Abstract
An overview of the epidemiological, biological, and clinical studies of Taenia and taeniasis in Taiwan for the past century is presented. The phenomenal observations that led to the discovery of Taenia asiatica as a new species, which differ from Taenia solium and Taenia saginata, are described. Parasitological surveys of the aborigines in Taiwan revealed a high prevalence of taeniasis, which might be due to the culture of eating raw liver of hunted wild boars. Chemotherapeutic deworming trials involving many patients with taeniasis were discussed. Praziquantel was found to be very effective, but sometimes complete worms could not be recovered from the feces after treatment, probably due to the dissolution of the proglottids. Atabrine, despite some side effects, can still be used, in properly controlled dosages, as the drug of choice for human T. asiatica infection if we need to recover the expelled worms for morphological examinations. Research results on the infection of T. asiatica eggs from Taiwan aborigines in experimental animals were also noted. Since the pig serve as the natural intermediate host of T. asiatica and the predilection site is the liver, a differential comparison of other parasitic pathogens that might cause apparently similar lesions is also presented.
-
Key words: Taenia asiatica, Taiwan Taenia, chemotherapy, symptoms, pig liver lesion, Taiwan
EARLY REPORTS OF HUMAN TAPEWORM INFECTIONS IN TAIWAN
Taiwan and the offshore island of Penghu came under the Japanese rule in 1895 under the Treaty of Shimonoseki, when the Ching government of China ceded the islands to the Japanese government. In 1911, the Republic of China was founded, replacing the Ching government in China. However, Japanese ruled Taiwan until the end of the Second World War in 1945. Then, the Nationalist government of China came over and took control of Taiwan until this day.
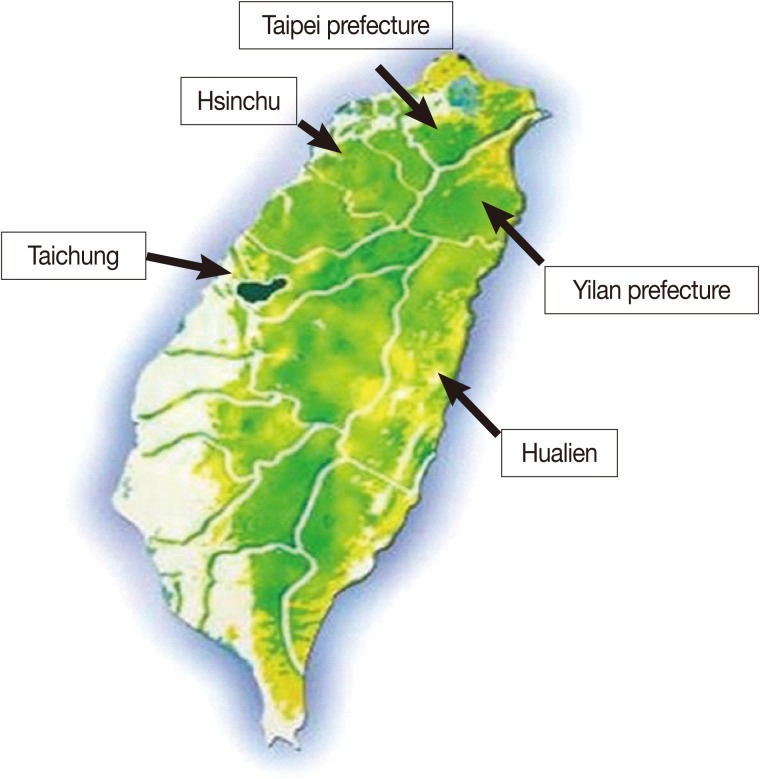
The first report of taeniasis in Taiwan was made by Oi in 1915 [
1], when he found 2 positive cases in a fecal parasitological survey of 301 persons composing of prisoners, students, and patients in Taichung, central Taiwan. In 1927, Oi [
2] reported that 2 Japanese immigrants were shedding taeniid eggs out of 220 people surveyed for intestinal parasites in Hualien port city. Then, in 1928, Yokogawa and his associates [
3] reported that out of 812 aborigines surveyed in Hsinchu, 163 (20%) were found to be excreting taeniid eggs. The locations of the study areas are shown in
Fig. 1.
