Border malaria characters of reemerging vivax malaria in the Republic of Korea
Article information
Abstract
Since 1993, the number of vivax malaria cases has increased every year in the northern part of the Republic of Korea (ROK). This study was designed to characterize factors related to the reemergence of malaria in the ROK. A total of 21 cases diagnosed in 1993 and 1994 distributed sporadically in the narrow zone along the demilitarized zone (DMZ). Of total 317 civilian inhabitant cases reported in 1994-1997, 287 cases were studied and 80.8% of them resided within 10 km from the southern border of the DMZ. The frequency distribution of anti-Plasmodium vivax antibody titers using indirect fluorescent antibody test was compared in three villages in relation with distance from the DMZ. The number of inhabitants with high antibody titers was larger in the village nearest to the border than that in more distant villages. The present results highly suggested that the reemerging vivax malaria start in the border area, most possibly caused by infected mosquitoes which flew across the border. This pattern of transmission repeated year after year.
INTRODUCTION
Malaria is the most important tropical disease putting more than half of the world's population at risk with 200 million estimated cases and two million deaths each year. Recently, Plasmodium vivax malaria has reemerged or resurged in several countries including India, Peru, and China (Gubler, 1998; Sleigh, 1998). In the Republic of Korea (ROK), vivax malaria has also reemerged after being absent for more than 10 years. The number of vivax malaria cases has been increased: one in 1993, 20 in 1994, 107 in 1995, 356 in 1996, 1713 in 1997 (Kim et al., 1998; Lee et al., 1998).
Since it was widely believed that indigenous vivax malaria was completely eradicated in the ROK during the mid-1970s and early 1980s (Paik et al., 1988), an explanation that the source of infection persists within the territory of the ROK is unlicely. From the beginning of the present epidemic, several possibilities have been suggested to explain the source of reemerging infection. Since all the initial cases did not originate from abroad, the possibility of foreign contraction could be eliminated (Chai et al., 1994; Cho et al., 1994). An alternative explanation could be that foreign immigrants themselves were carriers who were from malaria endemic countries (Chai et al., 1994). Cho et al. (1994) and Ree (1998) also suggested a different possibility that infected mosquitoes across the demilitarized zone (DMZ) could initiate the spread of malaria.
Some epidemiological studies including case analysis and entomological investigation have been undertaken (Yim et al., 1996; Shim et al., 1997; Kim et al., 1998; Lee et al., 1998). However, the origin of present epidemic is still unclear. To undertake a successful control measure, it is very important to identify the origin and the path of transmission. Therefore, this study was designed to find out the factors related to reemerging vivax malaria in the ROK.
MATERIALS AND METHODS
Geographical distribution of cases detected in 1993 and 1994
To trace the origin of the present epidemic, the time-space distribution of initial cases based on their date of onset and their residential places was analyzed. A total of 21 vivax malaria cases was reported in 1993 and 1994. Eighteen were in the military service, two were local civilian inhabitants, and one was an ex-soldier. Giemsa stained blood smear of those cases were re-examined. All of them were positive for P. vivax infection. A few questions were asked to the patients, including their onset of illness, their activities, and locality during 3 years since the onset of illness, etc. From the interview, the locations where they contracted malaria were determined. The locations were marked on a map with numbers showing the chronological order based on the date of onset.
Geographical distribution of civilian inhabitant cases detected in 1994-1997
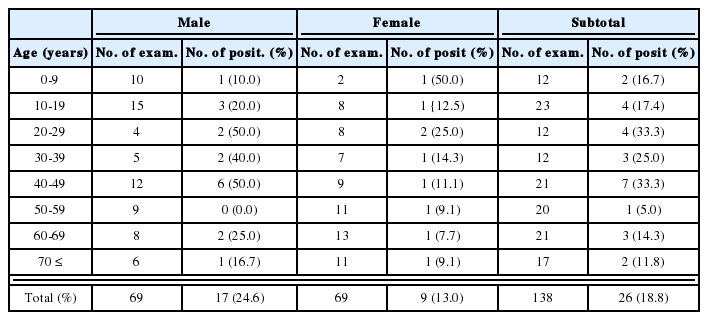
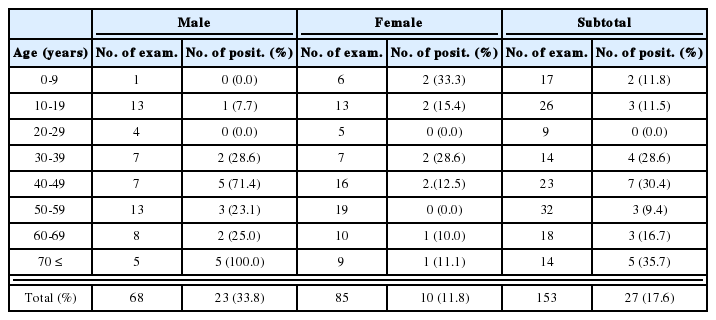
To characterize the pattern of malaria transmission in the present epidemic, time-space distribution of cases reported in 1994-1997 was also analyzed. In the period, a total of 2,219 vivax malaria cases, including military cases, was reported to the government. Among 650 civilian cases, 317 cases were inhabitants of the endemic areas in the northern part of Kyonggi-do or western Kangwon-do. The other 333 civilian cases were ex-soldiers, travelers, or workers who passed through the endemic areas (Lee et al., 1998). These civilian cases and all the military cases were excluded in this study because the sites of their location were not as exact as we required mapping. Of the 317 civilian inhabitant cases, 30 had no exact addresses and they were also excluded in this study (Table 1). The residences of 287 inhabitant cases were plotted on a map. Because all the subjected cases were located within 20 km from the southern border of DMZ, the 20 km zone was divided into four sectors by 5 km wide to show the relationship between transmission of malaria and the distance from the MZ.
