Clinical characteristics of toxoplasmosis patients in Korea: A retrospective study using health insurance review and assessment service data and electronic medical records
Article information
Abstract
This study aimed to elucidate the clinical characteristics of patients diagnosed with toxoplasmosis in Korea. We collected and analyzed the specific research data of 5,917 patients from the Health Insurance Review and Assessment (HIRA; 2007–2020) and 533 electronic medical records (EMRs; 2003–2021) of Korean patients. The HIRA data showed that toxoplasmosis is an endemic disease that occurs constantly in Korea, with a large proportion of patients complaining of ocular symptoms. Of the 533 patients for whom EMR data were available, 54.6% were diagnosed with toxoplasmosis; ocular toxoplasmosis (35.7%), congenital toxoplasmosis (4.7%), cerebral toxoplasmosis (4.1%), pulmonary toxoplasmosis (0.4%), and toxoplasma hepatitis (0.6%), in order of frequency. In ocular cases, 54.4% of the patients had diverse ocular pathologies. Toxoplasmosis in Korea is characterized by a high frequency of ocular symptoms, most patients are adults, and 51.8% of patients with seropositivity were positive for IgG, suggesting prior infection. This study highlights that patients with ocular symptoms are included in the major diagnosis group for acquired toxoplasmosis in Korea.
Introduction
Toxoplasma gondii is an obligate intracellular protozoan parasite with a global distribution among humans and animals [1–3]. Transmission to humans occurs either by ingesting T. gondii oocysts shed into the environment by cats or by eating raw meat of infected animals [4,5]. Globally, approximately one-third of humans are chronically infected with T. gondii [5–7]. Although T. gondii infection occurs, the seropositivity rates vary by region [2,6]. Regions with high rates of T. gondii infection include Europe and Central and South America, with seroprevalences of 40–60% and >80%, respectively. In the United States, the seroprevalence is >35% [6,8]. Asian countries, including Japan and China, have a relatively low prevalence of the disease, reported to be <10% [6,9–11].
Under normal immune conditions, T. gondii infection is frequently asymptomatic for several years. Therefore, in many cases, infection goes unrecognized [2,5,12]. However, it can be life threatening or cause serious disability in some patients [2,5,12]. In pregnant women with acute infection during pregnancy, congenital toxoplasmosis can occur in the fetus through the amniotic fluid and placenta [1,2,6]. In addition, fatal damage may occur in patients with immunocompromised status (HIV infection, etc.), accompanied by multiple brain lesions and irreversible neurologic disorders [1,2]. However, as mentioned above, individuals with an immunocompetent status will not have any symptoms, or if they do, they will have mild symptoms such as fever, body aches, and intraocular inflammation such as chorioretinitis [1,2,4]. Because toxoplasmosis does not have any specific symptoms, its diagnosis can be challenging in practice [13–15]. In addition, serological testing for T. gondii is recognized as having high false-positive and false-negative rates. Therefore, in practice, a diagnosis is made by combining the patient’s symptoms and various patient characteristics [14,16–18]. Specifically, ocular toxoplasmosis is often diagnosed based on the patient’s clinical symptoms [14,19,20]. Thus, the proper diagnosis and treatment of toxoplasmosis require comprehensive information regarding the characteristics of the patient. For instance, in the United States, a study reported on the characteristics and distribution of toxoplasmosis patients from 2003 to 2012 using the Truven Health MarketScan Database. Most (97.6%) of these patients were over the age of childhood, with a mean age of 37.5 years (±15.5 years).
Meanwhile, Korea, an Asian country, is considered to have a seropositivity rate of approximately 0.8–12.9% [21,22], which is considered relatively lower than that in other countries [5,8]. However, due to the recent rapid increase in international travel, pet ownership, and changing trends in diet, the prevalence of T. gondii infection may be gradually increasing in Korea [8].
Several regional seroprevalence surveys for toxoplasmosis have been conducted in Korea [20–22]. However, these studies had limitations, including a single-center design, short study duration, and small population [10,22,23]. Thus, it is difficult to determine whether they reflect the general characteristics of patients with toxoplasmosis in Korea. Considering that toxoplasmosis is usually diagnosed based on a patient’s symptoms, and given the difficulty of recognizing the infection, there is a need to obtain representative data on patients with toxoplasmosis to understand the current status of toxoplasmosis in Korea. Therefore, it is necessary to collect and analyze information on patients with toxoplasmosis diagnosed with various conditions from multiple institutions.
In this study, we collected information on all toxoplasmosis cases (n=5,917) that occurred in Korea from 2007 to 2020 (14 years) using patient-specific research data from the Health Insurance Review and Assessment (HIRA) service, and we also analyzed the current status of the outbreak toxoplasmosis in Korea. In addition, to analyze the characteristics of patients with toxoplasmosis in Korea, we collected the electronic medical records (EMRs) of 533 patients with toxoplasmosis from 4 upper-level general hospitals located in Seoul and Gyeonggi-do from 2003 to 2021 (19 years). Although the EMR data include information on patients diagnosed with toxoplasmosis and this study represents the largest cohort of its kind conducted domestically, we cannot definitively claim that the EMR data used in this study include all toxoplasmosis patients in Korea. Therefore, to complement the representativeness of the EMR information, it was necessary to use big data from HIRA to obtain information on patients nationwide.