It was not until 1952, when Huang and associates [
4-
6] reported that 20.5% (130/634) of the aborigines surveyed in Wulai, Taipei prefecture [
4], 16.3% (300/1,839) in Lotung, Ilan prefecture [
5], and 9.7% (49/503) in Nan-ao, Ilan prefecture [
6], were positive for taeniid eggs shedding, respectively. Since then, about 20 reports on the prevalence of taeniasis in humans in Taiwan had been published in the 1960s, all under the assumption that the causative agent was
Taenia saginata.
Taenia solium is extremely rare in Taiwan with only 5 cases being reported from 1957 to 1970 by Hsieh in southern Taiwan (Cited in Chung & Liu [
7]).
DISCOVERY OF TAIWAN TAENIA
It was only in 1966, when Huang and associates [
8] first proposed that the
Taenia tapeworm infecting the Taiwan aborigines in such high prevalences might not be the same as the classical
T. saginata. They observed that the aborigines do not have access to beef, and their main animal protein source came mainly from wild boars and other hunted wildlife [
8,
9].
It was only in the 1970s that experimental infection of the eggs of Taiwan taeniid and that of the American
T. saginata was carried out in bovine calf and goats for comparison [
10]. The cysticerci of the American isolate were found in the muscles of the neck, rib, heart, and legs but not in the liver. Whereas, about half of the cysticerci of the Taiwan isolate were found in the liver of the infected calf. Moreover, no hooklets were observed in any of the American isolate cysticerci, but 88% of the Taiwan isolate cysticerci had hooklets on their rostellum. In addition, it was also observed that the various morphormetric parameters, such as the body length and width, protoscolex, and sucker diameter were larger for the American isolate than the Taiwan isolate. All the cysticerci of the Taiwan isolate in the experimentally infected goat were recovered only from the liver, and all of them had hooklets. It was later observed that the cysticerci of Taiwan
Taenia could not grow in the liver of the cow because they degenerate at 2 months post-infection.
In the 1980s, it was apparently becoming clear that Taiwan
Taenia might be a different species than that of the classical
T. saginata, based on the site of predilection being in the liver, its developmental morphology, and the pig serving as its natural intermediate host (
Table 1) [
11,
12]. The paradox of this parasite epidemiology is that in the area where
T. saginata-like infection in humans is widely prevalent, the inhabitants had little chance of eating beef, and
Cysticercus bovis were not present in the bovids in that area. However, the inhabitants had the habit and chance of eating raw liver of pigs. Then, Fan and collaborators from other countries observed that taeniids with similar characteristics to Taiwan
Taenia were also found in other Asian countries such as Korea (Cheju-do Island), Indonesia (Samosir Island), the Philippines, Thailand (Chiang Mai), and Myanmar [
13-
15].
In the early 1990s, despite the overwhelming genetic evidence that the Taiwan
Taenia might be a new species, American and Australian workers still suggested that it would be more appropriate to classify it as a subspecies of
T. saginata [
16]. Thus, in 1995, Fan and associates [
17] proposed that the Taiwan
Taenia be named as
T. saginata asiatica, and the classical
T. saginata found in America and Europe as
T. saginata saginata. Today, that parasite, which is prevalent in many Asian countries, is now internationally recognized as a distinct species, namely,
T. asiatica, mainly through the efforts and description of Eom and colleagues in Korea [
18,
19]. Fan and his coworkers published more than 100 papers on
T. asiatica. He passed away on 2 September, 2008, due to an aortic aneurysm at the age of 86.
EXPERIMENTAL ANIMAL INFECTION WITH T. ASIATICA EGGS
Cysticerci of
T. asiatica have been recovered mainly from the liver of pig, calf, goat, and monkey after oral inoculation of the eggs. However, only calcified and degenerated cysticerci were observed in the liver of goat and monkey [
13,
20].
