Cited By
Citations to this article as recorded by

Early detection and estimation of infection burden by real-time PCR in rats experimentally infected with Clonorchis sinensis
S. M. Mazidur Rahman, Young Mee Bae, Sung-Tae Hong, Min-Ho Choi
Parasitology Research.2011; 109(2): 297.
CrossRef An EF-handed Ca2+-binding protein of Chinese liver fluke Clonorchis sinensis
Eun Joo Chung, Tae Yun Kim, Sung-Jong Hong, Tai-Soon Yong
Parasitology Research.2013; 112(12): 4121.
CrossRef A comparison of helminth infections as assessed through coprological analysis and adult worm burdens in a wild host
Rachel L. Byrne, Ursula Fogarty, Andrew Mooney, Nicola M. Marples, Celia V. Holland
International Journal for Parasitology: Parasites and Wildlife.2018; 7(3): 439.
CrossRef Oriental Cholangiohepatitis (Clonorchiasis Infestation) Caused by Clonorchis Sinensis
Sarah Klemencic, Michael Phelan, Robert Patrick, Noushin Vahdat
The Journal of Emergency Medicine.2012; 43(2): e107.
CrossRef Clonorchis sinensis and clonorchiasis, an update
Sung-Tae Hong, Yueyi Fang
Parasitology International.2012; 61(1): 17.
CrossRef Coproantigen capture ELISA for detection of Clonorchis sinensis infection in experimentally infected rats
S.M. Mazidur Rahman, Min-Ho Choi, Young Mee Bae, Sung-Tae Hong
Parasitology International.2012; 61(1): 203.
CrossRef Cohort Profile: Community-based prospective cohort from the National Cancer Center, Korea
Jin-Kyoung Oh, Min Kyung Lim, E Hwa Yun, Min-Ho Choi, Sung-Tae Hong, Soung-Hoon Chang, Sue Kyung Park, Sung-Il Cho, Dong-Hyun Kim, Keun-Young Yoo, Hai-Rim Shin
International Journal of Epidemiology.2015; : dyv302.
CrossRef Diagnosis of helminths depends on worm fecundity and the distribution of parasites within hosts
Thomas Crellen, Melissa Haswell, Paiboon Sithithaworn, Somphou Sayasone, Peter Odermatt, Poppy H. L. Lamberton, Simon E. F. Spencer, T. Déirdre Hollingsworth
Proceedings of the Royal Society B: Biological Sciences.2023;[Epub]
CrossRef Correlation between Discharged Worms and Fecal Egg Counts in Human Clonorchiasis
Jae-Hwan Kim, Min-Ho Choi, Young Mee Bae, Jin-Kyoung Oh, Min Kyung Lim, Sung-Tae Hong, Akira Ito
PLoS Neglected Tropical Diseases.2011; 5(10): e1339.
CrossRef Application of a loop-mediated isothermal amplification (LAMP) assay targeting cox1 gene for the detection of Clonorchis sinensis in human fecal samples
S. M. Mazidur Rahman, Hyun Beom Song, Yan Jin, Jin-Kyoung Oh, Min Kyung Lim, Sung-Tae Hong, Min-Ho Choi, Justin V. Remais
PLOS Neglected Tropical Diseases.2017; 11(10): e0005995.
CrossRef Obstructive Jaundice Caused by Clonorchiasis-associated Duodenal Papillitis: A Case Report
Jun Uk Lim, Kwang Ro Joo, Hyun Phil Shin, Jae Myung Cha, Joung Il Lee, Sung Jig Lim
Journal of Korean Medical Science.2011; 26(1): 135.
CrossRef
Clonorchis sinensis and Cholangiocarcinoma
Eun-Min Kim, Sung-Tae Hong
Journal of Korean Medical Science.2025;[Epub]
CrossRef Hypersensitive Reaction to Praziquantel in a Clonorchiasis Patient
Jung-Min Lee, Hyun-Sul Lim, Sung-Tae Hong
The Korean Journal of Parasitology.2011; 49(3): 273.
CrossRef
Abstract
A cohort was established for evaluation of cancer risk factors in Sancheong-gun, Gyeongsangnam-do, Korea. As one of the cohort studies, stools of 947 residents (403 males and 544 females, age range: 29-86 years) were screened for Clonorchis sinensis eggs using both Kato-Katz method and formalin-ether sedimentation technique. The overall egg positive rate of C. sinensis was 37.7% and individual EPG (eggs per gram of feces) counts ranged from 24 to 28,800. Eight egg positive residents voluntarily joined a process of collection of the passed worms after praziquantel treatment. A total of 158 worms were recovered from 5 of the 8 treated persons, ranged from 3 to 108 in each individual. The worms were 15-20 mm × 2-3 mm in size, and showed brown-pigmented, red, or white body colors. This is the first collection record of C. sinensis adult worms from humans through anthelmintic treatment and purgation. The adult worms of C. sinensis may be paralyzed by praziquantel and then discharged passively through bile flow in the bile duct and by peristaltic movement of the bowel.
Key words: Clonorchis sinensis, praziquantel, human, recovery, adult worms
Clonorchis sinensis Looss, 1907 is one of the major human trematodes in East Asia, such as China, Korea, East Russia, Taiwan, and Vietnam (
Hong, 2003;
Rim, 2005). In Korea, clonorchiasis is still prevalent and several endemic areas are scattered along major rivers, although other intestinal parasites have been dramatically controlled by the nationwide control program (
Hong et al., 2006). The 7
th national survey on prevalence of intestinal parasites in 2004 found that egg positive rate of
C. sinensis was 2.9% and about 1.3 million people are estimated to be infected in Korea (
Korea Association of Health Promotion, 2004).
Most of the infected people of clonorchiasis are asymptomatic, but they usually complain of non-specific symptoms, such as anorexia, nausea, vomiting, loose stool, and abdominal or epigastric discomfort, when they are heavily infected (
Hong, 2003). Many complications may occur in chronic clonorchiasis of heavy intensity, and the most serious one is cholangiocarcinoma. Incidence and mortality of cholangiocarcinoma correspond well with clonorchiasis in Korea (
Choi et al., 2006;
Lim et al., 2006).
Praziquantel (PZQ), a derivative of pyrazinoiso-quinoline, is the drug of choice for treatment of trematodes (
Greenberg, 2005;