This study sought to analyze information such as patient sex, age, symptoms, results of infection testing, treatment prescription, and history of exposure to risk factors. We retrospectively reviewed and analyzed the collected information. We aimed to establish data representing the characteristics of patients with toxoplasmosis and present the status of toxoplasmosis in Korea to help with its proper diagnosis and treatment.
Materials and Methods
Ethics statement
We retrospectively analyzed the characteristics of patients with toxoplasmosis in Korea using patient-specific research data and the EMR. We conducted the study after obtaining research approval from the institutional review board (IRB) of each of the 4 study hospitals (representative IRB: B-2201-730-104 from Seoul National University Bundang Hospital). Data collected included only information such as sex, age, and symptoms. Personally identifiable information, such as the patient’s medical record number or name, was excluded. There was no risk of infringing on the rights or human rights of the participants, and the need to obtain consent from the patients was waived by the IRB because of the retrospective nature of the study.
Data collection
To determine the characteristics of patients with toxoplasmosis in Korea, we collected information on patients diagnosed with toxoplasmosis from 2007 to 2020 using patient-specific research data provided by the HIRA service (Supplementary Fig. S1A). The data extraction process was as follows. We first extracted the medical record information from the HIRA data for patients with a history of a test for a parasitic infection. The test codes used were C4721 (Parasitic infection-general), C4722 (Parasitic infection-IgG), C4723 (Parasitic infection-IgM), D6421 (Parasitic infection-PCR), D2641 (Parasitic infection-General immunological test), D2642 (Parasitic infection-immunological test-IgG), D2643 (Parasitic infection-immunological test-IgM), and D2644 (Toxoplasma-IgG). From these extracted records, we further extracted information on all patients diagnosed with toxoplasmosis. The ICD-10 codes used were B58 (Toxoplasmosis), B580 (Ocular toxoplasmosis), B581 (Toxoplasma hepatitis), B582 (Toxoplasma meningoencephalitis), B583 (Pulmonary toxoplasmosis), B588 (Toxoplasma with other organ involvement), B589 (Toxoplasmosis, unspecified), and P371 (Congenital toxoplasmosis). We extracted information on a total of 5,917 patients (male, n=2,301; female, n=3,616) from 17,799 records (Supplementary Fig. S1A). From the data, we extracted and analyzed patient information including sex, age, year at the time of diagnosis for toxoplasmosis, diagnosing department, type and region of the hospital.
To investigate the patient characteristics and information in more detail, we collected the EMR data of patients with toxoplasmosis occurring from 2003 to 2021 from 4 upper-level general hospitals (Seoul National University Hospital, n=170; Yonsei Severance Hospital, n=189; Seoul National University Bundang Hospital, n=141; and Inha University Hospital, n=33) located in Seoul and Gyeonggi-do, Korea (Supplementary Fig. S1B). The ICD-10 codes used for the extraction were B58, B580, B581, B582, B583, B588, B589, and P371. Information from 533 patients was extracted, which included demographic information, symptoms, diagnosing department, name of diagnosis, history of exposure to toxoplasmosis risk factors, treatment, and the result of the test for T. gondii infection. No patient data were selectively excluded (Supplementary Fig. S1B). We retrospectively reviewed and analyzed all data.
Statistical analysis
We performed statistical analyses using SAS for Windows version 9.4 (SAS Institute, Cary, NC, USA). Data were presented as a percentage frequency.
Results
Features of toxoplasmosis patients ocurring from 2007 to 2020 in Korea (HIRA)
Data from a total of 5,917 patients were collected, and sex, age, year of diagnosis, region, institution type, and diagnosing department were analyzed. Of the 5,917 patients, 2,301 (38.9%) were male and 3,616 (61.1%) were female (Fig. 1A). The patients were distributed across all age groups, with most patients (26.2%) being in their 30s, followed by those in their 20s and 40s. In total, 3,659 patients were in their 20s to 40s, which accounted for 61.8% of all patients. This indicates that the most economically active population accounts for most cases of toxoplasmosis. In addition, 409 (6.9%) patients were children (aged <10 years); however, among them, 341 patients were between the ages of 0 and 4 years, accounting for 83.4% of the pediatric patients, and they were presumed to have congenital toxoplasmosis (Fig. 1B).
