Cited By
Citations to this article as recorded by

Leukotriene B4 receptors BLT1 and BLT2 are involved in interleukin-8 production in human neutrophils induced by Trichomonas vaginalis-derived secretory products
Young Hee Nam, Arim Min, Seong Hoon Kim, Young Ah Lee, Kyeong Ah Kim, Kyoung-Ju Song, Myeong Heon Shin
Inflammation Research.2012; 61(2): 97.
CrossRef Trichomonas vaginalis triggers the release of THP-1 extracellular traps
Li Fei, Wei Zhengkai, Jiang Weina, Cao Lili, Gao Yuhang, Yang Zhengtao, Li Jianhua, Yu Biao, Zhang Xichen, Gong Pengtao
Parasitology Research.2019; 118(1): 267.
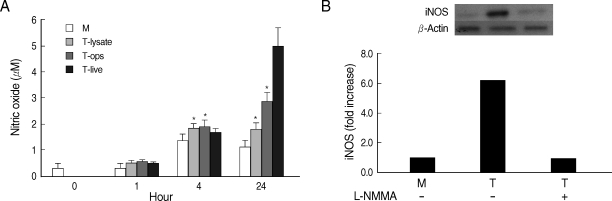
CrossRef Involvement of purinergic signaling on nitric oxide production by neutrophils stimulated with Trichomonas vaginalis
Amanda Piccoli Frasson, Geraldo Attilio De Carli, Carla Denise Bonan, Tiana Tasca
Purinergic Signalling.2012; 8(1): 1.
CrossRef Adenosine reduces reactive oxygen species and interleukin-8 production by Trichomonas vaginalis-stimulated neutrophils
Amanda Piccoli Frasson, Camila Braz Menezes, Gustavo Krumel Goelzer, Simone Cristina Baggio Gnoatto, Solange Cristina Garcia, Tiana Tasca
Purinergic Signalling.2017; 13(4): 569.
CrossRef Impact of microparticles released during murine systemic inflammation on macrophage activity and reactive nitrogen species regulation
Weronika Ortmann, Anna Such, Elzbieta Kolaczkowska
Immunologic Research.2024; 72(2): 299.
CrossRef Trichomoniasis immunity and the involvement of the purinergic signaling
Camila Braz Menezes, Tiana Tasca
Biomedical Journal.2016; 39(4): 234.
CrossRef Local cytokine/chemokine profiles in BALB/c and C57BL/6 mice in response to T. vaginalis infection
Sonal Yadav, Vivek Verma, Rakesh Singh Dhanda, Sumeeta Khurana, Manisha Yadav
Experimental Parasitology.2022; 239: 108287.
CrossRef Leukotriene B4 receptor BLT-mediated phosphorylation of NF-κB and CREB is involved in IL-8 production in human mast cells induced by Trichomonas vaginalis-derived secretory products
Young Hee Nam, Deulle Min, Hyoung-Pyo Kim, Kyoung-Ju Song, Kyeong Ah Kim, Young Ah Lee, Seong Hoon Kim, Myeong Heon Shin
Microbes and Infection.2011; 13(14-15): 1211.
CrossRef BLT1-mediated O-GlcNAcylation is required for NOX2-dependent migration, exocytotic degranulation and IL-8 release of human mast cell induced by Trichomonas vaginalis-secreted LTB4
Arim Min, Young Ah Lee, Kyeong Ah Kim, Myeong Heon Shin
Microbes and Infection.2018; 20(6): 376.
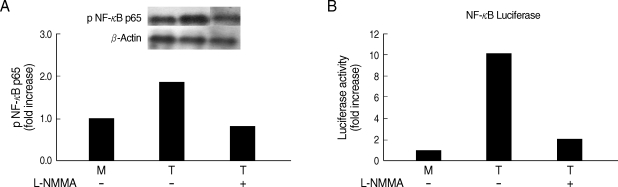
CrossRef Effect of iNOS inhibitor LNMMA along with antibiotics Chloramphenicol or Ofloxacin in murine peritoneal macrophages regulates S.aureus infection as well as inflammation: An in vitro study
Somrita Dey, Biswadev Bishayi
Microbial Pathogenesis.2017; 105: 307.
