An Imported Case of Disseminated Echinococcosis in Korea
Article information
Abstract
A complicated case of echinococcosis with multiple organ involvement is reported in a 53-year-old businessman who frequently traveled overseas, including China, Russia, and Kazakhstan from 2001 to 2007. The patient was first diagnosed with a large liver cyst during a screening abdomen ultrasonography in 2011, but he did not follow up on the lesion afterwards. Six years later, dizziness, dysarthria, and cough developed, and cystic lesions were found in the brain, liver and lungs. The clinical course was complicated when the patient went through multiple surgeries and inadequate treatment with a short duration of albendazole without a definite diagnosis. The patient visited our hospital for the first time in August 2018 due to worsening symptoms; he was finally diagnosed with echinococcosis using imaging and serologic criteria. He is now on prolonged albendazole treatment (400 mg twice a day) with gradual clinical and radiological improvement. A high index of suspicion is warranted to early diagnose echinococcosis in a patient with a travel history to endemic areas of echinococcosis.
INTRODUCTION
Echinococcosis is a zoonotic parasitic infection caused by the larval stage of the tapeworm Echinococcus [1]. It is endemic in many parts of the world, including northern Africa, central Asia, Siberia, and western China. In 2015, the World Health Organization (WHO) estimated echinococcosis to be the cause of 19,300 deaths globally each year [2]. In Korea, the first case of pulmonary echinococcosis was reported in 1983 [3]. Since then, 38 echinococcosis cases have been reported, most from endemic areas. Among these cases, there were only 3 cases of disseminated echinococcosis, involving more than 2 organs [4–6]. Here, we report the case of a patient with disseminated cystic echinococcosis, who had a complicated clinical course due to a delayed diagnosis and treatment.
