Abstract
Inflammatory eyelid symptoms are common in primary care and there have been several reports on Demodex blepharitis. In the present study, we evaluate the 9 patients with Demodex blepharitis, who showed inflammation of the eyelids, dry eye, and cylindrical dandruff at the base of the eyelashes. The causative species from all patients was Demodex folliculorum of either the adult or nymph stage. Two patients had recurrent chalazion and 3 patients had keratitis. Weekly lid scrubs with 50% tee tree oil were performed for 6 weeks. After treatment, the symptoms of blepharitis and keratitis had improved in all patients. This case report provides clinical reference source for the proper treatment of ocular demodicosis.
-
Key words: Demodex folliculorum, Demodex brevis, demodicosis, blepharitis, keratitis, tee tree oil
INTRODUCTION
Demodex is a genus of tiny mites living in the hair follicles or sebaceous glands of mammals including humans. The 2
Demodex species found in humans that are associated with ocular manifestations are
Demodex folliculorum and
D. brevis. They are more commonly known as eyelash mites, face mites or skin mites [
1–
3]. These species cause various ocular problems, including blepharitis, rosacea, keratitis and meibomian gland dysfunction, and inflammatory eyelid symptoms [
4]. The diagnosis and treatment of
Demodex blepharitis have been reported in primary care units in Korea [
5–
7].
A study of the clinical manifestations and immunological response to ocular demodicosis, found the condition to aggravate other inflammatory ocular disorders [
5]. Recently, a strong correlation has been found between the severity of ocular discomfort from eye conditions and
Demodex in eyelashes [
6]. A case report has also suggested
Demodex associated focal inflammatory nodules in the palpebral conjunctiva [
7]. Besides
Demodex, there are numerous causes of blepharitis including bacterial or fungal infections, dry eyes, and meibomian gland dysfunction. Therefore, differential diagnosis of eyelid diseases is necessary to ensure appropriate treatment [
8].
Demodex is also implicated in other ocular problems such as conjunctivitis, keratitis, and even malignant tumors of the eyelid [
7,
9,
10]. However,
Demodex is accepted as a normal part of the eyelid flora and whether these tiny mites should be regarded as benign or malignant is a matter of dispute.
The treatment of ocular demodicosis may be oral or topical, but clear guidelines have not yet been established [
11].
Demodex is the most common ectoparasite found on human skin and has been implicated with a variety of ocular diseases [
12]. It therefore should be a principal differential in the diagnosis of inflammatory symptoms of the eyelid, conjunctiva, and even cornea. It is easily misdiagnosed due to significant overlaps with other conditions. In this case report, we discuss the clinical manifestations and proper treatment of ocular demodicosis.
CASE RECORDS