T. asiatica cysticerci were found to be able to develop to maturity in scid mice [
21,
22] and also Mongolian gerbil [
21] after subcutaneous injection of oncospheres. These cysticerci were able to grow to maturity in the rodents and then develop into the tapeworm stage in the rodent alternative definitive host or in humans [
23].
CLINICAL MANIFESTATIONS AND CHEMOTHERAPY OF TAENIASIS PATIENTS IN TAIWAN
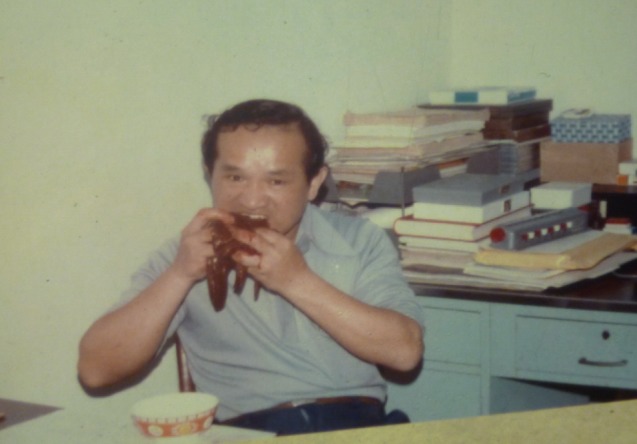
Humans infected with taeniasis infection experience many types of clinical symptoms but not all of them are the same.
Table 2 shows the clinical manifestation of taeniasis among Aborigines in Taiwan and these patients were most probably infected with the Taiwan
Taenia. To study the various symptoms of Taiwan taeniasis and to obtain the adult worm, many brave researchers had volunteered to orally infect themselves with cysticerci of
T. asiatica by eating the raw pig liver (
Fig. 2).
Since there were many taeniasis patients in Taiwan through the 6 decades, many types of drugs had been used in the chemotherapeutic deworming trials. These drugs include atabrine (quinacrine), dichlorophen (arecoline), bithionol (bithin), yomesan (niclosamide), acanil (mebendazole), albendazole, and praziquantel (
Table 3). It was observed that niclosamide (
Table 4) [
24], albendazole (
Table 5) [
25,
26], and mebendazole [
27] were not very efficacious against human
T. asiatica infections. However, Rim et al. [
28,
29] stated that albendazole was effective for treatment of
T. saginata and
T. solium. Nevertheless, it must be noted that the efficacy of anthelmintic drugs can be influenced by the patient's physiological status such as being in a fasting or non-fasting condition [
30].
Praziquantel, at a single dose of 150 mg, was found to be the most effective against
T. asiatica infection in humans, without causing any side reaction [
27]. This efficacy is followed by atabrine and then by niclosamide [
31]. However, sometimes no complete worms could be recovered from the feces of the patient after treatment, probably due to dissolution of the worm by the drug.
Atabrine, despite producing some side effects, can still be used, in properly controlled dosages, as the drug of choice for human
T. asiatica infection if we need to recover the expelled worms for morphological examinations. It can be taken orally at a total of 1 gm divided into 2 equal doses given at 30 min interval, after the patient is fasted and given 4 gm of sodium bicarbonate to prevent vomiting. The patient should then be given a purgative of magnesium salt (25 g in 1 liter of water) at 1.5 hr after taking the second dose. The expelled worm can then be collected from the feces within a few hours. To date, the most number of worms collected from a single patient in Taiwan was 24 specimens, after medication with atabrine (
Fig. 3).