Seroepidemiologic study
To estimate the intensity of transmission in relation with distance from the DMZ, the frequency distribution of anti-P. vivax antibody titers in three villages were compared. Together with Yonchon-gun (county), Paju-gun is one of the most prevalent areas in the present epidemic. Therefore, the seroepidemiologic study was carried out in Pajugun. The study area is located in the northern part of ROK lying between latitude 37°43'N and 38°00'N, longitude 126°45'E and 127°00'E. It is bordered on its west side by Hangang (River) and Imjingang (River). Between December 1997 and January 1998, blood specimens of inhabitants were collected from three villages, which were Majong-ri, Munsan-ri, and Sinsan-ri (Fig. 1). The shortest distance between DMZ and each village is 2 km (Majong-ri), 2.3 km (Munsan-ri), and 7.3 km (Sinsan-ri). In collaboration with local health centers, 90 blood samples were collected from Majong-ri, 91 from Munsan-ri, and 88 from Sinsan-ri, respectively. The subjects came from all age and both sexes. The mean age (range) of subjects in each village was 53.97 (5-82) in Majong-ri, 34.91 (2-82) in Munsan-ri, and 37.34 (5-75) in Sinsan-ri, respectively. The sex ratio (male to female) was 0.91 in Majong-ri, 0.60 in Munsan-ri, and 0.73 in Sinsan-ri, respectively. They were asked a couple of questions regarding their age, sex, and recent history of fever. Blood smears were examined by microscopy after Diff-Quik staining. Sera were subjected to the indirect fluorescent antibody test (IFAT).
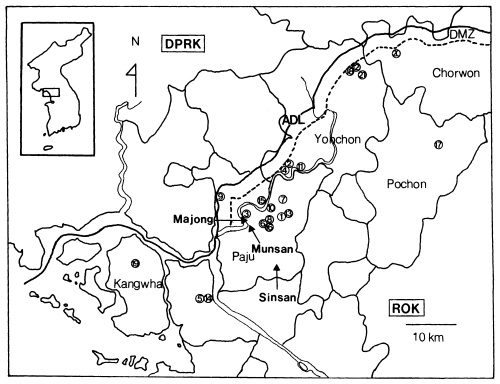
Geographical distribution of vivax malaria cases detected in 1993 and 1994. The locality of each case is numbered in a circle (○) sequentially according to the onset date of illness. The localities where the sero-epidemiology was carried out are marked with triangle (▲). ADL, armistice demarcation line; DMZ, demilitarized zone; ROK, Republic of Korea; DPRK, Democratic People's Republic of Korea.
The IFAT was carried out according to a modified method of Voller and O'Neill (1971). Briefly, a two-fold dilution system was applied to each sample. The samples at each dilution were overlaid on P. vivax antigen spots prepared on glass slides. The antigen was prepared from infected blood of a patient who had contracted vivax malaria in ROK. After incubation and washing, fluorescein conjugated rabbit anti-human IgG (Sigma, St. Louis, USA) (diluted to 1:30) was placed on each spot. Following the final washing, titers were determined by reading with an incident light illuminating type fluorescent microscope.
RESULTS
Geographical distribution of cases detected in 1993 and 1994
The area of interest lies between latitude 37°31'N and 38°24'N, longitude 126°04'E and 127°27'E. All the cases were distributed in a narrow zone, less than 20 km in width and about 125 km in length. The zone lay from west to east, along the DMZ, from Kangwha-gun, Kyonggi-do to Chorwon-gun, Kangwon-do. The cases were detected in six counties (guns); Kangwha, Kimpo, Paju, Yonchon, Pochon, and Chorwon-gun (Fig. 1). Infected soldiers were restricted to their areas because of their military duty. Two female civilian patients denied leaving their hometown for several years.
Geographical distribution of civilian inhabitant cases detected in 1994-1997
The studied cases were residents of Kanghwa, Kimpo, Koyang, Paju, Yonchon, Pochon, Chorwon, Yangju-gun, and Tongduchon-shi. Most cases (75.9%) were localized in Paju and Yonchon (Fig. 2; Table 2). The localities of inhabitant cases distributed along the DMZ. During 1994-1997, 232 inhabitant cases (80.8%) resided within 10 km from the southern border of the DMZ. Forty two cases (14.6%) were residing between 10 km and 15 km from the border, and 13 (4.5%) residing over 15 km from the border (Fig. 2; Table 3).