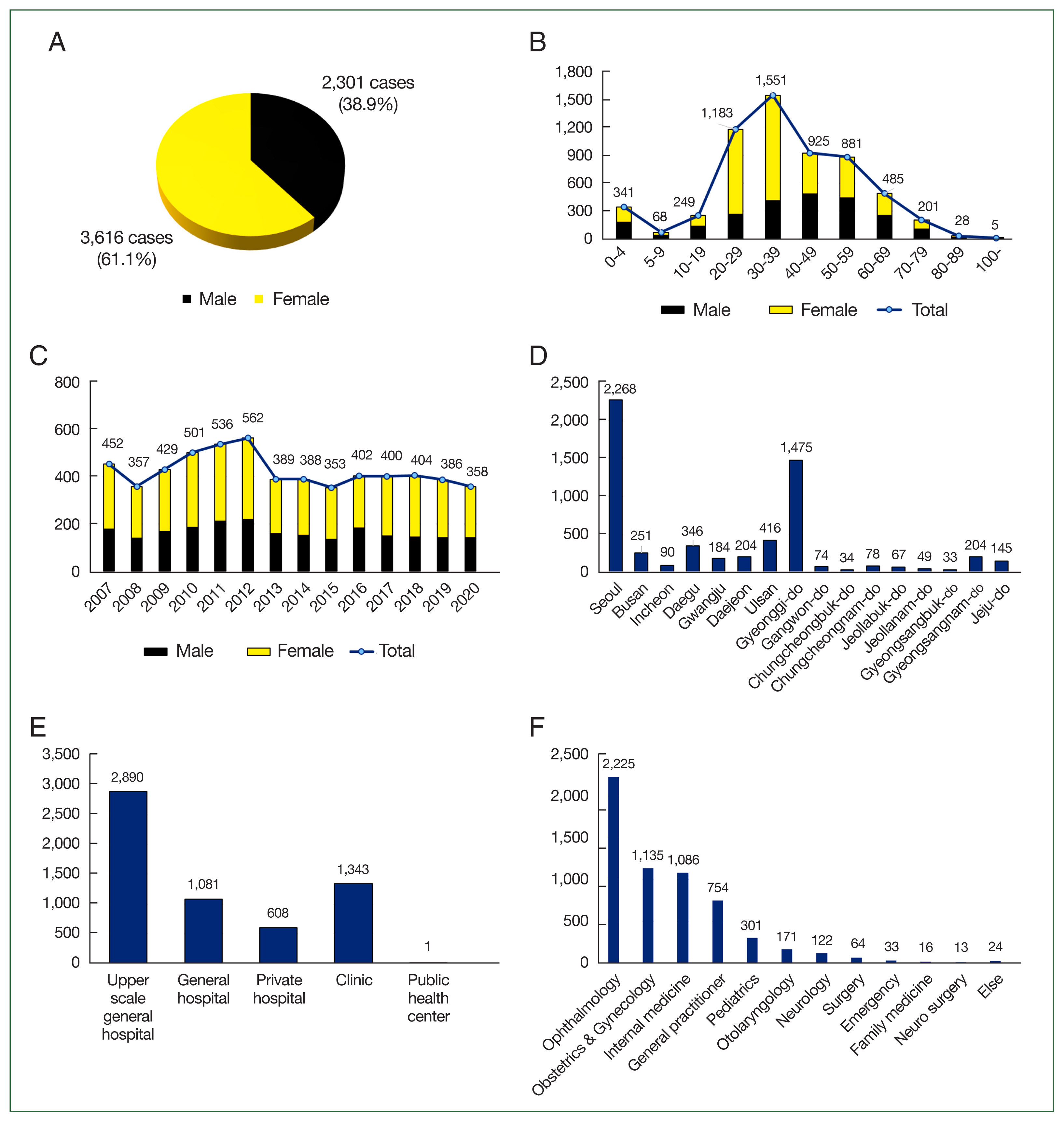
Features of patients with toxoplasmosis occurring from 2007 to 2020 in Korea extracted from patient-specific research data provided by the HIRA Service (total=5,917, black=male, yellow=female). (A) Distribution of patients with toxoplasmosis by sex. (B) Distribution of patients with toxoplasmosis by age at the time of diagnosis. (C–F) These contain multiple counts. (C) Distribution of patients with toxoplasmosis by year of diagnosis. (D) Distribution of patients by geography where the hospital is located. (E) Distribution of patients by institution (hospital type). (F) Distribution of patients by the diagnosing department. This data is an extraction of some of our previous data published in Public health weekly report [24] for the development of this study.
The year of diagnosis refers to the year in which toxoplasmosis was first diagnosed. From 2007 to 2020, the diagnosis appeared to occur constantly without a steady increasing or decreasing trend, and the annual average number of cases was 422.6 (Fig. 1C). This finding confirmed the regional distribution of the hospital where toxoplasmosis was diagnosed. The frequency was the highest in Seoul and Gyeonggi, accounting for 63.3% of the total number of cases (Fig. 1D). Five types of institutions were identified, with the highest frequency observed in upper-level general hospitals (48.8%), followed by clinics, general hospitals, private hospitals, and public health centers (Fig. 1E). Among the departments diagnosing toxoplasmosis in Korea, ophthalmology had the highest frequency of diagnosis (37.6%), followed by obstetrics and gynecology, internal medicine, general medicine, pediatrics, otolaryngology, neurology, surgery, emergency medicine, family medicine, and neurosurgery, in order of frequency. Departments with a frequency of less than 10 cases were grouped as “else”: plastic surgery (7), thoracic surgery (5), orthopedic surgery (4), diagnostic radiology (2), clinical pathology (2), public health (1), rehabilitation medicine (1), nuclear medicine (1), and dermatology (1) (Fig. 1F).
In summary, there has been a consistent incidence of Korean toxoplasmosis for the past 14 years, and a large number of patients with toxoplasmosis belong to the economically active population (20s–40s). The frequency of diagnosis among upper-scale general hospitals located in Seoul and Gyeonggi-do was high, with the highest diagnosis rate observed in ophthalmology departments.