CASE DESCRIPTION
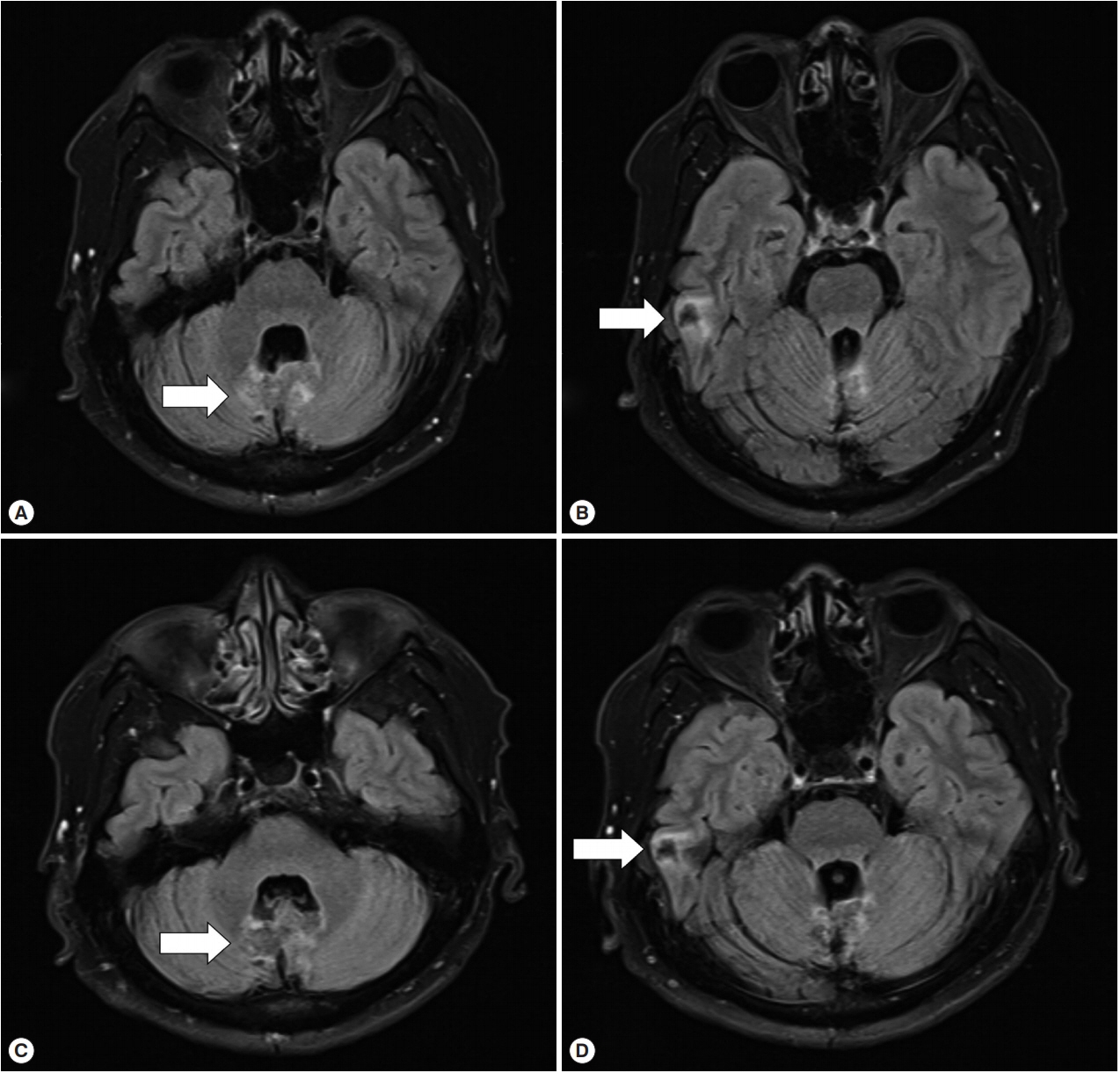
A 53-year-old businessman visited our hospital due to worsening dizziness and dysarthria starting 2 years ago. He had frequently traveled to China, Russia, and Kazakhstan between 2001 and 2007. He was previously healthy except for a history of tuberculous pleurisy 30 years ago. He was first diagnosed with a liver cyst (unknown size) by screening abdominal ultrasonography in a hospital in 2011. However, he did not follow up on the lesion. In April 2017, he visited another hospital because of non-whirling dizziness and dysarthria for several months. A 2 cm cerebellar mass and an 11.8 cm liver cyst were found in the brain magnetic resonance imaging (MRI) and abdomen computed tomography (CT), respectively (Fig. 1A, B). A stereotactic brain biopsy was attempted because a glioblastoma was suspected radiologically, but no tissue was obtained because of dense calcification. Craniotomy and mass removal were performed, and the pathologic exam revealed necrotizing granulomatous inflammation with hyalinized bodies indicating parasitic infection, although no definite parasites were found. The presumptive diagnosis was neurocysticercosis, due to the positive result from the enzyme-linked immunosorbent assay (ELISA) for cysticercosis IgG (an unknown value). The patient took albendazole, 500 mg twice a day (14 mg/kg/day), for 52 days but his dizziness did not disappear. However, he did not visit the hospital of his own will.
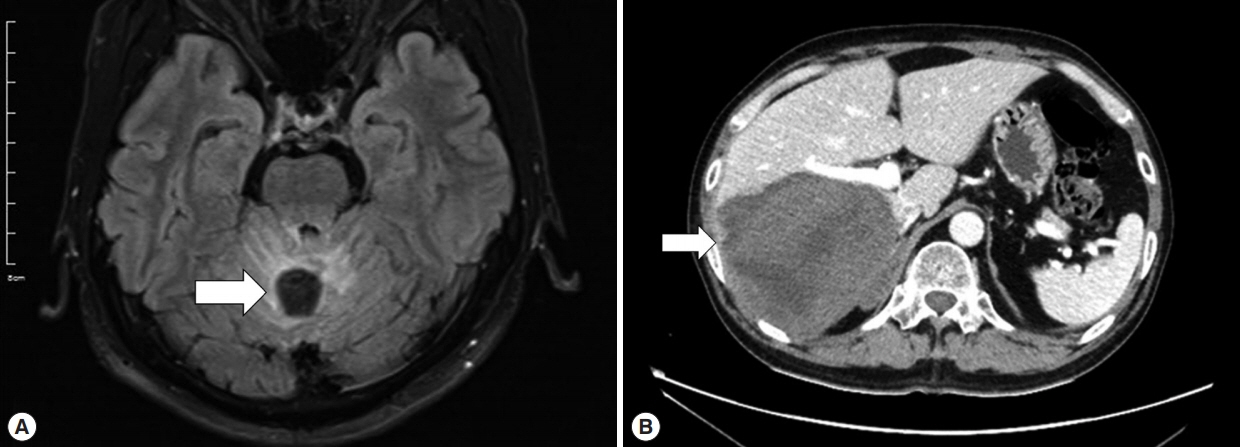
Cystic lesions in the liver and cerebellum in 2017. (A) MRI T2 sequencing showed a 2 cm peripheral enhancing mass (arrow) in the cerebellum. (B) Liver CT, with portal vein enhancement, showed an 11 cm lobulated mass (arrow) in the right posterior section of the liver.