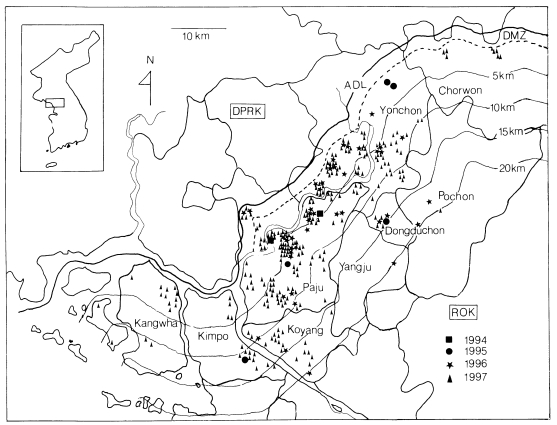
Distribution of 278 civilian inhabitant cases of vivax malaria in 1994-1997. The residences of each case is marked. Among 278 cases, 232 (80.8%) were detected within 10 km from the southern border of the demilitarized zone (DMZ). ADL, armistice demarcation line; ROK, Republic of Korea; DPRK, Democratic People's Republic of Korea.
Distribution of the subjected civilian inhabitant cases of vivax malaria, presented by the counties, 1994-1997
Seroepidemiology
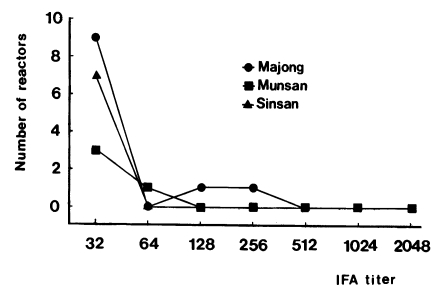
Antibody titer of 1:32 or higher was regarded as sero-positive. The sero-positive rates were 12.2% in Majong-ri, 4.4% in Munsan-ri, and 8.0% in Sinsan-ri, respectively. The frequency distribution curves of the IFA titers in each examined village are shown in Fig. 3. The IFA titers of subjects were relatively low (1:32-1:512). All of the studied people were negative for malaria parasites by the microscopic examination.
DISCUSSION
Concerning the origin of infection which led into the present epidemic, two major possibilities have been discussed (Chai et al., 1994; Cho et al., 1994; Ree et al., 1998). The first possibility was that undiagnosed imported malaria cases provided a nidus for reestablishment of this epidemic. In the ROK, immigrant of workers from malaria endemic countries began to increase since the early 1990s. This possibility should be considered. The second possibility is that the cases were infected malaria by mosquito that came across the DMZ. The geographical and chronological occurrence patterns of initial three cases and the ecologically favorable conditions for malaria transmission in this area back up this possibility (Cho et al., 1994).
The results of the present study strongly support the second possibility. First of all, the time-space distribution of cases detected in 1993 and 1994 shows that malaria occurred sporadically in a vertically narrow and horizontally wide zone along the DMZ during a relatively short period. If this epidemic originated from one or several sources of infection, the geographical distribution of initial cases would spread from one or more foci. However, the initial cases distributed diffusely in the area 125 km in length after two short transmission seasons. Furthermore, most of the patients were restricted to their areas. Therefore, this distribution can be explained only when large number of mosquitoes, which flew from endemic areas near the present endemic areas, attacked simultaneously the present endemic area in the ROK.
Second, the cases were more concentrated in areas closer to the DMZ as shown in the distribution map of civilian inhabitant cases, which were detected during 1994-1997. This pattern of distribution repeated year after year. Besides civilian inhabitant cases, 70.4% of the total cases detected in the same period were military soldiers. Including ex-soldiers, 81.3% of the total cases contracted malaria during their military service (Lee et al., 1998). During 1994-1997, all the military cases had histories of services in or near the DMZ during malaria transmission seasons (Kim et al., 1998). These findings meant that almost all cases contracted malaria near the DMZ.
Furthermore, the sero-positive rate of people was relatively higher in the village closest to the DMZ. As shown in frequency distribution curves of IFA titer, the titer was very low. The number of inhabitants with high antibody titer was larger in the village nearest to the DMZ than in more distant villages. When transmission of malaria in an area is increasing, the number of the high titer reactor is also increasing (Suzuki, 1991). Our result in the present study meant that the malaria was more actively transmitted in the villages near the DMZ. Above results suggest that people in the area near the DMZ more easily contract malaria than those in areas further from the DMZ.
Our results of the case detection surveillance, distribution, and seroepidemiological findings highly suggested that the reemerging vivax malaria start in the border area, most possibly caused by infected mosquitoes which flew across the border. This pattern of transmission occurred repeatedly year after year.
Notes
This study was supported by a grant (HMP-96-M-2-1057) of Good Health R & D Project, Ministry of Health and Welfare, Republic of Korea and also supported by a Research Grant of Japan Health Sciences Foundation, Japan.