Rim, 2005). The recommended regimen for clonorchiasis is 25 mg/kg, 3 times at 5-hr intervals in a day. However, the recommended dosage of PZQ is not completely effective, with the cure rate of 83-85% in clonorchiasis (
Rim et al., 1981;
Seo et al., 1983). Control of clonorchiasis by PZQ treatment was tried in the field, but the result was incomplete in spite of repeated treatments (
Hong et al., 1998).
We established a cohort study in Sancheong-gun, Gyeongsangnam-do to evaluate risk factors of cancers in Korea, and examined the prevalence of clonorchiasis as a program of the cohort study in July 2006. The study site is a known endemic area of clonorchiasis. The present study protocol was approved by the institutional review board of the National Cancer Center of Korea, and informed consent was obtained from subjected residents. A total of 947 residents (age range, 29-86 years; median age, 64 years) were subjected to the examination, including 403 males and 544 females. The subjects were examined their stools by both Kato-Katz method and formalin-ether sedimentation technique.
The egg positive rate of C. sinensis was 37.7%, and EPG (eggs per gram of feces) counts determined by Kato-Katz method ranged from 24 to 28,800 and most of infected persons had light infection burdens (EPG < 1,000). All of the infected people were treated with 3 doses of 25 mg/kg PZQ in a day.
We tried to recover adult worms of C. sinensis, which passed through the intestine after PZQ treatment in 8 volunteers (EPG > 1,000), who fully agreed to join the worm collection protocol. They were administered with 25 mg/kg PZQ, 3 times a day, and purgation was induced on the next day by drinking of a purgative drug (Colyte®-F, Taejoon Pharm Co, Seoul, Korea). During the purgation, they were encouraged to drink as much water as possible to facilitate diarrhea and to prevent dehydration. Whole fecal samples were collected until no worms were detected in stools, and the worms were recovered from diarrheic stools.
A total of 158 adult worms of
C. sinensis were recovered from 5 of the 8 volunteers (
Table 1). Worm recovery in each individual ranged from 3 to 108, and the highest number of worms (n = 108) were collected from a heavily infected person (EPG = 12,240). Although it was difficult to predict the exact worm burden in the infected person due to a small number of subjects in this study, it was expected to recover hundreds of worms from a person with EPG higher than 10,000. Failure of worm recovery in 3 volunteers may be due to evacuation of their stool before the purgation, or by late passing of the worms from the bile duct because of the ductal pathology. Of course there still remained a possibility of lost worms during washing and collection from fecal materials, although the process was carefully carried.
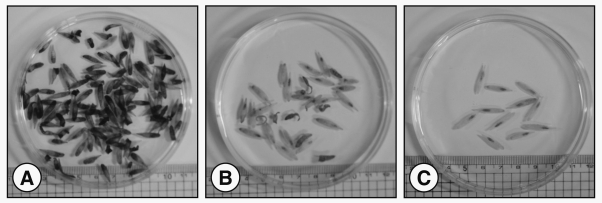
The recovered worms were fully matured and 15-20 mm × 2-3 mm in size, but, interestingly, their body color varied according to individuals; dark brown, red, and white (
Fig. 1). On the contrary, the live worms recovered directly from the liver of infected animals are usually red. We considered that the dead worms with damaged tegument by PZQ treatment lost function of their tegument, and therefore, they were stained or destained by bile, digestive fluid, or intestinal contents during the passage through the intestinal tract.
PZQ causes 2 major effects on flatworms by disruption of Ca
2+ homeostasis; a rapid, sustained muscular contraction and tegumental disruption of flatworms (
Greenberg, 2005). Major changes in PZQ-treated trematodes are vacuolization of the tegument and subtegumental parenchymal layers, and narrowing of the intestinal lumens (
Seo et al., 1985). The body size decreases by contraction at the early phase, and increases later by extensive vacuolization and relaxation. In the present study, the recovered worms showed no activity and were relaxed, indicating that they were detached from their habitat, intrahepatic bile ducts, and expelled from the infected persons by peristaltic movement of the intestinal tract.
Worm recovery by PZQ treatment and purgation from the infected persons provides crucial information for the definite diagnosis of intestinal infection by trematodes or cestodes (
Chai et al., 2000). Especially, in case of intestinal trematode infections, it is very helpful for the diagnosis, because stool examination sometimes can not provide a clue for the species of trematodes due to similar morphology of eggs between heterophyids and
C. sinensis (
Lee et al., 1984). Further human infection by unidentified parasites can be benefited by worm recovery (
Hong et al., 1988;
Lee et al., 1993). It also provides the information of the worm burden in the infected persons; however, it is not always accurate as shown by this study.
The present study first describes collection of adult worms in C. sinensis-infected persons through anthelmintic treatment and purgation. We also believe that the collected worms must be regarded as minimum confirmed numbers recovered from the subjected persons.
ACKNOWLEDGMENTS
We express our great thanks to all of voluntarily subjected residents for this worm collection trial. Also all related staffs of the Sancheong Health Center and County Hospital, Gyeongsangnam-do are appreciated for their kind help for the present worm collection.
REFERENCES
1. Chai JY, Lee GC, Park YK, Han ET, Seo M, Kim J, Guk SM, Shin EH, Choi MH, Lee SH. Persistent endemicity of
Gymnophalloides seoi infection in a southwestern coastal village of Korea with special reference to its egg laying capacity in the human host. Korean J Parasitol. 2000. 38:51-57. PMID:
10905065.