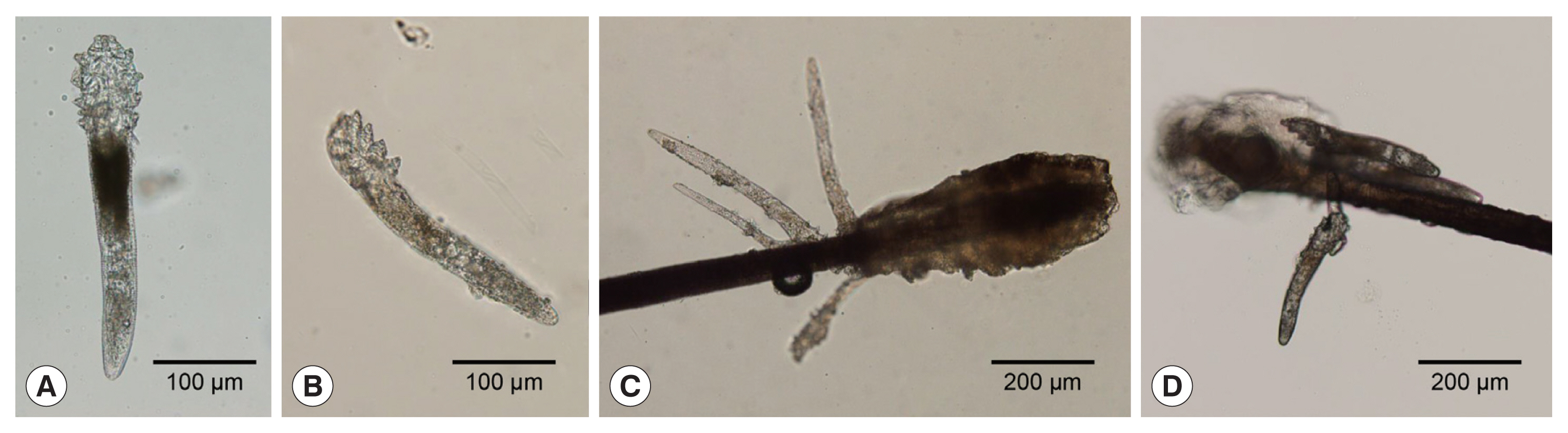
Among the patients admitted to the Department of Ophthalmology, Dankook University Hospital between January 2020 and April 2021, we analyzed 9 cases diagnosed with
Demodex blepharitis. In all patients, 8 eyelashes (4 from the upper and 4 from the lower eyelid) were removed from 1 eye and examined for
Demodex spp. under a light microscope (
Fig. 1). We identified these mites as
Demodex folliculorum of the adult or nymph stage. The length and width of the prosoma, opisthosoma, and the whole body of each specimen were easured using ImageJ (National Institute of Health, Bethesda, Maryland, USA) software (
https://imagej.nih.gov/). The developmental stage of each specimen was inferred from the morphological traits observed including the length and width of the prosoma and opisthosoma (
Table 1).
The mean age of the patients was 36.4 years (range: 5–71 years), and 5 patients were female. Among them, 2 had diabetes and 2 suffered from hypertension. One patient had conjunctival lymphoma in the left eye, which was surgically removed and treated with radiation (case 1). None of the other patients had any history of eye trauma or surgery. The main symptoms with which patients presented were the foreign body sensation, itching, redness, and pain. On slit lamp microscopic examination, all patients showed inflammation of the eyelids, dry eyes, and cylindrical dandruff at the base of the eyelashes (
Fig. 2B). In addition to blepharitis, 2 patients had recurrent chalazion and 3 had keratitis (cases 6, 8, and 9). Those with keratitis were pediatric patients aged 5, 13, and 14 years. Two of these 3 had neovascularization (
Fig. 2A) and 1 had staphylococcal marginal keratitis. Weekly lid scrubs with 50% tea tree oil (TTO) were performed at the clinic to remove the
Demodex mites, and daily lid scrubs with 0.4% polyhexamethylene biguanide (Ocusoft, Richmond, Texas, USA) were administered for 6 weeks. Antibiotic eye drops (levofloxacin) and steroid eye drops (fluorometholone) were prescribed for patients with keratitis or staphylococcal marginal keratitis. Blepharitis symptoms improved in all patients after 6 weeks of treatment. The symptoms of keratitis had also improved and corneal neovascularization decreased (
Fig. 2C).
DISCUSSION
As shown in
Table 1, all of the
Demodex found in our series were
D. folliculorum of nymph or adult stages of
D. folliculorum. Although
D. brevis is also a primary cause of demodicosis, it was not found in these patients. Ocular complications are more common as the density of the mites increases over time. However, there was no correlation between symptoms and mite density, as high tick density was also observed in asymptomatic blepharitis [
13]. Our cases included children and teenagers (
Table 1). Interestingly, significant
Demodex-related symptoms such as trichiasis and scaly discharge from the eyelashes, were seen in these patients, even in healthy children [
14].
