Sparganosis in the Indian Sub-continent and the Middle East
Article information
Abstract
Sparganosis is one of the common zoonotic diseases caused by infection with the larval plerocercoids (spargana) of the cestode genus Spirometra. While this parasite distributes globally in canine and feline hosts, human infection is predominantly reported in East Asia, especially China, Korea, Japan, and Thailand. Maybe related to the behavior and food culture, this zoonotic disease is rather rare in South Asia to the Middle East. In these areas, sporadic case reports have been appeared mostly in the local medical journals. To draw a solid picture of sparganosis in these non-endemic areas of Asia, we made an extensive literature survey to gather sparganosis cases in the Indian subcontinent and the Middle East.
Introduction
Sparganosis is one of the well-known zoonotic diseases caused by infection with the larval plerocercoids (sparganum; pl.=spargana) of cestode of genus Spirometra, which is a middle-sized tapeworm parasitizing in the small intestine of canine, feline, and other mammalian hosts. This parasite requires 2 intermediate hosts; coracidia hatched from eggs in freshwater are ingested by cyclops (the first intermediate hosts), and develop into procercoids. When procercoids in cyclops are ingested by amphibians (the second intermediate hosts), they grow into plerocercoids (=spargana). Along with the food-chain, reptiles, birds, and mammals including humans can act as the paratenic hosts [1–4]. While this parasite distributes globally in canine and feline hosts, human infection is predominantly reported in East and Southeast Asia, especially China [1], Korea [2], Japan [3], and Thailand [4,5]. In those highly endemic areas, human infection occurs via 3 ways; 1) as a water-borne disease by ingestion of cyclops contaminated with procercoids, 2) as a food-borne disease by ingestion of uncooked/undercooked meat harboring plerocercoids of second intermediate or paratenic hosts, and 3) direct penetration from contaminated meat used as poultice. Once Spirometra larvae are ingested by humans, they preferentially migrate into soft subcutaneous tissues to form slowly moving nodular lesions. Although the frequency is far lower than subcutaneous migration, occasionally the larvae migrate into the vital organs such as brain, spinal cord or eyes to cause deleterious results [1–4].
In contrast to the high incidence in East and Southeast Asia, this zoonotic disease is rather rare in South Asia to Middle East, maybe related to the behavior and food culture. In those areas, only few sporadic case reports have been appeared mostly in the local medical journals. To draw a solid picture of sparganosis in these non/low-endemic areas in Asia, we made an extensive literature survey to gather sparganosis cases in the Indian subcontinent and Middle East.
Literature survey
We used terms “sparganosis”, “Spirometra” and the country names like “India”, “Iraq”, and etc. for search. As the first step, we searched published works, mostly case reports, of sparganosis from PubMed (https://www.ncbi.nlm.nih.gov/pubmed/) in conjunction with Medical Subject Headings (MeSH) in the National Library of Medicine (https://www.nlm.nih.gov/mesh/). We also searched the related papers using Google Scholar (https://scholar.google.co.jp/). Then, as the secondary search, we carefully and thoroughly checked the references/citations in each paper.
Indian subcontinent
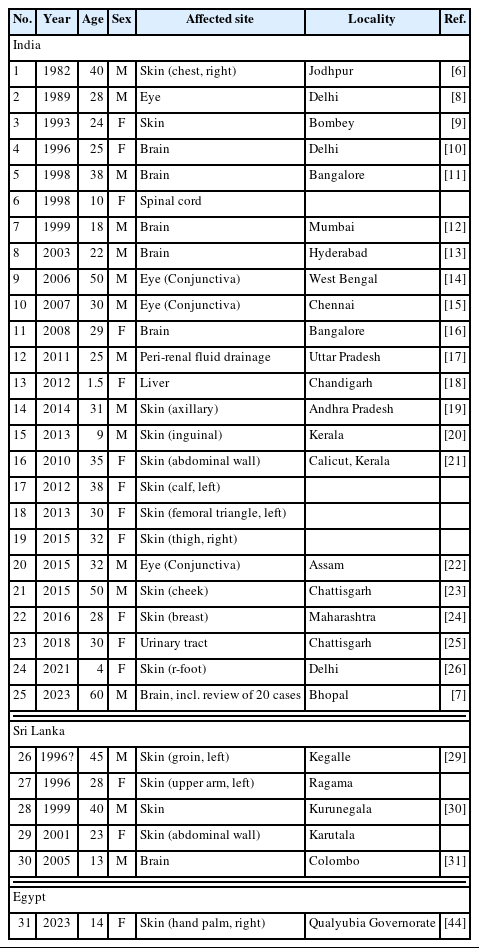
In India, the first case of human sparganosis was recorded by Datta et al. in Jodhpur in 1982 [6]. Since then, human sparganosis cases have been reported sporadically from various places of India, 20 cases of which were recently reviewed by Kaur and Shukla [7] in their case report of cerebral sparganosis. After extensive literature survey, we have found some additional cases which are not included in the list by Kaur and Shukla [7]. In total, we could gather 25 cases of human sparganosis in India and the results are summarized in Table 1 [6–26]. Their mean age was 29.3 years-old ranging from 4 to 60 years-old. No obvious gender difference was observed with the M:F ratio of 13:12. Their geographical distribution together with 5 cases in Sri Lanka (details are given below) is shown in Fig. 1. In addition to those indigenous cases listed in Table 1, there is a case report of cerebral sparganosis in an American salesman who frequently visit India on his business [27]. Conversely, a case of cerebral sparganosis in an Indian man living several years in USA was reported [28].
