INTRODUCTION
Among many tropical diseases, malaria is prevalent worldwide and remains a major health problem. According to the World Health Organization (WHO) (1994), one third of the world population are living in malaria endemic regions. Vivax malaria has been prevalent throughout the Republic of Korea (ROK) for a long time. However, as a result of a national malaria eradication program with a help from WHO, the incidence of vivax malaria rapidly decreased (National Malaria Eradication Service, 1966; Paik et al., 1988). Vivax malaria was believed to be eradicated in ROK since the late 1970s, although two sporadic cases were detected in the 1980s (Soh et al., 1985), which were relapsed after long incubation.
In 1993, a vivax malaria case was diagnosed among ROK army soldiers serving in the northern Kyonggi-do (Chai et al., 1994). Subsequently, Cho et al. (1994) reported two civilian patients infected with vivax malaria. Thereafter, a total of 2,198 patients (soldiers 1,548, civilians 650) was detected from 1994 to 1997 near the demilitarized zone (DMZ) centering around Paju-shi, Yonchon-gun, Chorwon-gun, Kimpo-shi, Kangwha-gun, Koyang-shi, and Tongduchon-shi. Hence, the possibility of re-establishment and geographical expansion of malaria is highly concerned.
The Department of Medical Zoology, National Institute of Health (Korea) is the responsible body-organ for undertaking national malaria surveillance. In order to make basic epidemiologic data on the reemerging malaria in ROK, we describe the malaria occurrence and its geographical distribution in civilian cases.
MATERIALS AND METHODS
History taking of patients
According to the "Prevention Law of Communicable Disease", in which malaria is one of reportable diseases of the second class, physicians are responsible to report its occurrence. Therefore, physicians all over the country, who diagnosed and treated malaria patients, reported the case to our Department by telephone or by document. Compliance rate was extremely high because anti-malarials, especially primaquine is very difficult to get in Korean market without the report.
All the patients in this report were diagnosed as vivax malaria by blood smear. Once reported, every case was investigated individually for the following epidemiologic items by direct or telephone interview to attending physicians: age, sex, residence, occupation, onset of symptom, date of diagnosis, past hisory of traveling abroad and within Korea, especially the experience of visiting the northern Kyonggi-do. In cases of young men, they were asked about their service areas and episodes of fever in the event they were discharged from military service. All the cases who have traveled abroad within three years were excluded from this data.
Determination of prevalent area
The prevalent area was determined by investigating the activities of patients during the malaria transmission season (May through October) and onset of symptoms. In this article, based on the above criteria, the prevalent area of malaria was determined as the northern part of Kyonggi-do and a part of Kangwon-do along the DMZ, including Paju-shi, Yonchon-gun, Chorwon-gun, Kimpo-shi, Kangwha-gun, Koyang-shi, and Tongduchon-shi.
Calculation of annual parasite index and delayed incubation period
The annual parasite index (API) was calculated as the incidence of malaria per 1,000 inhabitants. The patients of delayed incubation period (DIP) was determined as follows: patients demonstrating symptoms during the period when adult mosquitoes are inactive and after military service of soldiers in prevalent areas during the transmission period.
RESULTS
All the detected cases were vivax malaria without exception. The number of civilian cases were 3 in 1994, 19 in 1995, 71 in 1996, and 557 in 1997. Among the total civilian cases (650), 411 cases (63.2%) were civilians who had no relation with military service in the past two years, while the remaining 239 were personnel discharged from military service within two years, suggesting a correlation between malaria infection and military service.
During 1994, malaria was reported from persons of 20 years or older. In the subsequent years, the malaria incidence rate among 20-29 year-old group rapidly increased, possibly as a result of military service. The age groups 30-39, 40-49, 50-59 and over 60 years old increased similarly. Malaria rates among persons more than 20 years old was infrequent (Table 1).