Demodex can causes various ocular problems besides blepharitis, and associated ocular symptoms might be often confused with other pathologies. Several cylindrical dandruff and scales were observed in eyelashes of the patients enrolled in this study, which are characteristic features of
Demodex blepharitis [
15]. In our cases, 2 patients had recurrent chalazion and 3 patients had keratitis; one of them was staphylococcal marginal keratitis, and 2 were accompanied by neovascularization. As a common eye problem in patients of all ages, chalazions are highly correlated with demodicosis. Furthermore, ocular demodicosis is a risk factor for chalazions and may be involved in their pathogenesis, although whether demodicosis is a direct cause of chalazions is not yet established yet [
16–
18]. Differential diagnosis of inflammatory conditions, especially in the anterior compartment of the eye, is essential [
8]. When diagnosing infectious agents such as
Herpes virus,
Demodex leads to misdiagnosis as viral keratitis or allergic conjunctivitis [
19]. In cases of recurrent viral keratitis, comorbid ocular demodicosis should be considered to prevent the viral infection from entering the cornea [
20].
Demodex infestation is often overlooked in clinical settings of ocular surface inflammatory diseases and may be a cause of antibacterial and antiviral treatment failure. Although its pathogenesis has been debated for a long time, increasing evidence suggests that
Demodex infestation is a potential cause of ocular surface inflammation in blepharitis, blepharoconjunctivitis, chalazion, corneal neovascularization, and sight-threatening keratitis [
21].
Topical TTO administration is the most common treatment for blepharitis [
5,
21]. In our series, all
Demodex-associated symptoms were improved with topical administration of 50% TTO. However, its effectiveness has not been well-evaluated in the literature and the most effective concentration for good clinical outcomes is uncertain since higher concentrations can cause irritation [
22,
23]. Therefore, further data on TTO, including the optimum concentration and administration period are needed. As an alternative to TTO, the topical administration of ivermectin, either alone or in combination with metronidazole, is also effective, having both antiparasitic and anti-inflammatory effects [
24,
25].
As this study is a case report and does not include statistical analysis of data from a large sample, it is limited in its ability to explain how the type, number, and stage of Demodex relate to the clinical picture of blepharitis how Demodex affects blepharitis and other comorbidities. Inflammatory eyelid symptoms related to Demodex are common, but are not properly diagnosed despite many cases of demodicosis in Korea. Our present study provides a clinical reference for the proper treatment and management of ocular demodicosis.
Notes
-
The authors declare no competing interests.
Fig. 1Photographs of Demodex species recovered from patients. A number of D. folliculorum was found in the patients’ eyelashes. They were mostly at nymph and adult stages, varying in length and width. (A) Ventral view of adult Demodex sp. (B) Lateral view of adult Demodex sp. (C) A cluster of Demodex sp. found at the hair bulb. (D) Demodex sp. sticking to the hair shaft.