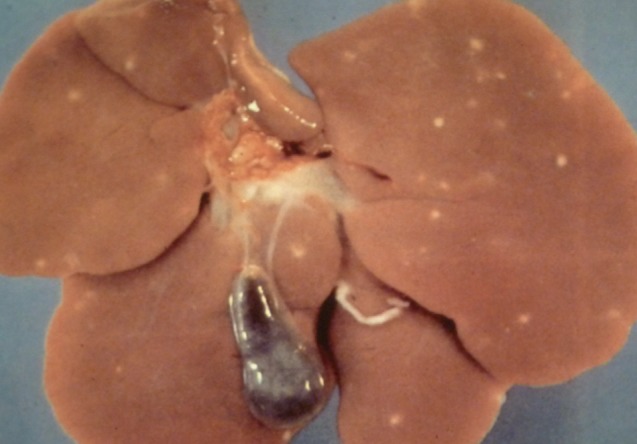
LESIONS IN THE PIG LIVER
The pig serves as the natural intermediate host of
T. asiatica and the site of predilection is in the liver (
Fig. 4). However, other parasitic pathogens might also cause apparently similar hepatic lesions. A differential comparison of the hepatic lesions caused by other parasites is presented in
Table 6 [
32-
36].
PRESENT STATUS OF TAENIASIS IN TAIWAN
T. asiatica is still present in Taiwan today but in only some aborigines who live in the mountainous areas. However, the cases are getting rarer with the improvement of rural medical health services. Taenia asiatica has always been there and has come a long way for its recognition. We just need to train our eyes to see in different dimension.
References
- 1. Oi T. Examination of eggs of intestinal parasites in Central Taiwan. J Formos Med Assoc 1915;154:816-825.
- 2. Oi T. Intestinal parasites of Japanese immigrants in Eastern Formosan, especially the distribution of the hookworm. J Formos Med Assoc 1927;263:224-239.
- 3. Yokogawa S, Kobayashi H, Ko C. The stool examination in aborigines in Shinchiku Shu. J Formos Med Assoc 1928;283:1194.
- 4. Huang WH, Loo WT, Hsieh HC, Wu CL. Parasitological investigation on the aborigines in Taipeh Prefecture, Formosa. Part I. Parasitological investigation on the aborigines in Urai district. J Formos Med Assoc 1952;51:95-118.
- 5. Huang WH, Loo WT, Huang CH, Wu CL. Parasitological investigation on the aborigines in Taipeh Prefecture, Formosa. Part II. Parasitological investigation on the aborigines in Lotung district. Mem Fac Med Natl Taiwan Univ 1952;2:7-32.
- 6. Huang WH, Loo WT, Tseng PT, Wu CL. Parasitological investigations on the aborigines in Taipeh Prefecture, Formosa. Part III. Parasitological investigation on the aborigines in Nan-ao district. Mem Fac Med Natl Taiwan Univ 1952;2:33-47.
- 7. Chung WC, Liu JC. Prevalence and treatment of taeniasis saginata in aborigines in Wufeng district, Hsinchu county, North Taiwan. Proceedings of the 7th SEAMEO Regional Seminar/Laboratory Meeting on Tropical Medicine and Public Health. The Infectious Diseases of the Gastrointestinal system in Southeast Asia and Far East. Sept. 28-Oct. 2, 1970; Taipei, Taiwan: 275-276.
- 8. Huang SW, Khaw OK, Liu CY. Studies on Taenia species prevalent among the aborigines in Wulai district Taiwan. Part I. On the parasitological fauna of the aborigines in Wulai district. Bull Inst Zool (Acad Sin) 1966;5:87-91.
- 9. Huang SW. Studies on Taenia species prevalent among the aborigines in Wulai district Taiwan. Part II. On the species of Taenia. Bull Inst Zool (Acad Sin) 1967;6:29-34.
- 10. Chao D, Fan PC, Liu HY, Lee KM, Chung WC. Taenia saginata (?) among Taiwan aborigines is probably a new species. Chin J Microbiol 1979;12:108-109.
- 11. Fan PC, Chan CH, Chao D, Chung WC. Studies on some problems of taeniasis among aborigines in Taiwan. Program and Summary of Sino-Japanese Seminar on Parasitic Zoonoses. August 28-29, 1982; Hirosaki, Japan: 110-115.
