Demodex Blepharitis: An Analysis of Nine Patients
Article information
Abstract
Inflammatory eyelid symptoms are common in primary care and there have been several reports on Demodex blepharitis. In the present study, we evaluate the 9 patients with Demodex blepharitis, who showed inflammation of the eyelids, dry eye, and cylindrical dandruff at the base of the eyelashes. The causative species from all patients was Demodex folliculorum of either the adult or nymph stage. Two patients had recurrent chalazion and 3 patients had keratitis. Weekly lid scrubs with 50% tee tree oil were performed for 6 weeks. After treatment, the symptoms of blepharitis and keratitis had improved in all patients. This case report provides clinical reference source for the proper treatment of ocular demodicosis.
INTRODUCTION
Demodex is a genus of tiny mites living in the hair follicles or sebaceous glands of mammals including humans. The 2 Demodex species found in humans that are associated with ocular manifestations are Demodex folliculorum and D. brevis. They are more commonly known as eyelash mites, face mites or skin mites [1–3]. These species cause various ocular problems, including blepharitis, rosacea, keratitis and meibomian gland dysfunction, and inflammatory eyelid symptoms [4]. The diagnosis and treatment of Demodex blepharitis have been reported in primary care units in Korea [5–7].
A study of the clinical manifestations and immunological response to ocular demodicosis, found the condition to aggravate other inflammatory ocular disorders [5]. Recently, a strong correlation has been found between the severity of ocular discomfort from eye conditions and Demodex in eyelashes [6]. A case report has also suggested Demodex associated focal inflammatory nodules in the palpebral conjunctiva [7]. Besides Demodex, there are numerous causes of blepharitis including bacterial or fungal infections, dry eyes, and meibomian gland dysfunction. Therefore, differential diagnosis of eyelid diseases is necessary to ensure appropriate treatment [8]. Demodex is also implicated in other ocular problems such as conjunctivitis, keratitis, and even malignant tumors of the eyelid [7,9,10]. However, Demodex is accepted as a normal part of the eyelid flora and whether these tiny mites should be regarded as benign or malignant is a matter of dispute.
The treatment of ocular demodicosis may be oral or topical, but clear guidelines have not yet been established [11]. Demodex is the most common ectoparasite found on human skin and has been implicated with a variety of ocular diseases [12]. It therefore should be a principal differential in the diagnosis of inflammatory symptoms of the eyelid, conjunctiva, and even cornea. It is easily misdiagnosed due to significant overlaps with other conditions. In this case report, we discuss the clinical manifestations and proper treatment of ocular demodicosis.
CASE RECORDS
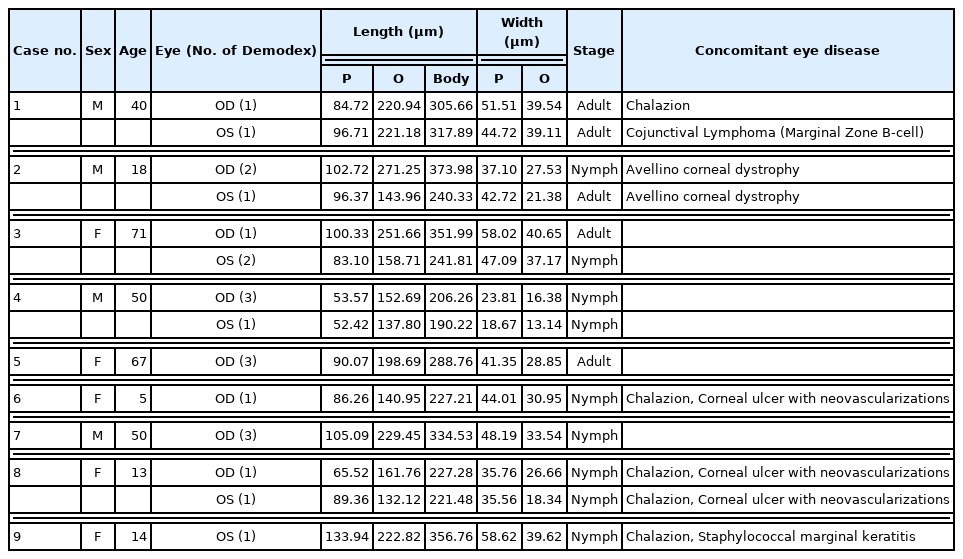
Among the patients admitted to the Department of Ophthalmology, Dankook University Hospital between January 2020 and April 2021, we analyzed 9 cases diagnosed with Demodex blepharitis. In all patients, 8 eyelashes (4 from the upper and 4 from the lower eyelid) were removed from 1 eye and examined for Demodex spp. under a light microscope (Fig. 1). We identified these mites as Demodex folliculorum of the adult or nymph stage. The length and width of the prosoma, opisthosoma, and the whole body of each specimen were easured using ImageJ (National Institute of Health, Bethesda, Maryland, USA) software (https://imagej.nih.gov/). The developmental stage of each specimen was inferred from the morphological traits observed including the length and width of the prosoma and opisthosoma (Table 1).