In Sri Lanka, Wijesundera et al. [29] first reported 2 cases of cutaneous sparganosis presented as non-tender subcutaneous lumps; one case is a 45 years-old male with left-groin lesion, and the other is a 28 years old female with left-upper arm lesion. Subsequently, Dissanike et al. [30] added 2 more cases of cutaneous sparganosis in which a plerocercoid larva (sparganum), probably of Spirometra sp., was successfully removed from the anterior abdominal wall of 2 patients (a 40-year-old man and a 23-year-old woman) in Colombo. In addition, Alibhoy et al. [31] reported a case of cerebral sparganosis in a 5-year-old boy in Sri Lanka.
A couple of review articles on parasitic zoonoses in Nepal mentioned about the incidence of potential sparganosis in Nepal without referring to actual cases [32,33]. A case of breast sparganosis in a 57-year-old Nepalese woman living in UK was reported [34]. She was born in Nepal and had moved to UK 12 years previously, but she visited Nepal 1 year before the onset of the disease. Although Sah et al. [35] reported 4 asymptomatic ocular helminthiasis and 3 of them were possibly be an infection with sparganum of Spirometra species, the size of the worms in the eyes appeared to be too small as a sparganum.
Situation of sparganosis in Bangladesh is similar to that in Nepal. Although Spirometra sp. was found in wild animals [36], actual indigenous human cases have not yet been reported. A case of cerebral sparganosis in a Bangladesh man was reported from Switzerland [37].
Middle East
Situation of human sparganosis in the Middle East is similar to that observed in Nepal and Bangladesh. Thus, Spirometra sp. tapeworms have been found in mammalian final hosts [38–42] and/or amphibian/reptile intermediate hosts [43] in this area. However, until very recently, human sparganosis cases have not been reported from Middle East. While we are preparing this manuscript, a case of hand palm sparganosis in a 14-year-old girl was reported from Egypt with morphological and genetic identification of 2 spargana as Spirometra erinaceieuropaei [44].
Overall view
After an extemsive literature review, we could find 25 cases in India, 5 cases in Sri Lanka, and 1 case in Egypt. The affected sites of all the patients are summarized in Fig. 2; among 31 sparganosis cases in the Indian subcontinent and Middle East, 16 cases are cutaneous sparganosis followed by 8 cases of CNS sparganosis (incl. 1 case of spinal lesion) and 4 cases of ocular sparganosis. In one case each, a worm (sparganum) was found in perinephritic abscess, the urinary tract and the liver.
Discussion
The genus Spirometra consisting of several species is a medium sized tapeworm parasitizing the intestine of carnivorous mammalian hosts. This tapeworm is zoonotic and when humans ingest their larval stage in the intermediate or paratenic hosts, the larvae migrate into various organs/tissues to cause acute to chronic inflammatory changes. This tapeworm is cosmopolitan and distribute worldwide. High endemicity of this disease in humans in East and Southeast Asia is related to the traditional eating habits where people consume uncooked/undercooked meats of intermediate/paratenic hosts for Spirometra, e.g., amphibians, reptiles or chickens. Thus, in those endemic areas, sparganosis is considered principally a food-borne parasitic zoonosis [2–5]. In addition, in some areas, frog meat has been used as a poultice for eye diseases in the traditional medicine [2–4]. In contrast, in this study, the most likely source of infection with sparganum in the Indian subcontinent and the Middle East is assumed to be ingestion of the infected first intermediate host, cyclops in water, and thus the disease is considered a water-borne disease [7,15,44].
In terms of the causative Spirometra species, most of the case reports listed here mentioned it at the genus level and not intended to identify the species. Exception is the one recent case report from Egypt, in that the parasite retrieved from the patient was identified as S. erinaceieuropaei by the molecular method. Although Datta et al. [6] identified the worm as S. mansoni, morphological/morphometrical data were not provided. Bharucha et al. [12] also mentioned the worm from the brain of the patient as S. mansoni without solid morphological evidences of the worm. In a case of American salesman frequently visited India, the worm from his brain was identified as S. mansonoides [27]. Since this species is distributed only in the Americas, whether he was infected in USA or in India remains unknown. Molecular identification of the worm is necessary for such a case. Recently, based on the molecular data, the taxonomic classification and geographical distribution has been drastically changed [45,46]. For example, S. erinaceieuropaei was considered the most common zoonotic Spirometra species in East and Southeast Asian countries. However, this name is now applicable only to the European isolates [45]. For the major Asian isolates previously named S. erinaceieuropaei, Yamasaki et al. [46] recommended to use S. mansoni as the valid name. Together with this proposal, they reported the discovery of new Spirometra species, S. asiana sp. nov. adults from dogs and plerocercoids from wild boars in Japan and its zoonotic nature was proven by the molecular data base search [46]. As the rare human cases, infections with Spirometra decipiens [47] and S. ranarum [48] have been reported. Since validity of those 2 species are still under debate, more extensive molecular epidemiological study is necessary to identify the causative agent(s) for human sparganosis. In particular, the Indian subcontinent and the Middle East are the cross-passing place of animals and their parasites, exact identification of the causative agents of sparganosis in this area is extremely interesting to elucidate the diversification of Spirometra species.
Notes
Author contributions
Conceptualization: Nawa Y
Data curation: Nawa Y, Tanaka M, Yoshikawa M
Formal analysis: Nawa Y, Tanaka M, Yoshikawa M
Investigation: Nawa Y, Tanaka M, Yoshikawa M
Project administration: Nawa Y
Validation: Nawa Y, Tanaka M, Yoshikawa M
Visualization: Nawa Y, Tanaka M
Writing – original draft: Nawa Y
Writing – review & editing: Tanaka M, Yoshikawa M
We have no conflict of interest related to this work.
Acknowledgment
This study is a literature survey and is not a subject of ethical approval.