- 12. Fan PC, Chan CH, Chung WC, Chen CC, Wong MM, Chao D, Huang SH, Hsu MC, Wu CC, Chen YA. Studies on taeniasis in Taiwan. IV. Current status of epidemiological, experimental and morphological aspects of Taiwan Taenia. Proceedings of Sino-Japanese Symposium on Parasitic Zoonoses. July 11-12, 1986; Osaka, Japan: 100-107.
- 13. Fan PC, Chung WC, Lin CY, Soh CT, Lee KT, Kosman MI, Kosin E, Depari AA, Napitupulu T. Studies on taeniasis in Taiwan VI. Is Taenia saginata from Taiwan, Korea and Indonesia a new species. Chin J Parasitol 1988;1:56-70.
- 14. Bowles J, McManus DP. Genetic characterization of Asian Taenia, a newly described taeniid cestode of humans. Am J Trop Med Hyg 1994;50:33-44.
- 15. Fan PC, Chung WC, Lin CY, Chen TM, Wu CC. Studies on taeniasis in Taiwan. IX. Prevalence of taeniasis among Atayal, Bunun and Ami aborigines in Hualien county, East Taiwan. Chin J Parasitol 1989;2:47-59.
- 16. Chung WC, Fan PC, Chan CH, Chen YA, Hsu MC, Wu CC, Chao D. Studies on taeniasis in Taiwan. II. Pravelence of taeniasis among aborigines in Lanyu (Orchid Island) district, Taitung county, East Taiwan with reference to domestic pigs (Lanyu strain), which can be considered as the intermediate host of Taiwan Taenia (?). Proceed First Sino-American Symp. 1987, pp 78-90.
- 17. Fan PC, Lin CY, Chen CC, Chung WC. Morphological description of Taenia saginata asiatica (Cyclophyllidea: Taeniidae) from man in Asia. J Helminthol 1995;69:299-303.
- 18. Eom KS, Rim HJ. Morphologic descriptions of Taenia asiatica sp. n. Korean J Parasitol 1993;31:1-6.
- 19. Eom KS, Rim HJ. Epidemiological understanding of Taenia tapeworm infections with special reference to Taenia asiatica in Korea. Korean J Parasitol 2001;39:267-283.
- 20. Chung WC, Lin CY, Fan PC. Ectopic locations of Taenia saginata asiatica in the abdominal cavity of domestic pig and monkey. J Parasitol 1996;82:1032-1034.
- 21. Ito A, Chung WC, Chen CC, Ito M, Endo S, Okamoto M, Fan PC. Human Taenia eggs develop into cysticerci in scid mice. Parasitology 1997;114:85-88.
- 22. Chang SL, Nonaka N, Kamiya M, Kanai Y, Ooi HK, Chung WC, Oku Y. Development of Taenia saginata asiatica metacestodes in SCID mice and its infectivity in human and alternative definitive hosts. Parasitol Res 2005;96:95-101.
- 23. Chang SL, Ooi HK, Nonaka N, Kamiya M, Oku Y. Development of Taenia asiatica cysticerci to infective stage and adult stage in Mongolian gerbils. J Helminthol 2006;80:219-223.
- 24. Fan PC, Chung WC, Lin CY, Wu CC. Efficacy of niclosamide against aboriginal taeniasis in Taiwan. Zhonghua Yi Xue Za Zhi (Taipei) 1990;45:241-245.
- 25. Chung WC, Fan PC, Lin CY, Wu CC. Poor efficacy of albendazole for the treatment of human taeniasis. Int J Parasitol 1991;21:269-270.
- 26. Fan PC, Chung WC, Lin CY. Review: Therapeutic efficacy of mebendazole, praziquantel, albendazole and niclosamides for the treatment of Taiwan Taenia infection. Proceed Second Asia-Pacific Congr Parasitic Zoon. July 24-26, 1992; 40-52.