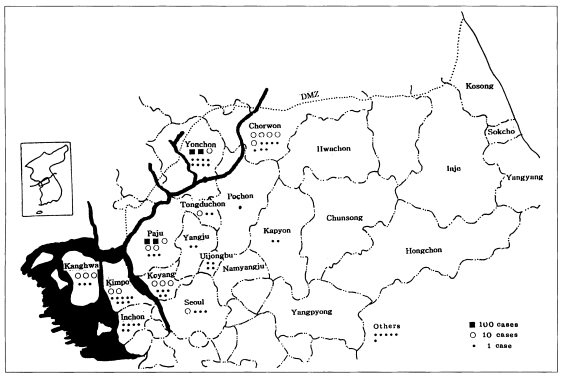
Most of the civilian patients resided in the northern part of Kyonggi-do, but the distribution of malaria for discharged soldiers demonstrated a nationwide pattern. The number of patients was the highest in Paju-shi (138) and Yonchon-gun (85), in the second place. Fewer cases were observed in Chorwon-gun (9), Kimpo-shi (17), Kanghwa-gun (17), Koyang-gun (41), Tongduchon-shi (10), and other areas (333). Civilian patients were not reported from Chorwon-gun and Kangwha-gun until 1996 (Table 2).
The relationship between civilian cases and prevalent areas were analyzed; the residents of the prevalent area occupied nearly half of the total civilian cases, ex-soldiers discharged from the prevalent areas for the second, and some had the history of traveling there. Few cases denied the relevance to the prevalent area (Table 3).
The distribution patterns were analyzed with a village as a unit. Patients from Paju-shi and Yonchon-gun were concentrated within 10 km from the DMZ in 1996, but the boundary was expanded to 20 km from DMZ in 1997. The Chorwon area reported civilian cases near the civilian control line (CCL) for the first time in 1997. Patients from Kimpo-shi and Kanghwa-gun mainly resided along the Imjingang (River) or near the river basin. Among the prevalent areas, the API of 1997 was the highest in Yonchon-gun, 1.232, and lowest in Koyang-shi, 0.056 (Table 4).
Monthly incidence of the civilian cases were shown in Table 5. The cases were diagnosed from March through December each year. But more than a hundred cases were diagnosed in July, August and September, showing an unimodal curve.
The geographical distribution pattern of 650 malaria patients was shown in Fig. 1. The malaria infection was focused to Paju-gun and Yonchon-gun, 233 and 218, respectively. Then, tens of malaria cases were infected in Kimpo-gun, Kangwha-gun, and Chorwon-gun. In addition, there were a few infections in Uijongbu-shi, Inchon-shi, Seoul-shi, Kapyong-gun, etc.
After resurgence of malaria was recognized in 1994, mean of the days from onset of symptoms to diagnosis was 23.6 days in 1995, and shortened to 13.7 in 1997. In some cases, the diagnosis was delayed up to 65-77 days after the onset of fever. However, the maximum number of days for individual patients (65-77) was not significantly different among the years 1995 through 1997.
The prolonged incubation period was calculated based on the malaria transmission season and the time of diagnosis, in 107 cases who had discharged from military service. The average of delayed incubation period was calculated as 279 ± 41 days (153 to 452 days) in those cases.
DISCUSSION
From these results, the northern Kyonggi-do and a part of Kangwon-do were confirmed to be the prevalent area of vivax malaria. The establishment of malaria along the north eastern boundary are results of ecological and socioecological conditions. Since the report of malaria patients who had never been abroad in 1993 (Chai et al., 1994), the number of patients has been annually increasing at the northern part of Kyonggi-do (Cho et al. 1994; Yim et al. 1996; Lee et al. 1997). This article describes all the civilian patients from 1994 to 1997, including the cases reported by other authors.