CrossRef OsmC and incomplete glycine decarboxylase complex mediate reductive detoxification of peroxides in hydrogenosomes of Trichomonas vaginalis
Eva Nývltová, Tamara Smutná, Jan Tachezy, Ivan Hrdý
Molecular and Biochemical Parasitology.2016; 206(1-2): 29.
CrossRef ReducedTrichomonas vaginalisviability in mice pretreated with parasite DNA
Marco Antonio Barajas-Mendiola, Laura E. Castellano, Miriam Barrios-Rodiles, Martha A. Deveze-Alvarez, Eva E. Avila, Patricia Cuéllar-Mata
Parasitology.2019; 146(13): 1636.
CrossRef Immune cell arrival kinetics to peritoneum and role during murine-experimental trichomoniasis
F. J. Rangel-Mata, E. E. Ávila-Muro, J. E. Reyes-Martínez, L. M. Olmos-Ortiz, M. E. Brunck, L. A. Arriaga-Pizano, P. Cuéllar-Mata
Parasitology.2021; 148(13): 1624.
CrossRef In Vitro Activation of Macrophages by an MHC Class II-restricted Trichomonas Vaginalis TvZIP8-derived Synthetic Peptide
Victor Ermilo Arana-Argáez, Emanuel Ceballos-Góngora, María Elizbeth Alvarez-Sánchez, Antonio Euan-Canto, Julio Lara-Riegos, Julio César Torres-Romero
Immunological Investigations.2022; 51(1): 88.
CrossRef IL‐22 Levels are Associated with Trichomonas vaginalis Infection in the Lower Genital Tract
Hadijat Moradeke Makinde, Reza Zariffard, Paria Mirmonsef, Richard M Novak, Olamide Jarrett, Alan L Landay, Gregory T Spear
American Journal of Reproductive Immunology.2013; 70(1): 38.
CrossRef The anti‐Trichomonas vaginalis phloroglucinol derivative isoaustrobrasilol B modulates extracellular nucleotide hydrolysis
Camila Braz Menezes, Graziela Vargas Rigo, Henrique Bridi, Danielle da Silva Trentin, Alexandre José Macedo, Gilsane Lino von Poser, Tiana Tasca
Chemical Biology & Drug Design.2017; 90(5): 811.
CrossRef Involvement of mast cells in inflammation induced by Trichomonas vaginalis via crosstalk with vaginal epithelial cells
I. H. HAN, S. J. PARK, M. H. AHN, J. S. RYU
Parasite Immunology.2012; 34(1): 8.
CrossRef Immunity in urogenital protozoa
N. Malla, K. Goyal, R. S. Dhanda, M. Yadav
Parasite Immunology.2014; 36(9): 400.
CrossRef Trichomonas vaginalis exosome‐like vesicles modify the cytokine profile and reduce inflammation in parasite‐infected mice
L. M. Olmos‐Ortiz, M. A. Barajas‐Mendiola, M. Barrios‐Rodiles, L. E. Castellano, S. Arias‐Negrete, E. E. Avila, P. Cuéllar‐Mata
Parasite Immunology.2017;[Epub]
CrossRef Humoral and T cell–mediated immune response against trichomoniasis
M. Nemati, N. Malla, M. Yadav, H. Khorramdelazad, A. Jafarzadeh
Parasite Immunology.2018;[Epub]
CrossRef Inflammatory responses during trichomoniasis: The role of Toll‐like receptors and inflammasomes