Fig. 2Photographs of Demodex blepharitis and corneal ulcer in 5-year-old female patient. (A) Corneal ulcer with eyelid inflammation and corneal neovascularization at the time of initial visit. (B) Severe inflammation with telangiectasis on the eyelid. (C) Improved after 3 weeks of treatment with lid scrubs with 50% tea tree oil and antibiotic eye drops.

Table 1Numerical measurements of Demodex folliculorum collected
Table 1
|
Case no. |
Sex |
Age |
Eye (No. of Demodex) |
Length (μm) |
Width (μm) |
Stage |
Concomitant eye disease |
|
|
|
P |
O |
Body |
P |
O |
|
1 |
M |
40 |
OD (1) |
84.72 |
220.94 |
305.66 |
51.51 |
39.54 |
Adult |
Chalazion |
|
|
|
OS (1) |
96.71 |
221.18 |
317.89 |
44.72 |
39.11 |
Adult |
Cojunctival Lymphoma (Marginal Zone B-cell) |
|
|
2 |
M |
18 |
OD (2) |
102.72 |
271.25 |
373.98 |
37.10 |
27.53 |
Nymph |
Avellino corneal dystrophy |
|
|
|
OS (1) |
96.37 |
143.96 |
240.33 |
42.72 |
21.38 |
Adult |
Avellino corneal dystrophy |
|
|
3 |
F |
71 |
OD (1) |
100.33 |
251.66 |
351.99 |
58.02 |
40.65 |
Adult |
|
|
|
|
OS (2) |
83.10 |
158.71 |
241.81 |
47.09 |
37.17 |
Nymph |
|
|
|
4 |
M |
50 |
OD (3) |
53.57 |
152.69 |
206.26 |
23.81 |
16.38 |
Nymph |
|
|
|
|
OS (1) |
52.42 |
137.80 |
190.22 |
18.67 |
13.14 |
Nymph |
|
|
|
5 |
F |
67 |
OD (3) |
90.07 |
198.69 |
288.76 |
41.35 |
28.85 |
Adult |
|
|
|
6 |
F |
5 |
OD (1) |
86.26 |
140.95 |
227.21 |
44.01 |
30.95 |
Nymph |
Chalazion, Corneal ulcer with neovascularizations |
|
|
7 |
M |
50 |
OD (3) |
105.09 |
229.45 |
334.53 |
48.19 |
33.54 |
Nymph |
|
|
|
8 |
F |
13 |
OD (1) |
65.52 |
161.76 |
227.28 |
35.76 |
26.66 |
Nymph |
Chalazion, Corneal ulcer with neovascularizations |
|
|
|
OS (1) |
89.36 |
132.12 |
221.48 |
35.56 |
18.34 |
Nymph |
Chalazion, Corneal ulcer with neovascularizations |
|
|
9 |
F |
14 |
OS (1) |
133.94 |
222.82 |
356.76 |
58.62 |
39.62 |
Nymph |
Chalazion, Staphylococcal marginal keratitis |
References
- 1. Kheirkhah A, Casas V, Li W, Raju VK, Tseng SCG. Corneal manifestations of ocular Demodex infestation. Am J Ophthalmol 2007;143:743-749. https://doi.org/10.1016/j.ajo.2007.01.054
- 2. Bhandari V, Reddy JK. Blepharitis: always remember demodex. Middle East Afr J Ophthalmol 2014;21:317-320. https://doi.org/10.4103/0974-9233.142268
- 3. English FP, Nutting WB. Demodicosis of ophthalmic concern. Am J Ophthalmol 1981;91:362-372. https://doi.org/10.1016/0002-9394(81)90291-9
- 4. Stephanie RF, Jennifer SH, Jaymeni P, Dominick LO. Demodex blepharitis: clinical perspectives. Clin Optom 2018;10:57-63. https://doi.org/10.2147/OPTO.S142708
- 5. Kim JH, Chun YS, Kim JC. Clinical and immunological responses in ocular demodicosis. J Korean Med Sci 2011;26:1231-1237. https://doi.org/10.3346/jkms.2011.26.9.1231
- 6. Lee SH, Chun YS, Kim JH, Kim ES, Kim JC. The relationship between demodex and ocular discomfort. Invest Ophthalmol Vis Sci 2010;51:2906-2911. https://doi.org/10.1167/iovs.09-4850
- 7. Li Y, Kim GE, Yoon KC, Choi W. First report of palpebral conjunctival inflammatory nodule associated with Demodex species. Ind J Ophthalmol 2018;66:1365-1367. https://doi.org/10.4103/ijo.IJO_375_18
- 8. Carlisle RT, Digiovanni J. Differential diagnosis of the swollen red eyelid. Am Fam Physician 2015;92:106-112.