In April 2018, the patient visited another hospital because his dry cough had progressed. CT revealed multiple cystic lesions in both lungs and a 12.4 cm liver cyst involving the right adrenal gland (Fig. 2A, B), and a follow-up brain MRI was performed that showed aggravated cerebellar lesions and a newly developed cystic lesion in the right temporal lobe (Fig. 2C, D). The patient underwent a right lower lobectomy, right hepatectomy, and right adrenalectomy because malignant disease was suspected. However, the histopathologic exams revealed chronic granulomatous inflammation with the degenerated parasitic organism (Fig. 3A–D). Praziquantel 1,200 mg 3 times a day (50 mg/kg/day) was prescribed for 14 days.
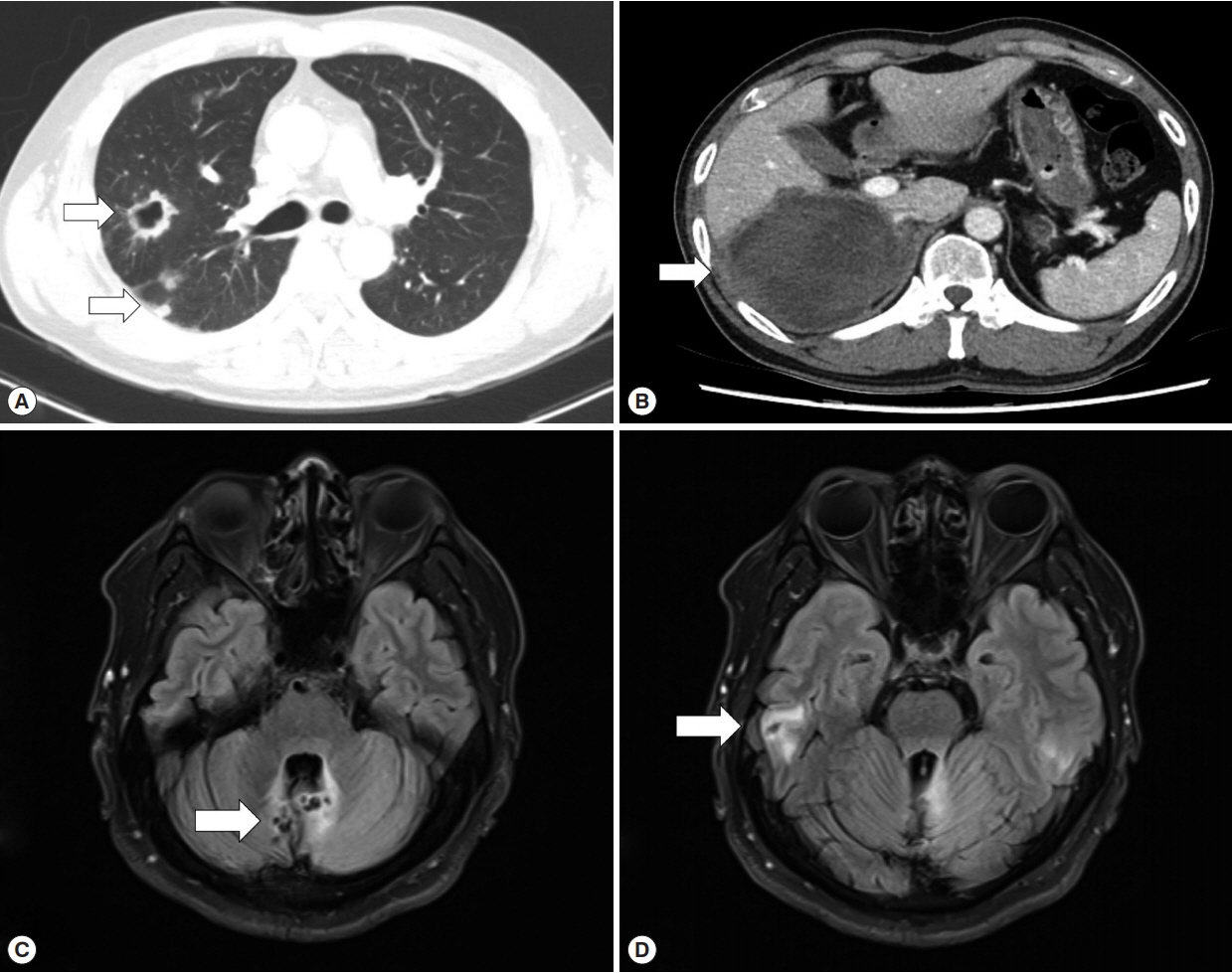
Cystic lesions in the lung, liver, and brain in April 2018. (A) Chest CT showed multiple cystic to nodular lesions (arrows). (B) Liver CT, with portal vein enhancement, showed a 12.4 cm lobulated mass (arrow). (C, D) Brain MRI T2 sequencing showed new cystic lesions in the cerebellum and right temporal lobe (arrow).