- 27. Fan PC, Chung WC, Chan CH, Chen YA, Cheng FY, Hsu MC. Studies on taeniasis in Taiwan. V. Field trial on evaluation of therapeutic efficacy of mebendazole and praziquantel against taeniasis. Southeast Asian J Trop Med Public Health 1986;17:82-90.
- 28. Rim HJ, Joo KH, Lee JS, Wang JS. Anthelmintic effect of albendazole (Zentel R) against helmintic infections. Korean J Rural Med 1984;9:67-73.
- 29. Rim HJ, Joo KH, Park HS. Anthelmintic effect of albendazole against Taenia saginata and Taenia solium infections. J Korean Soc Chemother 1989;7:29-39.
- 30. Fan PC, Chung WC, Lin CY, Wu CC. The effect of fasting on the treatment of taeniasis. Chin J Parasitol 1990;3:93-95.
- 31. Fan PC, Chung WC, Lin CY, Chan CH. Clinical manifestations of taeniasis in Taiwan aborigines. J Helminthol 1992;66:118-123.
- 32. Iburg T, Johansen MV, Leifsson PS, Willingham AL, Lindberg R. Hepatic changes in congenital Schistosoma japonicum infections in pigs. J Comp Pathol 2007;136:250-255.
- 33. Kamiya M, Ooi HK, Oku Y, Okamoto M, Ohbayashi M, Seki N. Isolation of Echinococcus multilocularis from the liver of swine in Hokkaido, Japan. Jpn J Vet Res 1987;35:99-107.
- 34. van Veen S. Facioliasis (Fasciola gigantica) in West Africa: A review. Vet Bull 1980;50:529-533.
- 35. Soulsby EJL. Helminths, Arthropods and Protozoa of Domesticated Animals. 1982, 7th ed. London, UK. Bailliere Tindall Publ. Ltd. pp 1-809.
- 36. Taira K, Saeed I, Permin A, Kapel CM. Zoonotic risk of Toxocara canis infection through consumption of pig or poultry viscera. Vet Parasitol 2004;121:115-124.
Fig. 1Map of Taiwan showing the locations where early epidemiological taeniasis surveys were carried out.

Fig. 2A volunteer, Dr. Chung WC, trying to infect himself with Taenia asiatica by eating raw wild boar liver that contained cysticerci.

Fig. 3A Taenia asiatica patient, Mr. Chen Chin-Fu, with 24 strobilae that were purged from him after using atabrine.

Fig. 4Cysts of Taenia asiatica in the liver of a pig.

Table 1.Comparison of
Cysticercus bovis from Taiwan and American Origins
a
Table 1.
|
Origin |
Intermediate host |
Cysticercus locality |
Cysticercus examined |
Hooklets on cyst
|
|
Absent |
Present |
|
Taiwan aborigine |
Calf (cow) |
Liver |
33 |
6 (18.2%) |
27 (81.8%) |
|
Taiwan aborigine |
Goat |
Liver |
16 |
0 (0.0%) |
16 (100%) |
|
American volunteer |
Calf (cow) |
Musclesb |
39b
|
39 (100%) |
0 |
Table 2.Clinical manifestation of taeniasis among aborigines in Taiwan
a
Table 2.
|
Clinical signs |
No. of cases (Total 1,258) |
% |
|
Proglottids shed in feces |
1,200 |
95 |
|
Pruritis at perianal area |
963 |
77 |
|
Nausea |
584 |
46 |
|
Abdominal pain |
564 |
45 |
|
Dizziness |
523 |
42 |
|
Increased appetite |
374 |
30 |
|
Headache |
321 |
26 |
|
Diarrhea |
222 |
18 |
|
Weakness/Lethargy |
210 |
17 |
|
Feeling of hunger |
200 |
16 |
|
Constipation |
135 |
11 |
|
Weight loss |
71 |
6 |
|
Abdominal discomfort |
66 |
5 |
|
Tiredness |
53 |
4 |
|
Loss of appetite |
52 |
4 |
|
Vomiting |
50 |
4 |
|
No appetite despite fasting |
14 |
1 |
|
Muscular pain |
13 |
1 |
|
Stomach discomfort |
9 |
< 1 |
|
Gastric pain |
8 |
< 1 |
|
Feeling sleepy |
4 |
< 1 |
|
Convulsion |
2 |
< 1 |
|
Anxiety |
2 |
< 1 |
|
Skin pruritis |
1 |
< 1 |
|
Respiratory irregularity |
1 |
< 1 |
|
Hunger pain |
1 |
< 1 |
Table 3.Chemotherapeutic agents for cestode infections
Table 3.