- 9. Luo X, Li J, Chen C, Tseng S, Liang L. Ocular demodicosis as a potential cause of ocular surface inflammation. Cornea 2017;36:suppl. 9-14. https://doi.org/10.1097/ICO.0000000000001361
- 10. Yam JC, Tang BS, Chan TM, Cheng AC. Ocular demodicidosis as a risk factor of adult recurrent chalazion. Eur J Ophthalmol 2014;24:159-163. https://doi.org/10.5301/ejo.5000341
- 11. Jacob S, VanDaele MA, Brown JN. Treatment of Demodex-associated inflammatory skin conditions: A systematic review. Dermatol Ther 2019;32:e13103. https://doi.org/10.1111/dth.13103
- 12. Liu J, Sheha H, Tseng SC. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol 2010;10:505-510. https://doi.org/10.1097/ACI.0b013e32833df9f4
- 13. Nicholls SG, Oakley CL, Tan A, Vote BJ. Demodex species in human ocular disease: new clinicopathological aspects. Int Ophthalmol 2017;37:303-312. https://doi.org/10.1007/s10792-016-0249-9
- 14. Zhang N, Liu Y, Wen K, Jin L, Chen C, Chen Q, Zeng Y, Liang L. Prevalence of ocular Demodex infestation in children: An epidemiological survey in South China. Eye Contact Lens 2021;47:60-64. https://doi.org/10.1097/ICL.0000000000000705
- 15. Gao YY, Di Pascuale MA, Li W, Liu DTS, Baradaran0Rafii A, Elizondo A, Kawakita T, Raju VK, Tseng SCG. High prevalence of Demodex in eyelashes with cylindrical dandruff. Inv Ophthalmol Vis Sci 2005;46:3089-3094. https://doi.org/10.1167/iovs.05-0275
- 16. Liang L, Ding X, Tseng SC. High prevalence of Demodex brevis infestation in chalazia. Am J Ophthalmol 2014;157:342-348. https://doi.org/10.1016/j.ajo.2013.09.031
- 17. Schear MJ, Milman T, Steiner T, Shih C, Udell IJ, Steiner A. The association of Demodex with chalazia: a histopathologic study of the eyelid. Ophthalmic Plast Recon Surg 2016;32:275-278. https://doi.org/10.1097/IOP.0000000000000500
- 18. Patel NV, Mathur U, Gandhi A, Singh M. Demodex blepharokeratoconjunctivitis affecting young patients: A case series. Ind J Ophthalmol 2020;68:745-749. https://doi.org/10.4103/ijo.IJO_1402_19
- 19. Hung KH, Lan YH, Lin JY, Kang EY, Tan HY, Chen HC, Hsiao CH, Yeh LK. Potential role and significance of ocular demodicosis in patients with concomitant refractory herpetic Keratitis. Clin Ophthalmol 2020;14:4469-4482. https://doi.org/10.2147/OPTH.S282059
- 20. Koo H, Kim TH, Kim KW, Wee SW, Chun YS, Kim JC. Ocular surface discomfort and Demodex: effect of tea tree oil eyelid scrub in Demodex blepharitis. J Kor Med Sci 2012;27:1574-1579. https://doi.org/10.3346/jkms.2012.27.12.1574
- 21. Ziaja-Sołtys M, Kołodziejczyk M, Rymgayłło-Jankowska B, Wróbel-Dudzińska D, Suchodoła-Ratajewicz E, Szlonzak D, Żarnowski T, Bogucka-Kocka A. Massive demodicosis of the eyes in a patient with Sjogren syndrome: a case report. Acta Parasitol 2021;66:677-681. https://doi.org/10.1007/s11686-020-00297-w
- 22. Gao YY, Di Pascuale MA, Elizondo A, Tseng SC. Clinical treatment of ocular demodicosis by lid scrub with tea tree oil. Cornea 2007;26:136-143. https://doi.org/10.1097/01.ico.0000244870.62384.79
- 23. Savla K, Le JT, Pucker AD. Tea tree oil for Demodex blepharitis. Cochrane Database Syst Rev; 2020. 6:CD013333 https://doi.org/10.1002/14651858.CD013333.pub2
- 24. Choi Y, Eom YS, Yoon EG, Song JS, Kim IH, Kim HM. Efficacy of topical ivermectin 1% in the treatment of Demodex blepharitis. Cornea 2022;41:427-434. https://doi.org/10.1097/ICO.0000000000002802
- 25. Ávila MY, Martínez-Pulgarín DF, Rizo Madrid C. Topical ivermectin-metronidazole gel therapy in the treatment of blepharitis caused by Demodex spp.: a randomized clinical trial. Cont Lens Anterior Eye 2021;44:101326. https://doi.org/10.1016/j.clae.2020.04.011
Citations
Citations to this article as recorded by

- Natural Products as Mite Control Agents in Animals: A Review
Fei Liao, Changquan Han, Qingsheng Deng, Ziyao Zhou, Taotao Bao, Menghuai Zhong, Guangyao Tao, Renjun Li, Bo Han, Yanlong Qiao, Yanchun Hu
Molecules.2023; 28(19): 6818. CrossRef