Abstract
Primary amebic encephalitis (PAM) is a devastating central nervous system infection caused by Naegleria fowleri, a free-living amoeba, which can survive in soil and warm fresh water. Here, a 43-year-old healthy male was exposed to warm freshwater 5 days before the symptom onset. He rapidly developed severe cerebral edema before the diagnosis of PAM and was treated with intravenous conventional amphotericin B while died of terminal cerebral hernia finally. Comparing the patients with PAM who has similar clinical symptoms to those with other common types of meningoencephalitis, this infection is probably curable if treated early and aggressively. PAM should be considered in the differential diagnosis of purulent meningoencephalitis, especially in patients with recent freshwater-related activities during the hot season.
-
Key words: Naegleria fowleri, primary amebic meningoencephalitis, cerebral hernia, amphotericin B
INTRODUCTION
Naegleria fowleri is a free-living amoeba that can survive in soil and warm fresh water [
1]. When humans are exposed to contaminated water, amoeba enters the nasal cavity of the host and travels through the nasal mucosa, followed by moving along the cribriform plate and olfactory nerve, finally reaching the olfactory bulbs. Consequently, it destroys the central nervous system (CNS), thereby causing primary amebic meningoencephalitis (PAM) [
2]. Although the infection is rare, it is fatal. To date, there have been only 7 cases reported in China, and none of them survived because of a severe increase of cerebrospinal fluid (CSF) and intracranial pressure.
CASE RECORD
A 43-year-old, previously healthy male, visited the emergency department of Zhejiang Provincial People’s Hospital, Hangzhou, China, on 20 August 20, 2016, with a 2-day history of persistently occipital headache, fever, myalgia, and fatigue. He was a tourist from Shenzhen, China, which is a large city located in southern China. Before visiting the Hospital, he had self-administered some NSAIDs (non-steroidal anti-inflammatory drugs) without achieving any relief. The headache was excruciating and intolerable.