The proportion of cases diagnosed from active duty soldiers was 70.4%, and increased to 81.3% when discharged soldiers are included. Yim et al. (1996) indicated that there was a correlation between malaria cases and guard duty at night along the DMZ since soldiers are exposed to mosquito bites. Malaria cases during the early period of malaria reemergence were suspected to be bitten by sporozoite positive mosquitoes which flew from North Korea. In addition, we proved that the mosquitoes collected from two areas of Paju-gun, i.e., Jangpa-ri and Tongil village, had the sporozoites of Plasmodium vivax by PCR method. Based on the patients occurrence and discovery of sporozoite positive mosquitoes, the northern Kyonggi-do and a part of Kangwon-do were confirmed to be the prevalent area of vivax malaria, and malaria is established and does not require more introduction from North Korea.
Area of the greatest transmission had been damaged by floods during 1995 and 1996. The flood of July 1996 submerged farmland and houses in the northern part of Kyonggi-do and a part of Kangwon-do. About the time of environmental disasters, there was an 3.7 fold increase of malaria cases in 1996, and 7.8 fold increase in 1997. This suggests that the floods may have played a role in increased transmission of malaria by spreading mosquito population, and thereby increasing human exposure to mosquito bites.
The API for malaria ranged from 109.2 to 2.5 in 1960s when the vivax malaria had been prevalent (Kim et al. 1982; Lee et al. 1994). Currently, the API ranges from 0.056 to 1.232 in 1997, much lower than that in the early 1960s. However, because of the increasing trend and the reestablishment of malaria at Kyonggi-do, early detection and early treatment is required to interrupt the transmission cycle of malaria.
Shim et al. (1997) concluded that Anopheles mosquitoes from North Korea migrated to the south for blood-sucking to cows or pigs due to the absence of blood sources in North Korea. In addition, the environment was suitable for the mosquito survival, and the amount of insecticide used along the DMZ was less than for other areas. Anopheles sinensis is zoophilic, but readily bites human and is attracted to light, resulting in the mosquitoes' entering into houses. Due to the scarcity of large animals along the DMZ, unprotected soldiers may be the primary source of blood.
The distribution pattern by residence indicates that malaria occurs nationwidely, but these data merely reflect the return of the discharged soldiers to their residences in non-prevalent areas. However, the distribution of malaria is increasing as malaria had not been reported in Chorwon and Kangwha until 1997. The malaria distribution pattern reported by a village showed that the malaria outbreak of Paju-gun and Yonchon-gun was confirmed within 10 km of the DMZ in 1996, but the estimated prevalent area extended further south in 1997. Asymptomatic reservoirs among the civilian population might act as an infection source, increasing the distribution of malaria to areas beyond the DMZ. Hence, malaria surveillance must include an area wider than the estimated prevalent area.
By investigating the history of infected soldiers, Lim et al. (1997) recognized that 4.0% had been blood donors within a month of confirmed diagnosis, and based on delayed diagnosis, may have been positive for asexual parasites. In fact, a 67-year old woman was infected with P. vivax through blood transfusion during an operation, and the donor was proven to be a soldier during leave. Subsequently, blood examination revealed malaria parasites from the asymptomatic soldier. In Korea, the blood donation has been executed without any precaution about malaria except for conventional history report. Hence, the careful control of blood donation is required for residents of prevalent areas or persons with history of visiting prevalent areas.
In 1913, Hasegawa showed that the delayed incubation period was characteristic of Korean malaria parasite strains (Lee et al., 1994). Of 650 civilian patients, at least 239 demonstrated delayed onset of symptoms when considering the area and duration of military service. In Korea, the mosquito activity is confined to the period from May through October. Patients developing symptoms from December to May might have the delayed incubation period. Therefore, the early detection and early treatment of these carriers might prevent the additional occurrences during the onset of the malaria season.
With the reintroduction of malaria, there was insufficient knowledge and education for malaria resulting in delayed diagnosis. As health officials become more aware of malaria, the period of onset of symptoms to diagnosis decreased. However, diagnosis and radical treatment was delayed because some patients went first to the drugstore for self-treatment.
The military service began to execute the chemoprophylaxis or radical chemotherapy for soldiers conducting guard duty near the DMZ. The effect of administering chemoprevention on soldiers will be evaluated for integrating potential malaria control programs among the civilian population.