Abdollah Jafarzadeh, Maryam Nemati, Ehsan Salarkia, Sonal Yadav, Najmeh Aminizadeh, Sara Jafarzadeh, Manisha Yadav
Parasite Immunology.2023;[Epub]
CrossRef Activation of murine macrophages by membrane proteins from Tritrichomonas foetus grown on iron‐ and calcium‐rich conditions
Antonio Euan‐Canto, Julio César Torres‐Romero, María Elizbeth Alvarez‐Sánchez, Victor Ermilo Arana‐Argáez, Karla Acosta‐Viana, Emanuel Ceballos‐Góngora, Laura Vázquez‐Carrillo, Leidi Alvarez‐Sánchez
Parasite Immunology.2024;[Epub]
CrossRef Heterogeneous macrophages: Supersensors of exogenous inducing factors
Caiyun Qian, Zehui Yun, Yudi Yao, Minghua Cao, Qiang Liu, Song Hu, Shuhua Zhang, Daya Luo
Scandinavian Journal of Immunology.2019;[Epub]
CrossRef
SNAP23-Dependent Surface Translocation of Leukotriene B
4
(LTB
4
) Receptor 1 Is Essential for NOX2-Mediated Exocytotic Degranulation in Human Mast Cells Induced by Trichomonas vaginalis-Secrete
Arim Min, Young Ah Lee, Kyeong Ah Kim, Jamel El-Benna, Myeong Heon Shin, Judith A. Appleton
Infection and Immunity.2017;[Epub]
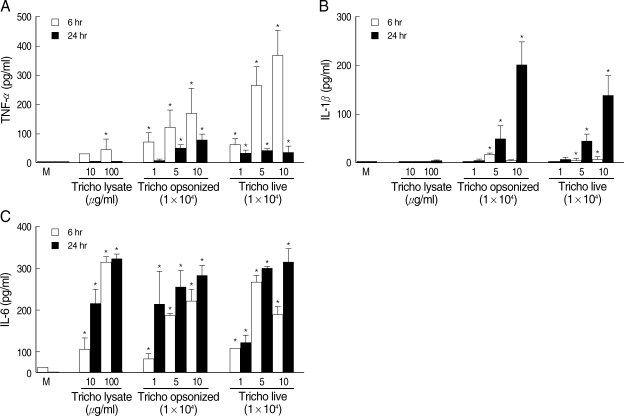
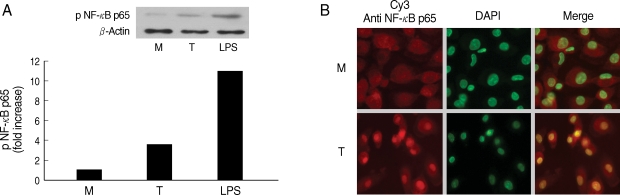
CrossRef Differential Regulation of Proinflammatory Cytokine Expression by Mitogen-Activated Protein Kinases in Macrophages in Response to Intestinal Parasite Infection
Mei Xing Lim, Chin Wen Png, Crispina Yan Bing Tay, Joshua Ding Wei Teo, Huipeng Jiao, Norbert Lehming, Kevin Shyong Wei Tan, Yongliang Zhang, J. A. Appleton
Infection and Immunity.2014; 82(11): 4789.
CrossRef Analysis of the Oxidative Stress Status in Nonspecific Vaginitis and Its Role in Vaginal Epithelial Cells Apoptosis
Zhaojie Chen, Zhen Zhang, Haiyan Zhang, Beibei Xie
BioMed Research International.2015; 2015: 1.
CrossRef Trichomonas vaginalis Induces NLRP3 Inflammasome Activation and Pyroptotic Cell Death in Human Macrophages
Angelica Montenegro Riestra, J. Andrés Valderrama, Kathryn A. Patras, Sharon D. Booth, Xing Yen Quek, Chih-Ming Tsai, Victor Nizet
Journal of Innate Immunity.2019; 11(1): 86.
CrossRef T. vaginalis Infection Is Associated with Increased IL-8 and TNFr1 Levels but with the Absence of CD38 and HLADR Activation in the Cervix of ESN
Olamide D. Jarrett, Kirsten E. Brady, Sharada P. Modur, Jill Plants, Alan L. Landay, Mahmood Ghassemi, Elizabeth T. Golub, Greg T. Spear, Richard M. Novak, Clive M. Gray
PLOS ONE.2015; 10(6): e0130146.
CrossRef Prostatic Disease Associated withTrichomonas vaginalis
Jae-Sook Ryu
The Korean Journal of Urogenital Tract Infection and Inflammation.2014; 9(2): 61.