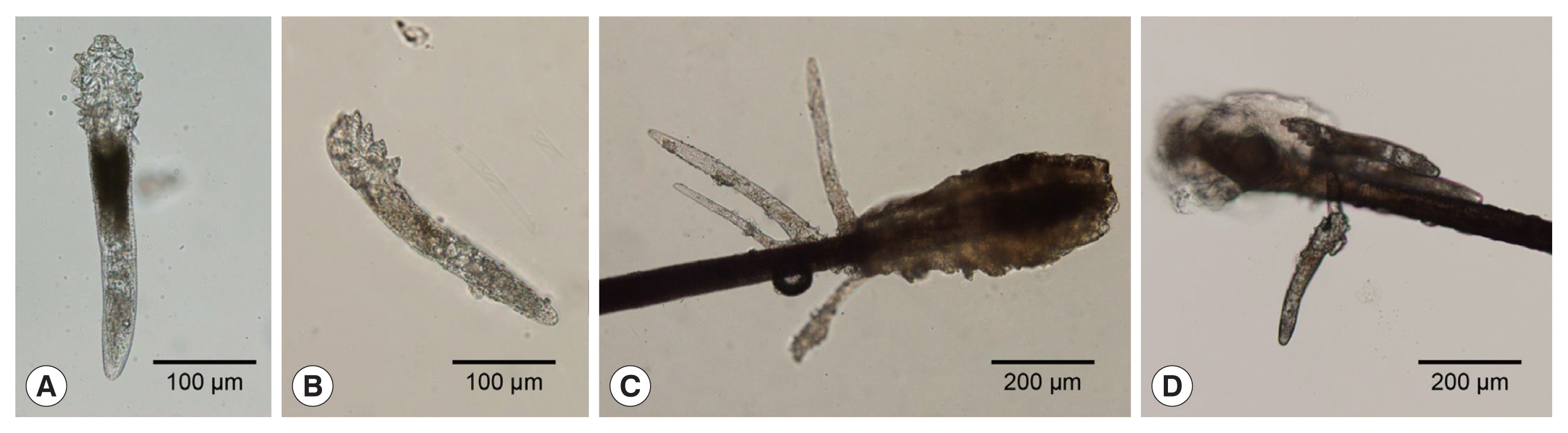
Photographs of Demodex species recovered from patients. A number of D. folliculorum was found in the patients’ eyelashes. They were mostly at nymph and adult stages, varying in length and width. (A) Ventral view of adult Demodex sp. (B) Lateral view of adult Demodex sp. (C) A cluster of Demodex sp. found at the hair bulb. (D) Demodex sp. sticking to the hair shaft.