At the time of Hospital admission, his vital signs were as follows: temperature, 39.1°C; pulse, 89 beats/min; respiratory rate, 33 breaths/min; blood pressure, 133/56 mmHg. Physical examination revealed the presence of positive meningeal irritation sign and left Babinski sign, while the CT scan of the head was normal. The routine blood test showed the leucocyte count of 10,480 cells/mm3 with 80% neutrophils and C-reactive protein (CRP) of 2.6 mg/L. Then, lumbar puncture was dispensed, the CSF was turbid with high pressure (300 mmHg), positive Pandy’s test, very low level of glucose (<1 mmol/L), highly elevated leukocytes (1,170 cells/mm3 with 83% neutrophils) and protein (>300 mg/dl). According to the above results, the patient was diagnosed with bacterial meningitis and administered empirical treatment. On August 21, he was intubated and sedated because of tachypnea and agitation, and then, transferred to the intensive care unit (ICU).
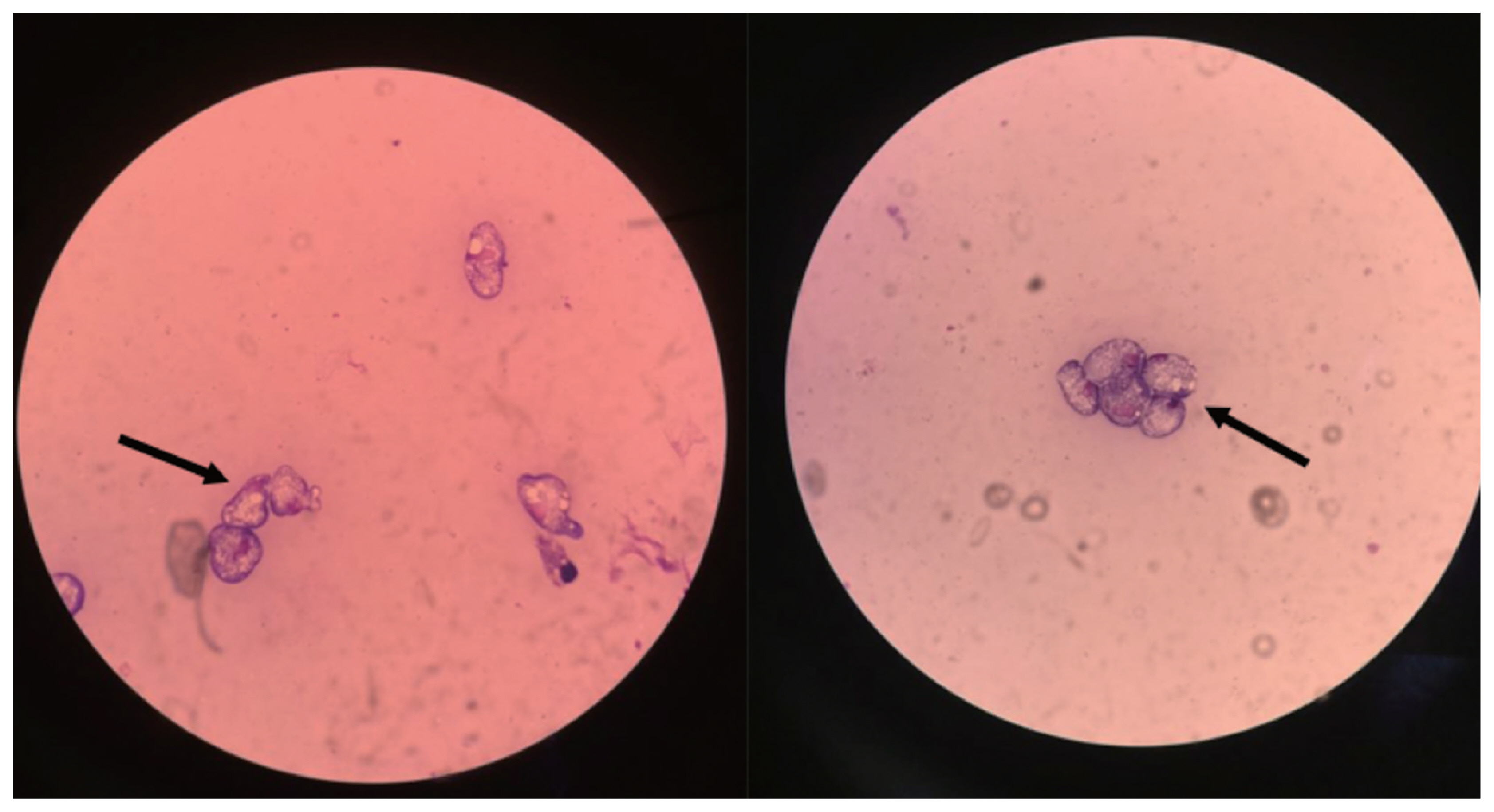
Considering the possibility of pyogenic meningitis, he was treated with 2 g meropenem every 8 hr, 600 mg linezolid every 12 hr intravenously, as well as, mannitol and dexamethasone. On the second evening of ICU stay, he suddenly developed a decreased responsiveness; the pupillary examination revealed the presence of fixed and dilated pupils. Thus, a 150 ml of 20% mannitol was infused for 30 min, followed by CT scanning. The brain CT scan demonstrated hydrocephalus, brain swelling, hyperdense interhemispheric fissure cistern, and supra sella cistern sign that confirmed cerebral hernia and meningoencephalitis. Subsequently, the external ventricular drainage was placed, and CSF samples were collected and reexamined. On August 24, he was eventually diagnosed with PAM as the trophozoites of
N. fowleri were identified in the CSF via Wright-Giemsa staining (
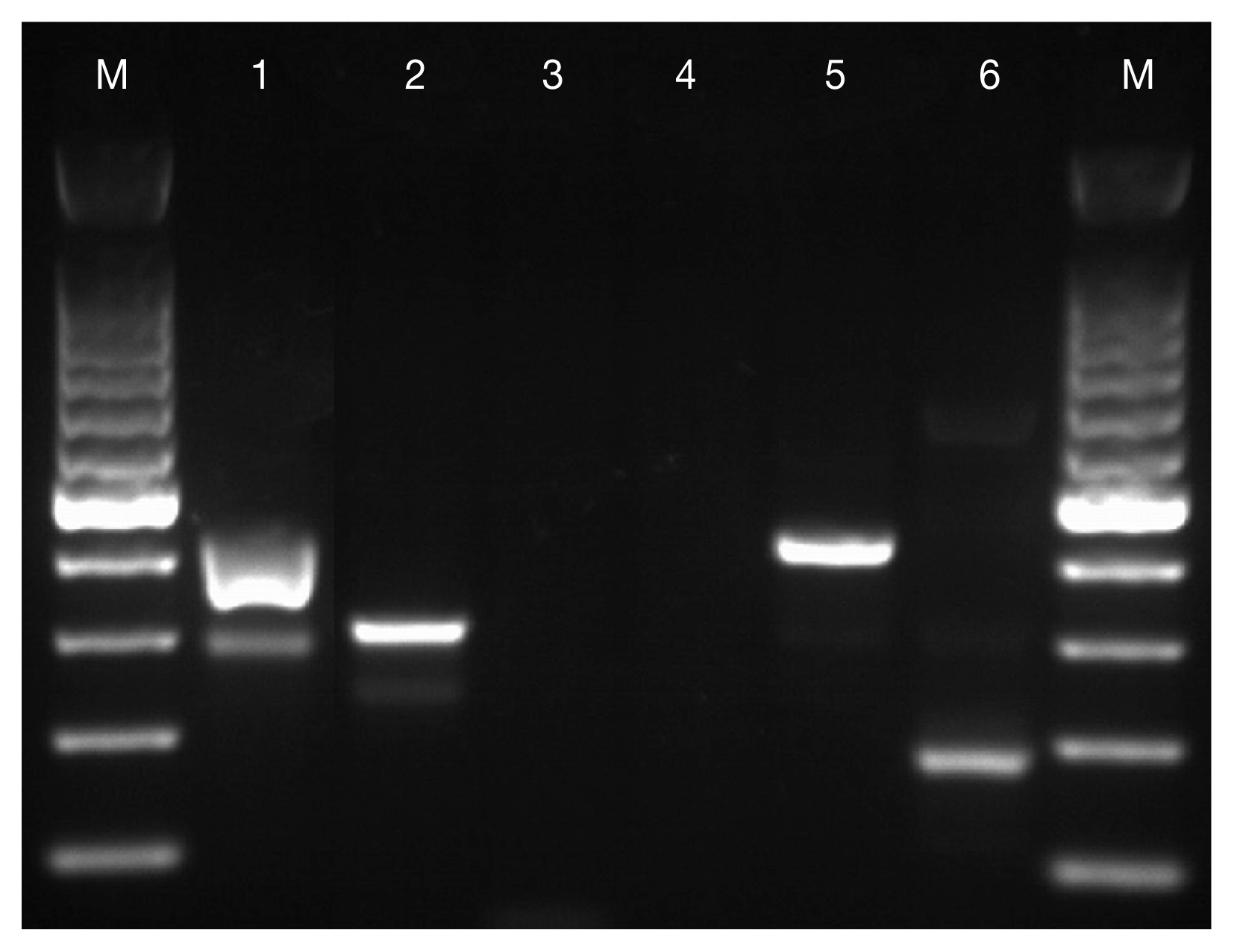
Fig. 1) and positive amplicons were obtained from the PCR for
Naegleria spp. and