2. Choi D, Lim JH, Lee KT, Lee JK, Choi SH, Heo JS, Jang KT, Lee NY, Kim S, Hong ST. Cholangiocarcinoma and
Clonorchis sinensis infection: A case-control study in Korea. J Hepatol. 2006. 44:1066-1073. PMID:
16480786.


3. Greenberg RM. Are Ca
2+ channels targets of praziquantel action? Int J Parasitol. 2005. 35:1-9. PMID:
15619510.


4. Hong SJ, Seo BS, Lee SH, Chai JY. A human case of
Centrocestus armatus infection in Korea. Korean J Parasitol. 1988. 26:55-60.


5. Hong ST. In Miliotis MD, Bier JW eds, Clonorchis sinensis. International Handbook of Foodborne Pathogens. 2003. Basel, New York, USA: Marcel Dekker, Inc.; 581-592.

6. Hong ST, Chai JY, Choi MH, Huh S, Rim HJ, Lee SH. A successful experience of soil-transmitted helminth control in the Republic of Korea. Korean J Parasitol. 2006. 44:177-185. PMID:
16969055.



7. Hong ST, Yoon K, Lee M, Seo M, Choi MH, Sim JS, Choi BI, Yun CK, Lee SH. Control of clonorchiasis by repeated praziquantel treatment and low diagnostic efficacy of sonography. Korean J Parasitol. 1998. 36:249-254. PMID:
9868890.



8. Lee SH, Chai JY, Hong ST.
Gymnophalloides seoi n. sp. (Digenea: Gymnophallidae), the first report of human infection by a gymnophallid. J Parasitol. 1993. 79:677-680. PMID:
8410538.


9. Lee SH, Hwang SW, Chai JY, Seo BS. Comparative morphology of eggs of heterophyids and
Clonorchis sinensis causing human infections in Korea. Korean J Parasitol. 1984. 22:171-180.


10. Lim MK, Ju YH, Franceschi S, Oh JK, Kong HJ, Hwang SS, Park SK, Cho SI, Sohn WM, Kim DI, Yoo KY, Hong ST, Shin HR.
Clonorchis sinensis infection and increasing risk of cholangiocarcinoma in the Republic of Korea. Am J Trop Med Hyg. 2006. 75:93-96. PMID:
16837714.

11. Korea Association of Health Promotion. Prevalence of intestinal parasitic infections in Korea - The 7th report-. 2004. Seoul: Korea Association of Health Promotion.
12. Rim HJ. Clonorchiasis: an update. J Helminthol. 2005. 79:269-281. PMID:
16153321.


13. Rim HJ, Lyu KS, Lee JS, Joo KH. Clinical evaluation of the therapeutic efficacy of praziquantel (Embay 8440) against
Clonorchis sinensis infection in man. Ann Trop Med Parasitol. 1981. 75:27-33. PMID:
7023402.

14. Seo BS, Cha IJ, Chai JY, Hong SJ, Lee SH. Studies on intestinal trematodes in Korea XIX. Light and scanning electron microscopy of
Fibricola seoulensis collected from albino rats treated with praziquantel. Korean J Parasitol. 1985. 23:47-57.


15. Seo BS, Lee SH, Chai JY, Hong ST. Praziquantel (Distocide
®) in treatment of
Clonorchis sinensis infection. Korean J Parasitol. 1983. 21:241-245.

Notes
This study was supported by the National Cancer Center, grant number 0410130-2