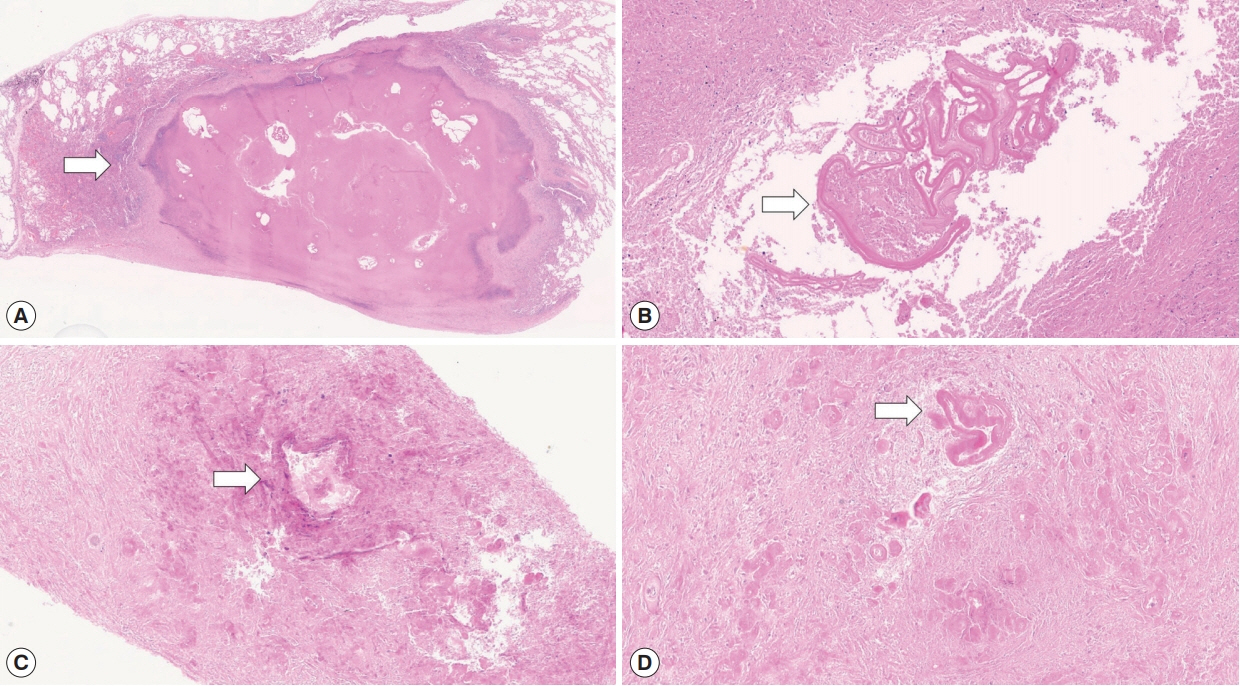
Pathologic exams of the resected lung tissue (A, B), and liver (C, D). (A) A demarcated lesion with extensive necrosis is observed (arrow). (B) High-power view reveals lamellated cyst wall with accompanied granulomatous inflammation (arrow). (C) A near-totally necrotic tissue with vague cyst-forming lesion (arrow). (D) High-power view reveals some amorphous hyalinized eosinophilic bodies (arrow).
In August 2018, the patient visited our hospital because of worsening symptoms. This was the third university-affiliated hospital he had visited during the course. At admission, his vital signs and laboratory tests were all within normal limits except for mild elevation of eosinophils (white blood cell count 9,190/μl; segment neutrophils 66.2%, lymphocytes 20.9%, eosinophils 5.8%). Although IgG for cysticercosis was positive again (titer 0.704; cut-off 0.232) by ELISA [7], the diagnosis of neurocysticercosis was doubted because the size and shape of cysts in the liver, lung and brain were not consistent with those of cysticercosis using radiological approaches. Given the past travel history to endemic areas of echinococcosis and the multiple organ involvement of cysts with varying sizes, a serum ELISA for echinococcosis IgG was performed as previously described [8], and turned out to be positive (titer 0.886; cut-off 0.270). The patient was finally diagnosed as probable cystic echinococcosis based on the diagnostic criteria [9]. Since it was technically difficult to excise all lesions from both cerebellar hemispheres and the temporal lobe, albendazole, 400 mg twice a day (10–15 mg/kg/day), was started. Worried about paradoxical worsening of neurological symptoms after the commencement of the treatment, we prescribed 4 mg of dexamethasone 4 times a day for 3 days, and then it had been tapered off over 10 days. His dizziness and dysarthria are gradually improving, and the cerebellar lesions are also radiologically improving at 2 (Fig. 4A, B) and 7 months (Fig. 4C, D) after the commencement of the therapy.