|
Chinese herbs (plant name, effective compound) |
Drug name |
|
Pumpkin seed (Cucurbita pepo, Cucurbitine) |
Atabrine (Quinacrine) |
|
Betel nut (Areca catechu, Arecoline) |
Dichlorophen |
|
Somegranate root (Pumca granatum, Pelletierrine) |
Bithionol (Bithin) |
|
Filix mas (Oleoresin aspidium) |
Yomesan (Niclosamide) |
|
Kamala (Mollotus philippinensis) |
Acanil (Mebendazole) |
Table 4.Efficacy of niclosamide in the treatment of human taeniasis
a
Table 4.
|
No. of worms expelled |
No. of cases |
Deworming results
|
Questionaire
|
|
Worm |
With scolex |
No. cases |
Worm expelled |
|
1 |
13 |
13 |
4 |
3 |
3c
|
|
2 |
3 |
6 |
2 |
0 |
|
|
3 |
2 |
6 |
0 |
0 |
|
|
8 |
1 |
8 |
5 |
0 |
|
|
Total |
19b
|
33 |
11 |
3 |
3 |
Table 5.Efficacy of albendazole in the treatment of human taeniasis
a
Table 5.
|
Dose (mg×days) |
No. cases treated |
No. follow-up exam. |
Deworming results
|
Retreatmentb
|
Cure rate (%) |
|
Worm |
Not-noticed |
No. |
cases/cured |
|
400×1 |
54 |
30 |
22 |
8 |
30 |
0 |
0.0 |
|
800×1 |
10 |
8 |
7 |
1 |
8 |
0 |
0.0 |
|
800×2 |
20 |
14 |
11 |
3 |
14 |
2 |
14.3 |
|
800×3 |
10 |
7 |
5 |
2 |
4 |
2 |
50.0 |
|
1,200×2 |
10 |
6 |
5 |
1 |
6 |
3 |
50.0 |
|
1,200×3 |
12 |
11 |
8 |
3 |
4 |
2 |
50.0 |
|
Total |
116 |
76 |
58 |
18 |
76 |
9 |
12.0 |
Table 6.Parasites that produce lesions in the liver of pigs
a
Table 6.
|
Parasite |
Location |
Principal lesions in the liver |
|
Clonorchis sinensis
|
Bile duct |
Dilation of the bile duct, periductal fibrosis |
|
Opisthorchis tenuicollis
|
Bile duct |
Dilation of the bile duct, periductal fibrosis |
|
Dicrocoelium dendriticum
|
Bile duct |
Dilation of the bile duct, periductal fibrosis |
|
Fasciola hepatica
|
Bile duct |
Dilation of the bile duct, periductal fibrosis |
|
Fasciola gigantica
|
Bile duct |
Dilation of the bile duct, periductal fibrosis |
|
Schistosoma japonicum
|
Liver |
Pinpoint white spot, granuloma |
|
Taenia hydatigena
|
Liver |
White cyst |
|
Echinococcus granulosus
|
Liver |
White cyst |
|
E. multilocularis
|
Liver |
White cyst |
|
Taenia asiatica (Taiwan taenia) |
Liver |
White cyst |
|
Ascaris suum
|
Liver |
Pinpoint white spot |
|
Toxocara canis
|
Liver |
Pinpoint white spot |
|
Stepahnurus dentatus
|
Liver |
Pinpoint white spot |