Epidemiologic characteristics of malaria in non-malarious area, Jeollabuk-do, Korea in 2000
Article information
Abstract
In South Korea, the north border area has been under vivax malaria epidemic since 1993. However, Jeollabuk-do, which is about 300 kms from the border, has not experienced the same epidemic. I investigated a total of 58 notified cases of malaria in Jeollabuk-do in the year 2000. All of the cases had an exposure history in the epidemic area. Among them were 49 ex-soldiers, 3 soldiers who served near the border area and 6 civilians who traveled there. The causal agent of all cases was Plasmodium vivax. Except the civilians, the soldiers and ex-soldiers were aged in their twenty's. In the present study, the incubation period was from 6 to 520 days with a median of 157 days, and the latent onset type (92%) was more prevalent than the early onset type. Illness onset of most cases (86%) peaked during the summer season (June to September) despite of variable incubation periods. The time lag for diagnosis ranged from 2 to 42 days with a median of 11 days. Jeollabuk-do has not been an area of epidemic untill now, but incidences have been increasing annually since 1996. In Jeollabuk-do, early diagnosis and treatment can be a feasible disease control measure to prevent spreading from the epidemic area.
INTRODUCTION
Plasmodium vivax malaria re-emerged first in 1993 in Korea (Cho et al., 1994). After that initial re-emergence, the number of vivax malaria cases has been increased annually in the north border area. In the year 2000, a total of 4,142 cases were notified nationwidely. In the epidemic area specified by National Institute of Health of Korea, where incidence (number of cases per 100,000 per year) was higher than 10 cases, disease control measures including mosquito control, early diagnosis and treatment were introduced already. In the non-epidemic area, however, the disease control measures were somewhat relaxed compared with those in the epidemic area. In Jeollabuk-do about 300 kms away from the border area, one case of re-emerging vivax malaria was first reported in 1996. Although the number of cases and incidences in Jeollabuk-do has been increasing every year (7 cases in 1997, 29 cases in 1998, 43 cases in 1999 and 58 cases in 2000), characteristics of this malaria epidemic in Jeollabuk-do were not yet well known. Since epidemiologic information provide the clue of adequate control measures of an epidemic, I analyzed the notified cases in Jeollabuk-do in year 2000 for establishing the disease control measures that are presently required.
MATERIALS AND METHODS
Since malaria is the class III notifiable disease in Korea, every clinician is obliged to notify malaria cases confirmed by blood smear to the public health authorities. In Jeollabuk-do 14 public health centers are located in each 14 cities or counties. Public health center authorities must report the notified cases to provincial epidemiologist in Jeonju by an electronic data interchange (EDI) system. The reporting abstract form consisted of name, age, sex, address, occupation, day of illness onset, day of diagnosis, estimated exposure site and date. I analyzed malaria cases reported in the year 2000. An independent t-test was done with a data analysis program SPSS 8.0. The p value less than 0.05 was accepted as statistically significant.
RESULTS
Demographic characteristics
Of a total 58 cases, there were 55 cases involving males and 3 cases of females. The age distribution showed that 54 cases were in their twenty's, 2 cases in their thirty's, 1 case each in their forty's and another in their fifty's. Occupations classified by military status were as follows: 49 cases of ex-soldiers, 3 cases of soldiers and 6 cases involving civilians. Addresses of the cases were 41 cases at 3 urban cities (Jeonju, Gunsan and Iksan) and 17 cases at 7 rural counties. The number of cases in urban areas was more than that in rural areas. However, no significant difference (p = 0.125) was shown in the incidences between both areas. The highest incidence was 5.2 in Gochang located in the southwestern part of the province. The average incidence in Jeollabuk-do was 2.9 (Table 1).
Monthly distribution, exposure site and incubation period
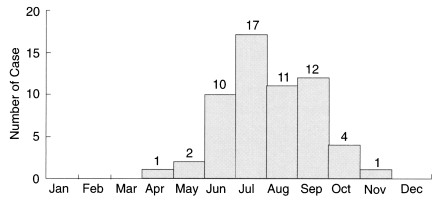
Onset of illness in 48 cases (86%) showed a peak during summer season (June to September) despite of variable long incubation periods (Fig. 1). In the cases of ex-soldiers or soldiers there were no exact way for detecting the exposure date or site because the site and schedule of military training or travelling were changed frequently. Because it was impossible to estimate the incubation period, I regarded the exposure time to be the date of retiring from military service, leaving the military service or returning from the travel, and exposure site as the area of the last service duty or travelling. All cases had a history of serving at or travelling to the epidemic border area (Table 2). The estimated exposure site was mainly the demilitarized zone facing the North Korea border. There was no locally acquired case in Jeollabuk-do. An estimated incubation period of total 58 cases ranged from 6 to 520 days with a median of 157 days. Only 4 cases had short incubation periods (illness onset within 14 days after exposure), 52 cases (92%) had long incubation periods and 2 cases were ill before retiring from military service. As for the 6 civilian cases, date of travel to epidemic area and exposure time could be estimated easily. The incubation periods of 6 cases were 10, 240, 285, 317, 345 and 375 days with a mean of 301 days. So 5 cases had long and only one case had short incubation period.