DISCUSSION
We have described a case of echinococcosis involving multiple organs that was complicated by a delayed diagnosis and treatment. Since echinococcosis is not prevalent in Korea, people are infected during travels to endemic areas and this makes an early diagnosis and proper management more challenging. The present case is the 4th disseminated case in Korea, and probably the most complicated, which underscores the importance of a high index of suspicion in a patient who has visited endemic areas of echinococcosis.
In Korea, 38 cases of echinococcosis have been reported since it was first described in 1983 [4–6,10–14]. Most cases involved the liver (22/38, 57.9%) or lung (10/38, 26.3%) only, while 3 involved multiple organs (3/38, 7.9%). Two of those three cases were cured by a resection operation [6,15]. However, one patient underwent repeated surgeries and was treated with long-term albendazole due to a delayed diagnosis because she had no history of travel to the endemic areas [5]. The present patient had another complicated case of disseminated echinococcosis. However, the patient had an extensive travel history to endemic area of echinococcosis; thus, one of the previous physicians should have considered this possibility.
If a patient with a large liver cyst had a travel history to endemic areas, echinococcosis should have been placed on the list of differentials and follow-up tests performed regularly. Also, it is important to ask the patient about close contact with a dog, which is a major route of infection by the tapeworm Echinococcus [16]. Since the cystic lesion of echinococcosis grows slowly and it may take several years before it is diagnosed [17], it is necessary to explore the exposure or travel history of the patient several years before detection of the hydatid cyst.
The next issue is to differentiate between echinococcosis and cysticercosis. Imaging procedures such as CT and MRI can easily differentiate the metacestode of Taenia solium (cysticercus) from a hydatid cyst. In neurocysticercosis, cysts of T. solium appear as small, round areas with the scolex within the cyst, and are easily distinguished from parenchyma of the brain. When cysts are degenerating, they show ill-defined margin and tend to be surrounded by edema [18]. In contrast, lesions of echinococcosis are presented as tumor-like masses with varying sizes, usually bigger than those of the cysts of T. solium, and the lesions have irregular margins, heterogeneous internal structures, and calcifications on CT [19]. In the present case, there were no cystic lesions showing the scolex on brain MRI [20], and a huge liver cyst larger than 5 cm was far more accordant with echinococcosis [9,21]. In this regard, the diagnosis should have been made more prudently.
Currently, serological diagnosis by ELISA is performed to detect infection by 4 major tissue parasites in Korea, which includes Clonorchis sinensis, Paragonimus westermani, the metacestode of Taenia solium, and sparganum. Therefore, without suspicion, the diagnosis of echinococcosis would be difficult by conventional ELISA as it does not include the detection of antibodies against the tapeworm Echinococcus. The positive result of IgG for cysticercosis in this case might be a cross-reaction with echinococcosis, and this made the diagnosis more difficult [22].
Suspecting echinococcosis prior to a surgery or a procedure is crucial because spillage of viable parasite material may cause anaphylactic reactions or secondary cystic echinococcosis [9]. During the patient’s first operation, the hydatid cyst might have spilled and led to more metastatic infections of the lungs and brain. Treatment options for cystic echinococcosis include surgery, percutaneous treatment, and drugs. Although surgery or percutaneous treatment are more preferred options, albendazole is often used as an adjunctive therapy after surgery or percutaneous treatment, or as a definitive therapy for small lesions [9,23–25]. However, there are some reports where inoperable disseminated or cerebral echinococcosis has been treated with a prolonged (at least 6 months) course of albendazole [9,26–28]. Fifty-two days of albendazole treatment after the first hospital visit might not have been sufficient for echinococcosis in the present case. Since it was impossible to excise all lesions in the present case, we decided to treat the patient with long-term albendazole, and he is now gradually improving both clinically and radiologically.
In conclusion, we presented a case of disseminated echinococcosis complicated by a delayed diagnosis and treatment. Considering a patient’s history of travels to endemic areas and having a high index of suspicion are crucial factors for an early diagnosis of echinococcosis.
ACKNOWLEDGMENT
This work was supported by Seoul National University Hospital.
Notes
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.