Demographic information of patients with toxoplasmosis (2003–2021, EMR)
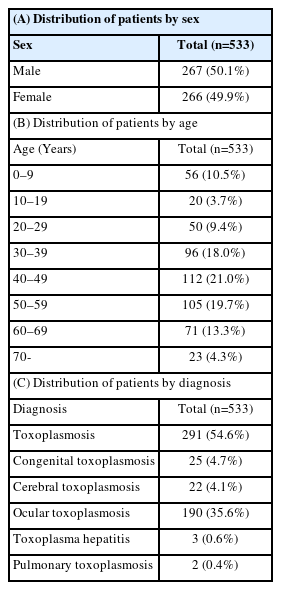
We investigated the comprehensive characteristics of patients with toxoplasmosis in Korea by analyzing patient-specific research data from the HIRA service. To determine the characteristics of patients with toxoplasmosis in more detail, we collected the EMR data of patients with toxoplasmosis and analyzed them from various perspectives. According to the results of the patient-specific research data, most patients with toxoplasmosis were diagnosed in hospitals located in Seoul and Gyeonggi, with an overwhelmingly high number of upper-scale general hospitals. Therefore, we collected the EMR data of 533 patients with toxoplasmosis between 2003 and 2021, representing 4 upper-scale general hospitals located in Seoul and Gyeonggi-do. We extracted information from a total of 533 patients, of whom 267 were male (50.1%) and 266 were female (49.9%) (Table 1A). With regard to the age distribution of the patients, 56 patients (10.5%) were <10 years old (children). And the number of patients aged 40 to 49 years was the highest (21.0%). In addition, the number of patients aged 20 to 59 years accounted for 68.1% of the total (Table 1B). All 533 patients were diagnosed with toxoplasmosis; however, the subdiagnostic names were different, and 7 diagnostic names were confirmed. Toxoplasmosis (54.6%) was the most frequent diagnosis, followed by ocular toxoplasmosis (35.6%), congenital toxoplasmosis (4.7%), cerebral toxoplasmosis (4.1%), toxoplasma hepatitis (0.6%), and pulmonary toxoplasmosis (0.4%) (Table 1C).
Distribution of patients with toxoplasmosis by the diagnosing department and symptoms (2003–2021, EMR)
We analyzed the EMR data to confirm the information on the diagnosing department and symptoms in more detail. Likewise, in previous results (patient-specific research data provided by the HIRA service), among 533 patients, 280 (52.5%) were diagnosed in the ophthalmology department. This was followed by infectious medicine (18.9%), otolaryngology (12.8%), pediatrics (6.7%), neurology (2.8%), obstetrics and gynecology (1.7%), and hematology (0.7%), in order of frequency. Departments with a frequency of ≤ 2 were grouped as “else” (Table 2A). Moreover, 533 patients exhibited different symptoms; however, the symptoms were largely divided into ocular and nonocular symptoms. Of the 533 patients, 290 (54.4%) complained of ocular symptoms and 243 (45.6%) did not (Table 2B). Twelve ocular symptoms were reported; among these, visual disturbance (21.0%) and vision loss (15.8%) were the most frequent. A total of 11 nonocular symptoms