CrossRef IL-10 release by bovine epithelial cells cultured with Trichomonas vaginalis and Tritrichomonas foetus
Ricardo Chaves Vilela, Marlene Benchimol
Memórias do Instituto Oswaldo Cruz.2013; 108(1): 110.
CrossRef NF-κB and CREB Are Involved in IL-8 Production of Human Neutrophils Induced byTrichomonas vaginalis-Derived Secretory Products
Young Hee Nam, Deulle Min, Soon-Jung Park, Kyeong Ah Kim, Young Ah Lee, Myeong Heon Shin
The Korean Journal of Parasitology.2011; 49(3): 291.
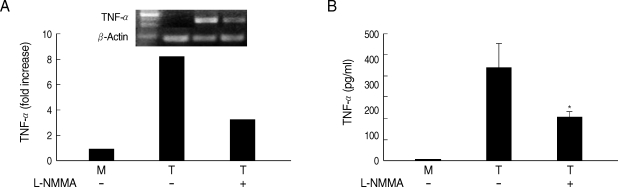
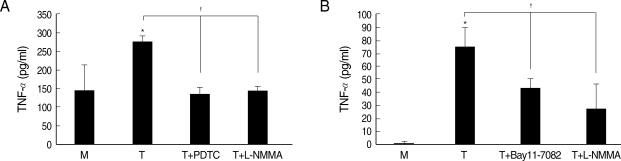
CrossRef Involvement of PI3K/AKT and MAPK Pathways for TNF-α Production in SiHa Cervical Mucosal Epithelial Cells Infected with <i>Trichomonas vaginalis</i>
Jung-Bo Yang, Juan-Hua Quan, Ye-Eun Kim, Yun-Ee Rhee, Byung-Hyun Kang, In-Wook Choi, Guang-Ho Cha, Jae-Min Yuk, Young-Ha Lee
The Korean Journal of Parasitology.2015; 53(4): 371.
CrossRef Trichomonas vaginalis α-Actinin 2 Modulates Host Immune Responses by Inducing Tolerogenic Dendritic Cells via IL-10 Production from Regulatory T Cells
Hye-Yeon Lee, Juri Kim, Jae-Sook Ryu, Soon-Jung Park
The Korean Journal of Parasitology.2017; 55(4): 375.
CrossRef Immune Response of BALB/c Mice toward Putative Calcium Transporter Recombinant Protein of Trichomonas vaginalis
Tahali Mendoza-Oliveros, Victor Arana-Argáez, Leidi C. Alvaréz-Sánchez, Julio Lara-Riegos, María Elizbeth Alvaréz-Sánchez, Julio C. Torres-Romero
The Korean Journal of Parasitology.2019; 57(1): 33.
CrossRef Immunopathology of Recurrent Vulvovaginal Infections: New Aspects and Research Directions
Namarta Kalia, Jatinder Singh, Manpreet Kaur
Frontiers in Immunology.2019;[Epub]
CrossRef Symbiotic Association with Mycoplasma hominis Can Influence Growth Rate, ATP Production, Cytolysis and Inflammatory Response of Trichomonas vaginalis
Valentina Margarita, Paola Rappelli, Daniele Dessì, Gianfranco Pintus, Robert P. Hirt, Pier L. Fiori
Frontiers in Microbiology.2016;[Epub]
CrossRef Trichomonas vaginalis Induces Production of Proinflammatory Cytokines in Mouse Macrophages Through Activation of MAPK and NF-κB Pathways Partially Mediated by TLR2
Ling Li, Xin Li, Pengtao Gong, Xichen Zhang, Zhengtao Yang, Ju Yang, Jianhua Li
Frontiers in Microbiology.2018;[Epub]
CrossRef Modulation of dendritic cell function by Trichomonas vaginalis-derived secretory products
Min-Ji Song, Jong-Joo Lee, Young Hee Nam, Tae-Gyun Kim, Youn Wook Chung, Mikyoung Kim, Ye-Eun Choi, Myeong Heon Shin, Hyoung-Pyo Kim
Trichomoniasis
Jae-Sook Ryu
Hanyang Medical Reviews.2010; 30(3): 213.
CrossRef