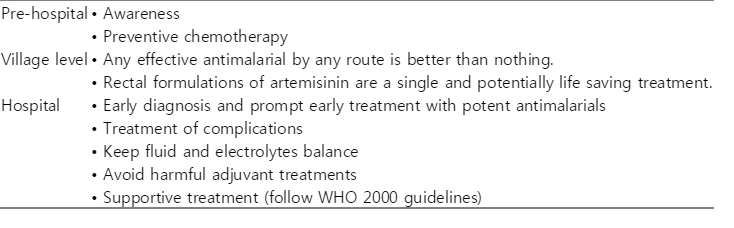
In severe malaria, the choice of antimalarial chemotherapy depends on clinical severity, drug sensitivity of the parasites and the availability and preparation of the drug. It is important to educate medical staff about the clinical features and rapid evaluation of severe disease in febrile patients who may have been exposed to P. falciparum infection. In rural areas of the tropics, where most of the estimated 1-2 million deaths per year form malaria occur, high-risk communities should be made aware of the key symptoms of malaria. Management of severe malaria is listed (Table 6).
Early and appropriate antimalarial chemotherapy may prevent development of severe disease. At the most peripheral level of the health service, oral treatment with tablets or capsules, and suppositories for those who are vomiting, might be useful strategy for local health personnel or village health workers. It is known that discrimination between malaria and acute lower respiratory tract infection is not always possible under these circumstances. Normally, patients who are suspected for severe malaria should be transferred to the highest level of medical care available (Table 2), however, on many occasions, factors such as seasonal flooding, lack of transportation or the condition of the patient may make this impossible.
Early treatment with a potent antimalarial drug preferably by a parental route, is of vital importance. The earlier the treatment started, the better the prognosis. The dose should be calculated by body weight, and the response should be monitored clinically and parasitologically. Patients should be observed for the known side effects of antimalarial drugs, such as hypoglycemia and cardiovascular effects of cinchona alkaloids. Quinine-induced hypoglycemia may develop during recovery several days after the start of treatment, and is particularly common in children and pregnant women. In patients with "algid malaria", the possibility of a concomitant secondary gram negative septicemia should be considered and appropriate antibiotics should be given. In the recovery phase, antimalarial drugs should be given as soon as possible by oral route.
Chloroquine is still the drug of choice for chloroquine-sensitive parasites occurring in some areas of Africa. Quinine and quinidine are the only widely available drugs which are effective against chloroquine-resistant strains. Two new synthetic antimalarial drugs, mefloquine and halofantrine are also effective against chloroquine resistant strains, but they have no parenteral formulation and cases of resistance to these drugs have been reported. Qunghaosu (artemisinin: an ancient Chinese herbal medicine) and its derivatives have been used successfully in treating both uncomplicated and severe falciparum malaria. Their effectiveness in eliminating parasites has been well established, although recrudescence rates can be rather high (10-30%). The recrudescence rate depends upon the dose, duration of artemisinin derivatives used and the severity of disease, and the more severe the dose, the higher the chance of recrudescence. Intravenous/intramuscular artesunate (2.4 mg/kg i.v. or i.m., followed by 1.2 mg/kg injection at 12 and 24 hr, and daily for 5 days) is effective however, not generally readily available in some countries. Intramuscular artemether (3.2 mg/kg i.m. injection followed by 1.6 mg/kg at 12, 24 hr, and then daily for 5 days) is also effective and the drug is generally available in most countries. Recently, intramuscular arteether (Artemotil®) developed by a Dutch company (supported by WHO/TDR) had proved to be safe and effective for the treatment of severe malaria. It is useful in remote areas where intravenous facilities are not available.
WHO/TDR has also concentrated efforts on the potential of artesunate in suppository form to cure parasites rapidly and to reduce significantly the mortality of severe P. falciparum malaria. The potentially life-saving suppository is considerable in two ways: first because the formulation offers the prospect of providing a safe and effective treatment for severe malaria in areas of the rural tropics where parenteral drugs cannot be given. Therefore they can be given at an earlier point in the evolution to severe disease than would normally be the case. Secondly, children and infants are the main beneficiaries; they are most at risk of early death.
POTENTIAL FUTURE DRUGS
The ideal antimalarial drugs should be cheap and well-tolerated efficacious oral drugs that are available as short courses for the treatment of uncomplicated falciparum malaria. For severe malaria, a potent antimalarial drug for either i.v., i.m. or rectal administration is needed. Effective adjunctive therapy should also be investigated.
Most of the antimalarial activity of artemisinin derivatives (but not artemisinin itself) is due to the metabolite dihydroartemisinin. Oral dihydroartemisinin treatment produces cure rates and parasite clearance time equivalent to historical controls treated with oral artesunate. Dihydroartemisinin can be manufactured more cheaply, however, it's pharmacokinetic and pharmocodynamic properties vary greatly. Artelinic acid, currently under development, is a water soluble artemisinin derivative that is more stable in solution than artesunate. Trioxanes, simplified analogues of artemisinin retaining the crucial endoperoxide bridge, are being developed but have not yet entered clinical trials.
Pyronaridine, a Mannich base synthesized by Chinese scientists, is effective in chloroquine-resistant P. falciparum. In Thailand, 28-day follow-up after a 5-day pyronaridine course demonstraed a 12% recrudescence rate (Looareesuwan et al., 1996b), suggesting that is should preferably be used in combination with an artemisinin derivative. Formulaiton and dose optimization studies are in progress.
Two new potent 8-aminoquinolones, tafenoquine and CDRI 80/53, are undergoing clinical trials (Newton et al., 1999; Walsh et al., 1999). Other potential approaches under development include phosphatidylcholine and orotic acid analogues and inhibitors of aspartate and cysteine proteases.