N. fowleri with amplification fragment lengths of about 410 bp and 310 bp, respectively (
Fig. 2). His family members recollected that he had been to a water park 5 days (5d) before the onset of symptoms. Then linezolid was discontinued immediately, and regime consisting of intravenous conventional amphotericin B (5 mg initial dose followed by 10 mg on day 2, 25 mg on day 3, and 50 mg/day thereafter) and fluconazole (400 mg/day) was begun immediately. Nevertheless, the result of a repeat CSF study after 5 days target treatment was negative for trophozoites and his vital signs became relatively stable with normal temperature, pulse, and pressure; yet the analysis of Glasgow coma scale (GCS) continually showed 3 points and no spontaneous breathing was detected. Considering the prognosis, the patient was transferred to a local hospital in Shenzhen on 30 August, he died on 3 September.
DISCUSSION
Since the first case of PAM was described by Fowler and Carter in Australia in 1965 [
3], there have been nearly 200 cases reported hitherto, including 7 cases from China. Although
N. fowleri is distributed worldwide, interestingly, a majority of the reported cases are from the USA with a total number of 138 cases until 2015 [
4].
N. fowleri commonly occurs in warm freshwater; thus, any freshwater-related activities such as swimming or diving could bring the water into the nose, resulting in PAM. However, the incidence of PAM is extremely low, which indicates that exposure rarely leads to infection. Nonetheless, factors related to the occurrence of PAM are yet unknown, raising several concerns about the prevention and detection of the infections. Some theories suggest avoiding the freshwater-related activities, especially jumping into the body of water, splashing, or submerging their heads under the water during the summer season when the water temperature is high. If such activities cannot be avoided, individuals should use nose clips during the activities or rinse the nose and nasal passages with clean water immediately after such activities [
5].