appeared in patients, including “else (symptoms that were not grouped into any category)” and “no symptoms,” and the most frequent symptom among them was “lymphadenopathy” (23.6%) followed by asymptomatic cases (10.7%) (Table 2C; these data are an extraction of some of our previous data published in Public Health Weekly Report [24] for the development of this study). Similar to previous patient-specific research data, more than half of toxoplasmosis cases showed ophthalmological symptoms, in which visual disturbance and vision loss was the highest. The lymphadenopathy was the highest in nonohthalmological patients.
Distribution of patients with toxoplasmosis according to the results of tests for T. gondii infection (2003–2021, EMR)
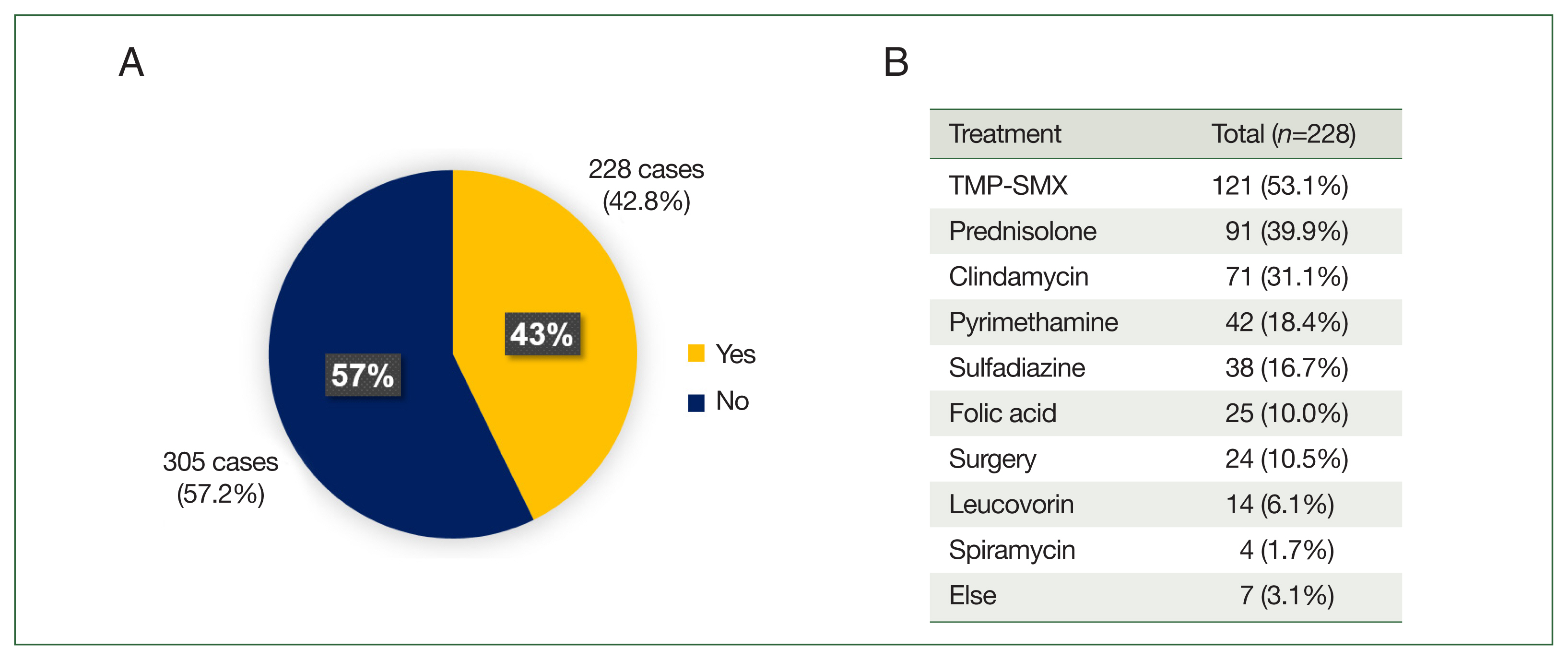
A total of 284 (53.3%) patients tested positive for T. gondii infection (enzyme-linked immunosorbent assay and polymerase chain reaction (PCR)), and 20 (3.7%) patients had negative results. The 229 (43.0%) patients were not tested (Fig. 2A). Looking at the distribution of patients by test type, we noted the largest number of patients with positive results in the Toxo-IgG test (51.8%), followed by the Toxo-IgG+Toxo-IgM test (36.6%), Toxo-IgM (7.7%), PCR (2.5%), Toxo-IgG+PCR (1.1%), and Toxo-IgG+IgM+PCR (0.3%) (Fig. 2B). The ocular symptoms collectively refer to ocular manifestations recognized in this study included uveitis, retinitis, retinopathy, ocular angiopathy, ocular neuropathy, macular lesions, vitreous lesions, visual disturbance, loss of vision, eye floaters, eye discomfort, and scars in the eye. Comparing the frequency of positive test results with the presence of ocular symptoms, patients with ocular symptoms (n=290) showed lower frequency of positive test than those without ocular symptoms (n=243) (Fig. 2C). This means that patients with ocular symptoms were more likely to be diagnosed based on symptoms without a positive test result. The result showing that 51.8% of the patients were IgG positive only, with no IgM detected, indicates that many patients became IgG positive due to previous infections.
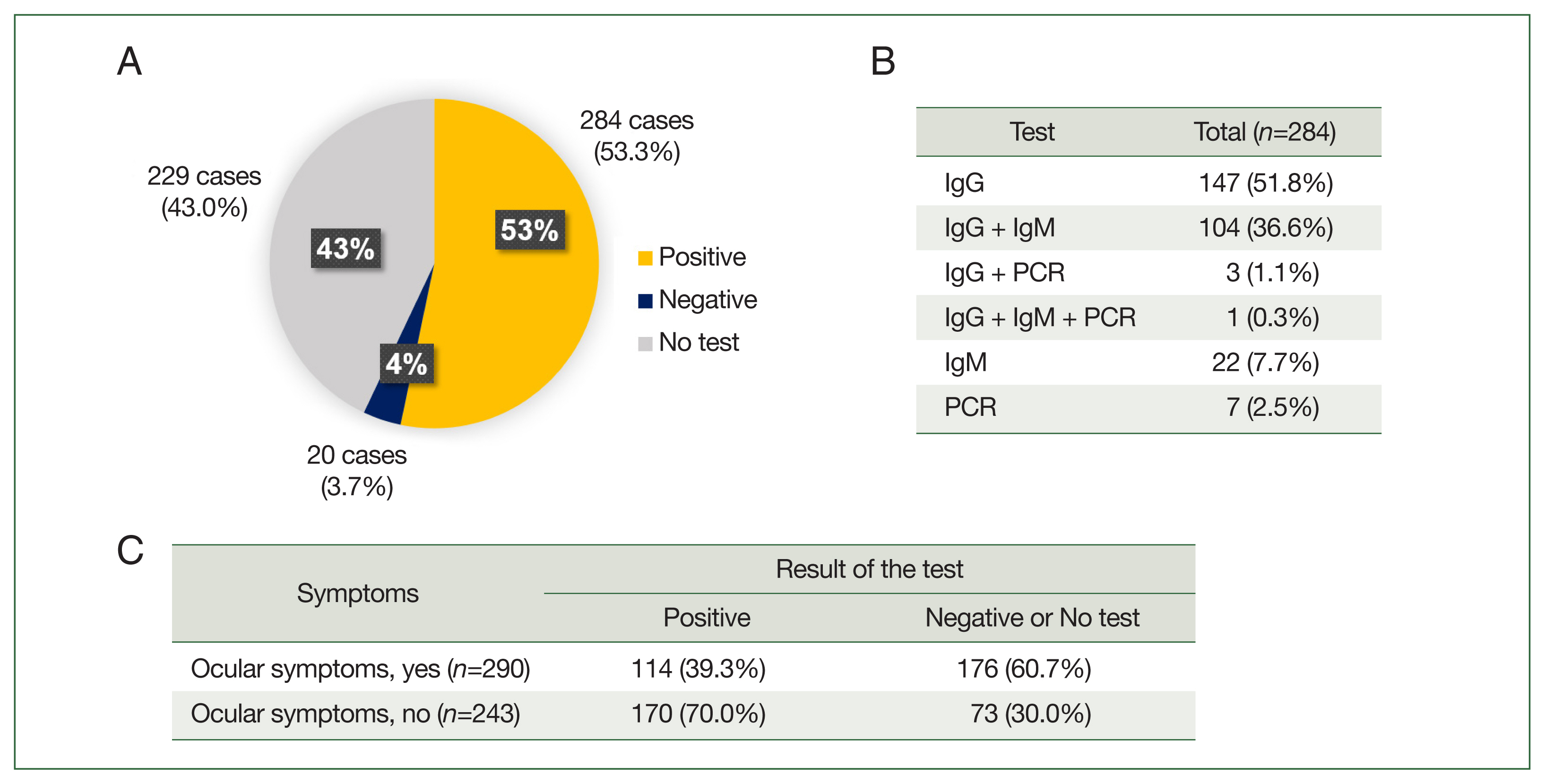
Distribution of patients with toxoplasmosis by the result of T. gondii infection tests (enzyme-linked immunosorbent assay and polymerase chain reaction) conducted in four hospitals (total=533 cases). (A) Distribution of patients with toxoplasmosis depending on the result of the T. gondii infection tests (yellow=positive, blue=negative, gray=no test). (B) Frequency of each test conducted in patients. (C) Distribution of patients by test results according to the presence or absence of ocular symptoms.