The mean age of the patients was 36.4 years (range: 5–71 years), and 5 patients were female. Among them, 2 had diabetes and 2 suffered from hypertension. One patient had conjunctival lymphoma in the left eye, which was surgically removed and treated with radiation (case 1). None of the other patients had any history of eye trauma or surgery. The main symptoms with which patients presented were the foreign body sensation, itching, redness, and pain. On slit lamp microscopic examination, all patients showed inflammation of the eyelids, dry eyes, and cylindrical dandruff at the base of the eyelashes (Fig. 2B). In addition to blepharitis, 2 patients had recurrent chalazion and 3 had keratitis (cases 6, 8, and 9). Those with keratitis were pediatric patients aged 5, 13, and 14 years. Two of these 3 had neovascularization (Fig. 2A) and 1 had staphylococcal marginal keratitis. Weekly lid scrubs with 50% tea tree oil (TTO) were performed at the clinic to remove the Demodex mites, and daily lid scrubs with 0.4% polyhexamethylene biguanide (Ocusoft, Richmond, Texas, USA) were administered for 6 weeks. Antibiotic eye drops (levofloxacin) and steroid eye drops (fluorometholone) were prescribed for patients with keratitis or staphylococcal marginal keratitis. Blepharitis symptoms improved in all patients after 6 weeks of treatment. The symptoms of keratitis had also improved and corneal neovascularization decreased (Fig. 2C).

Photographs of Demodex blepharitis and corneal ulcer in 5-year-old female patient. (A) Corneal ulcer with eyelid inflammation and corneal neovascularization at the time of initial visit. (B) Severe inflammation with telangiectasis on the eyelid. (C) Improved after 3 weeks of treatment with lid scrubs with 50% tea tree oil and antibiotic eye drops.
DISCUSSION
As shown in Table 1, all of the Demodex found in our series were D. folliculorum of nymph or adult stages of D. folliculorum. Although D. brevis is also a primary cause of demodicosis, it was not found in these patients. Ocular complications are more common as the density of the mites increases over time. However, there was no correlation between symptoms and mite density, as high tick density was also observed in asymptomatic blepharitis [13]. Our cases included children and teenagers (Table 1). Interestingly, significant Demodex-related symptoms such as trichiasis and scaly discharge from the eyelashes, were seen in these patients, even in healthy children [14].
Demodex can causes various ocular problems besides blepharitis, and associated ocular symptoms might be often confused with other pathologies. Several cylindrical dandruff and scales were observed in eyelashes of the patients enrolled in this study, which are characteristic features of Demodex blepharitis [15]. In our cases, 2 patients had recurrent chalazion and 3 patients had keratitis; one of them was staphylococcal marginal keratitis, and 2 were accompanied by neovascularization. As a common eye problem in patients of all ages, chalazions are highly correlated with demodicosis. Furthermore, ocular demodicosis is a risk factor for chalazions and may be involved in their pathogenesis, although whether demodicosis is a direct cause of chalazions is not yet established yet [16–18]. Differential diagnosis of inflammatory conditions, especially in the anterior compartment of the eye, is essential [8]. When diagnosing infectious agents such as Herpes virus, Demodex leads to misdiagnosis as viral keratitis or allergic conjunctivitis [19]. In cases of recurrent viral keratitis, comorbid ocular demodicosis should be considered to prevent the viral infection from entering the cornea [20]. Demodex infestation is often overlooked in clinical settings of ocular surface inflammatory diseases and may be a cause of antibacterial and antiviral treatment failure. Although its pathogenesis has been debated for a long time, increasing evidence suggests that Demodex infestation is a potential cause of ocular surface inflammation in blepharitis, blepharoconjunctivitis, chalazion, corneal neovascularization, and sight-threatening keratitis [21].
Topical TTO administration is the most common treatment for blepharitis [5,21]. In our series, all Demodex-associated symptoms were improved with topical administration of 50% TTO. However, its effectiveness has not been well-evaluated in the literature and the most effective concentration for good clinical outcomes is uncertain since higher concentrations can cause irritation [22,23]. Therefore, further data on TTO, including the optimum concentration and administration period are needed. As an alternative to TTO, the topical administration of ivermectin, either alone or in combination with metronidazole, is also effective, having both antiparasitic and anti-inflammatory effects [24,25].
As this study is a case report and does not include statistical analysis of data from a large sample, it is limited in its ability to explain how the type, number, and stage of Demodex relate to the clinical picture of blepharitis how Demodex affects blepharitis and other comorbidities. Inflammatory eyelid symptoms related to Demodex are common, but are not properly diagnosed despite many cases of demodicosis in Korea. Our present study provides a clinical reference for the proper treatment and management of ocular demodicosis.
Notes
The authors declare no competing interests.