Time lag for diagnosis
Among a total of 58 cases, dates of onset and diagnosis in 57 cases were informed. The time lag for diagnosis was analyzed. The median time lag for diagnosis was 11 days and the mean was 13 days. The mean of time lag for diagnosis of cases was 12 days in urban areas and 16 days in rural areas. The statistical difference between both areas was not significant (p = 0.214).
DISCUSSION
Malaria cases in Jeollabuk-do have similarities in epidemiologic features of national study, which investigated the cases of ex-soldiers and civilians in 1999 (Yang, 2000). In that study, areas of incidence above 10 (per 100,000 per year) were Gyeonggi-do, Gangwon-do and Incheon metropolitan city bordering North Korea. However, in those areas, only 13 counties (gun) had more than 10 cases. The incidences in the top five counties were 409 in Yeoncheon, 223 in Ganghwa, 221 in Cheorwon, 165 in Paju and 78 in Gimpo in order. The incidences in other provinces and metropolitan cities were less than 5 cases.
The incubation period in the cases of ex-soldiers had a median 180 days in 1999 (Yang, 2000). Lee et al. (1998) reported that the mean incubation period was 279 days in 239 ex-soldiers, which occurred from 1994 to 1997. This was longer than the median 157 days of Jeollabuk-do cases, but it should be noted that it was impossible to estimate the exact incubation period in the soldiers, ex-soldiers and residents in the epidemic area. The actual incubation period was estimated to be longer than estimated before. In my cases, the incubation periods of travellers (civilians) to the epidemic area were longer than total cases. Although the incubation period was somewhat different in each reported case, long incubation type was dominant in Korea. Shute et al. (1977) explained that a North Korean strain of Plasmodium vivax in Korea had long incubation periods shown by the experiment, and he established the most satisfactory theory based on the presumed existence of two populations of sporozoites in P. vivax. Krotoski (1989) supported this theory that a single, successful sporozoite can yield a parasitemic relapse and defines each major strain grouping, although the actual proportion of each sporozoite/ hypnozoite type within strains depicted was unknown, Liu et al. (1995) found that the temperature of environment contribute to the proportion of hypnozoites in total number of extraerythrocytic forms by experiment. The proportion of hypnozoites in laboratory hepatocytes is higher in low temperature, and Shu et al. (1995) also found that P. vivax isolates of various areas in China classified by the latitude more than 5 degrees were significantly different in the proportion of hypnozoite. He concluded that the percentages of hypnozoites are positively correlated with the latitude. In recent molecular biologic study, Li et al. (2001) categorized P. vivax according to developmental success in Anopheles albimanus, and they mentioned that separate types of P. vivax require taxonomic distinction. Such molecular study can be applied to classify the subspecies' distinct in incubation period.
Illness of most cases (86%) in Jeollabuk-do peaked in June to September, and most cases out of the total nationwide cases in 1997 (Feighner et al., 1998) and 1999 (Yang, 2000) began to occur in May to October. Despite variable long incubation period of cases in Korea, the reason why the illness' onset converged into summer time is yet unknown. It is suggested that other biological factors in hosts or causal agents may be involved in selecting the season of illness. Further study is required for solving that enigma.
The time from onset of illness to diagnosis was somewhat longer in Jeollabuk-do (median 11 days) than that of the whole nation (median 7 days) (Yang, 2000). Feighner et al. (1998) reported that the required time of diagnosis of the US army in Korea was a median of 5 days. These reports suggested that the time lag for diagnosis can be shorter than before.
In conclusion, Jeollabuk-do's early diagnosis and treatment can be feasible and be implemented now prior to mosquito control. Therefore, the source of infection (index case) can be eliminated early to prevent the occurrence of the introduced case. Locally acquired cases, which had no history of travelling to the epidemic areas, were suspected in non-malarious area (Yang, 2000). Investigation should be done for the evaluation of the current status of this malaria epidemic in Korea for locally acquired cases (Bradley et al., 2000).
ACKNOWLEDGEMENTS
The author would like to thank Dr. Hong-Bin Kim, Epidemic Intelligence Service (EIS) officer at National Institute of Health of Korea for his helpful advice about malaria epidemiology, and is indepted to members of the epidemic control teams at public health centers in Jeollabuk-do for investigating each case.