Distribution of toxoplasmosis patients according to treatment (2003–2021, EMR)
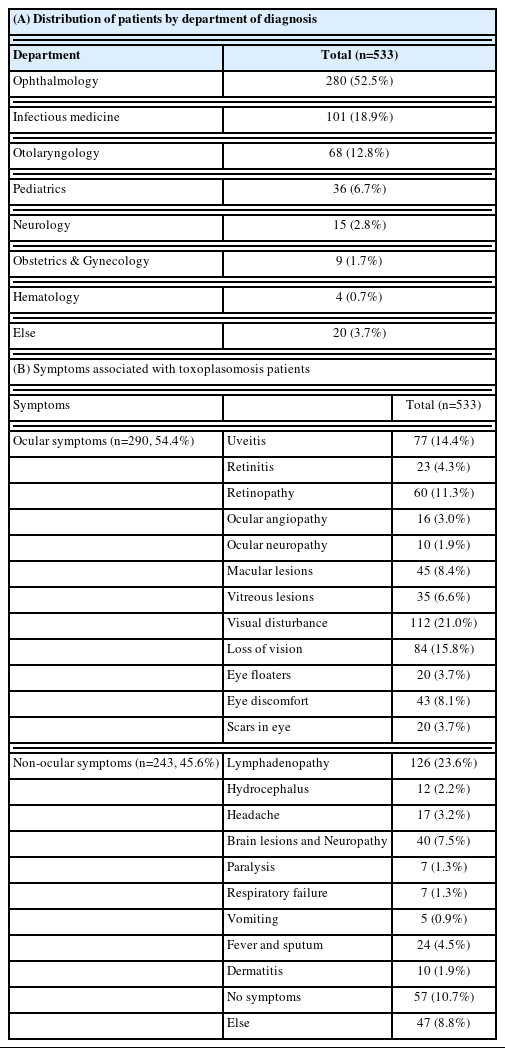
Of the 533 patients analyzed in this study, only 228 (42.8%) had prescriptions for treatment, and the remaining 305 (57.2%) were not prescribed any treatment (Fig. 3A). Among the 228 patients treated, the most frequently prescribed drug was trimethoprim-sulfamethoxazole (53.1%), followed by prednisolone (39.9%), clindamycin (31.1%), pyrimethamine (18.4%), sulfadiazine (16.7%), folic acid (10.0%), leucovorin (6.1%), and spiramycin (1.7%). Moreover, 24 patients (10.5%) underwent surgery, including lymph node removal (Fig. 3B).
Distribution of patients with toxoplasmosis according to exposure history to risk factors for T. gondii infection (2003–2021, EMR)
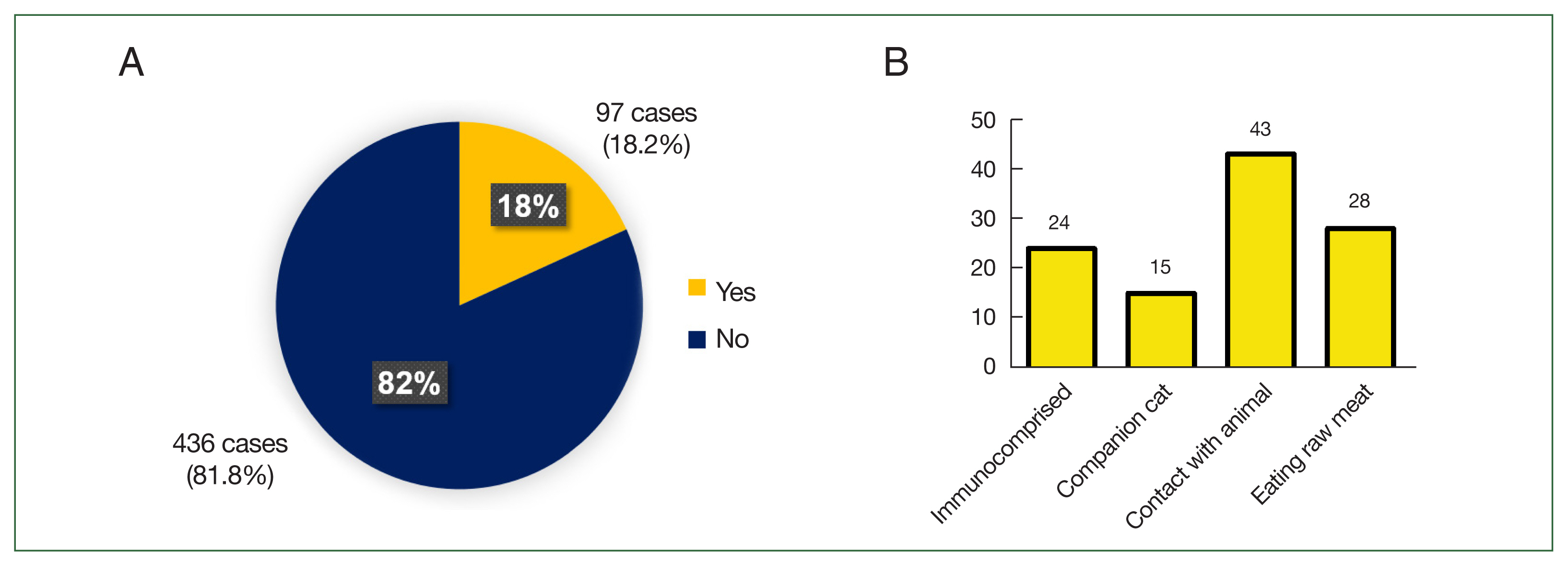
Finally, to investigate the risk factors of toxoplasmosis in Korea, we collected and analyzed more detailed data, such as history of exposure to risk factors for T. gondii infection, from the EMR data. The result confirmed the patient’s exposure history to infection risk factors reported to be the main cause of toxoplasmosis, namely, immunocompromise, presence of companion cats, contact with animals, and eating raw meat. Among 533 patients, 97 (18.2%) had a history of exposure to risk factors (Fig. 4A). Among the risk factors, contact with animals (including stray cats, 44.3%) and eating raw meat (28.9%) showed the highest frequency, followed by immunocompromise (24.7%) and presence of a companion cat (15.5%) (Fig. 4B).
Discussion
Some studies reported the clinical characteristics of toxoplasmosis in Korea; however, these previous studies have limitations, such as a single-center design, short study duration, and small population [10,22,23]. Therefore, it is difficult to determine whether they reflect the general characteristics of patients with toxoplasmosis in Korea. Thus, we analyzed the information of 5,917 patients and 533 patients diagnosed with toxoplasmosis provided by the HIRA service and EMR data from upper-scale general hospitals, respectively, as well as the clinical characteristics of patients with toxoplasmosis. Although no previous studies have investigated the nationwide sex and age distribution of toxoplasmosis in Korea, several studies have reported the prevalence of toxoplasmosis in specific regions, including sex and age distributions [12,25,26]. Researchers have reported that those aged >40 years had significantly higher seroprevalence than younger residents in Seoul and Jeju. In addition, males tended to have a higher seropositive rate than females. However, the sex difference in seroprevalence was not statistically significant [12]. In Cheor-won, 20.6% of males tested positive, whereas 13.1% of females tested positive; the positivitiy rates by age did not follow the general trend but increased gradually with age, reaching the highest rates in males in their 50s (28.7%) and in females in their 40s (20.0%) [25]. In Okcheon-gun, the positivity rates for males and females were reported to be 6.0% and 7.2%, respectively. However, these rates were not significantly different. It was also observed that the positivity rate began to increase from the age of 40 years [26]. In this study, the proportion of females with toxoplasmosis (61.1%) was higher than that of males (38.9%), and the highest number of patients were in their 30s. We also observed a higher proportion of women in this study, with particularly notable differences in the gender ratio of patients in their 20s and 30s. We speculated that these differences may be due to the early detection of T. gondii infection by the TORCH test in women who are pregnant or who are preparing to become pregnant [27]. Because toxoplasmosis is usually asymptomatic and hence can be difficult to recognize, women are tested for toxoplasmosis before or during pregnancy, which gives them a greater chance of being diagnosed at an early stage than men. Of a total of 3,616 women, 2,589 were of childbearing age. Of these, the proportion who had a pregnancy code during the same period was 64.5% (1,670 out of 2,589; data not shown). This can be considered consistent with the findings reported in a study conducted in the United States [28].
Toxoplasmosis was diagnosed in 21 departments, with the highest frequency of diagnosis occurring in the ophthalmology department (52.5%). This result is quite understandable when considered together with the results regarding symptoms and once again shows that the incidence of ocular symptoms is predominant among patients with toxoplasmosis in Korea. Considering the symptoms and diagnosis, the diagnosis rate of ocular toxoplasmosis was expected to be the highest; however, in reality, more cases were diagnosed as toxoplasmosis (54.6%) (Tables 1, 2). Meanwhile, from the HIRA data, we found that 37.6% of patients were diagnosed in the ophthalmology department, whereas the EMR data indicated that this figure was 52.5%. This discrepancy is likely to be due to differences in data composition. In terms of institution type, based on HIRA data, approximately 48.8% of cases were from upper-scale general hospitals among a total of 5 institutions, whereas the remaining 51.2% were from the other 4 institutions (Fig. 1E). Because the EMR data used in this study were obtained from only 4 high-level general hospitals, it is difficult to claim that they fully represent the characteristics of toxoplasmosis patients in Korea. This is also why there was a need for HIRA data in this study, as they complement the lack of representativeness of the EMR data. However, both datasets consistently showed that among patients with toxoplasmosis in Korea, the greatest proportion were diagnosed in the ophthalmology department.
Of the 533 patients diagnosed with toxoplasmosis, only 284 (53.3%) had a positive result for T. gondii infection. The remaining patients had not been tested or had negative results (Fig. 2). This means that they were diagnosed based on their clinical symptoms [14,19]. Specifically, patients with ocular symptoms had a lower frequency of positive tests than patients without ocular symptoms did (Fig. 2). This finding indicates that patients with ocular symptoms were more likely to be diagnosed based on symptoms without a positive test result.
Among all patients, 228 (42.8%) were prescribed or received treatment. The most commonly used drug for toxoplasmosis in Korea was trimethoprim-sulfamethoxazole (prescribed to 53.1% of patients treated) (Fig. 3). Lastly, we reviewed the specific patient information recorded at the time the patient was diagnosed with toxoplasmosis but were not able to confirm anything that could be the route of infection or risk factor for toxoplasmosis (Fig. 4).
In general, the prevalence of toxoplasmosis in Asia, including Korea, is relatively low [6,9–11]. However, based on the results of this study, we believe toxoplasmosis to be endemic and persistent in Korea for the following reasons. First, according to the yearly distribution of patients with toxoplasmosis from 2007 to 2020, the patient incidence rate was consistent by year. Even during strict travel and entry restrictions due to COVID-19, the incidence of toxoplasmosis did not change in Korea. In addition, among 533 patients studied using EMR data, 524 (98.3%) had no history of travel suspected as a route of infection. Taken together, these findings suggest it is reasonable to assume that toxoplasmosis is endemic in Korea rather than imported from other countries.
More than half of the patients with toxoplasmosis complained of ocular symptoms, of which the most frequent were visual disturbance and vision loss. Because patients in areas where type 1 and atypical strains are distributed show severe clinical symptoms and have been reported to have a high incidence of ocular toxoplasmosis [5,29,30], these results serve as evidence confirming, once again, the significance of the findings from previous studies reporting that the KI-1 strain discovered in Korea is genetically similar to the type I strain [5,31]. Although we could not examine the direct correlation between the characteristics of patients and the genotypes of T. gondii in this study, our findings provide important data for predicting the genotype of T. gondii currently circulating in Korea based on the characteristics and genotype reports of patients in known regions.
The fact that only 53.3% of the 533 patients tested positive for infection and 51.8% tested positive only for IgG but not for IgM might be assumed that the symptoms were caused by a previous infection rather than primary infection [32]. Patients with ocular symptoms were likely to be diagnosed baserd on clinical symptoms becase they had a lower frequency of positive infection [14,19].
Althogh we collected all of the information regarding previously known classical risk factors (history of cat and animal breeding [33,34], history of eating raw meat [6,29], etc.) to investigate the risk factors, too few patients had been exposed to risk factors; thus, obtaining clear clues was difficult. Moreover, this type of information may be less accurate because it relies solely on the patient’s statements [35]. Considering the fact that toxoplasmosis has been steadily occurred in Korea [24], an epidemiologic investigation should be conducted to identify the route of infection for appropriate preventive management.
In summary, the characteristics of Korean toxoplasmosis are as follows: toxoplasmosis is estimated to be an endemic disease that has occurred constantly over a 14-year period (2007–2020), with a high proportion of patients complaining of ocular symptoms. The proportion of female patients was higher than that of male patients, the frequency of diagnosis was the highest in upper-scale general hospitals, and the rate of diagnosis was the highest in ophthalmology departments. The most common symptoms were visual disturbance, vision loss, and lymphadenopathy. The frequency of patients diagnosed based on clinical symptoms without a positive result was assumed to be high. This tendency was particularly high among patients complaining of ocular symptoms [14]. In addition, because most patients were adults and IgM seropositivity was low, the symptoms were assumed to be caused by a previous infection [32]. This study is noteworthy because it is the first to present information on patients with toxoplasmosis and various conditions collected from multiple institutions and it is the the largest research on the characteristics of the toxoplasosis patients in Korea. Nevertheless, our study was limited by the lack of detailed pre- and post-diagnosis information or information on infection route. Further research is required to characterize toxoplasmosis in detail by considering the circulating genotype, prevalence, and symptoms of toxoplasmosis in Korea.
Supplementary Information
Notes
Author contributions
Conceptualization: Shin EH
Data curation: Ham DW, Jung BK, Shin JH
Formal analysis: Ham DW, Jung BK, Shin JH
Funding acquisition: Shin EH
Investigation: Ham DW, Kim YJ, Seo KY, Lee SM, Im JH
Methodology: Kim YJ, Seo KY, Lee SM, Im JH, Kwon JR, Lee HS
Project administration: Kwon JR, Lee HS, Hwang KW, Shin EH
Supervision: Shin EH
Validation: Ham DW, Shin EH
Visualization: Ham DW
Writing – original draft: Ham DW
Writing – review & editing: Shin EH
The authors have no competing interests to declare.
Acknowledgment
This study was supported by the research program funded by the Korea Disease Control and Prevention Agency (2021-07-015).