The fatality of PAM is extremly high with only 7 survivors to date [
5]. This might be attributed to the following 2 reasons: Firstly, PAM is underdiagnosed since clinical symptoms are similar to those of other more commonly known types of meningitis [
6]. Similar to this case, headache, fever, nausea, and vomiting are common clinical manifestations. The diagnosis of PAM is primarily based on the presence of trophozoites in the CSF that can be detected by trichrome or Giemsa stain. The time spent on diagnosis often results in delayed treatment. Most patients progress rapidly into a deep coma with significantly high intracranial pressure and CSF pressure before diagnosis, which can lead to death [
7]. Secondly, there are no relevant clinical studies that have assessed the efficacy of a specific treatment option [
5]. All the treatment methods, including the recommendation from The Centers for Disease Control and Prevention (CDC), are either based on case reports or in vitro studies. Presently, amphotericin B is accepted as the first choice drug for PAM. The
N. fowleri is highly sensitive to amphotericin B in vitro [
8], and all survivors from North America were reported to have received this medication [
6,
9,
10]. In this case, the result of a repeat CSF study became negative for trophozoites after 5 days target treatment. The recommended therapy of CDC comprises of conventional amphotericin B administered intravenously at the dosages of 1.5 mg/kg/day in 2 doses for 3 day, followed by 1 mg/kg/day for an additional 11 day. The intrathecal administration of conventional amphotericin B (1.5 mg/day for 2 day and 1 mg/day for an additional 8 day) can also be used in combination with intravenous amphotericin B [
11]. Other medications that could be potentially effective include fluconazole, miconazole, miltefosine, azithromycin, and rifampin, which are usually used in combination with conventional amphotericin B [
5].
Although this fatal disease might be cured if treated early and effectively, most clinicians might have never encountered it before. Therefore, it is imperative for clinicians to have an awareness of the possibility of PAM in every case of purulent meningitis, especially in patients with recent freshwater exposure during the hot season.
ACKNOWLEDGMENT
This study was financially funded by the General Project Funds from the Health Department of Zhejiang Province. Grant No. 2015KYA018.
Fig. 1Wright-Giemsa staining of CSF shows trophozoites (arrow) of N. fowleri.

Fig. 2PCR products revealed by agarose gel electrophoresis. M: 100-bp marker; lanes 1–6: amplified with primers of Naegleria spp., N. fowleri, Entamoeba histolytica, Entamoeba dispar, Vahlkampfia spp., and Acanthamoeba spp., respectively.

References
- 1. De Jonckheere JF. Origin and evolution of the worldwide distributed pathogenic amoeboflagellate Naegleria fowleri. Infect Genet Evol 2011;11:1520-1528.
- 2. Jarolim KL, McCosh JK, Howard MJ, John DT. A light microscopy study of the migration of Naegleria fowleri from the nasal submucosa to the central nervous system during the early stage of primary amebic meningoencephalitis in mice. J Parasitol 2000;86:50-55.
- 3. Fowler M, Carter RF. Acute pyogenic meningitis probably due to Acanthamoeba sp.: a preliminary report. Br Med J 1965;2:740-742.
- 4. Cope JR, Ali IK. Primary amebic meningoencephalitis: what have we learned in the last 5 years? Curr Infect Dis Rep 2016;18:31-37.
- 5. Grace E, Asbill S, Virga K. Naegleria fowleri: Pathogenesis, Diagnosis, and Treatment Options. Antimicrob Agents Chemother 2015;59:6677-6681.
- 6. Capewell LG, Harris AM, Yoder JS, Cope JR, Eddy BA, Roy SL, Visvesvara GS, Fox LM, Beach MJ. Diagnosis, clinical course, and treatment of primary amoebic meningoencephalitis in the United States, 1937–2013. J Pediatric Infect Dis Soc 2015;4:68-75.
- 7. Visvesvara GS, Moura H, Schuster FL. Pathogenic and opportunistic free-living amoebae: Acanthamoeba spp., Balamuthia mandrillaris, Naegleria fowleri, and Sappinia diploidea. FEMS Immunol Med Microbiol 2007;50:1-26.
- 8. Carter RF. Sensitivity to amphotericin B of a Naegleria sp. related from a case of primary amoebic encephalitis. J Clin Pathol 1969;22:470-474.
- 9. Seidel JS, Harmatz P, Visvesvara GS, Cohen A, Edwards J, Turner J. Successful treatment of primary amebic meningoencephalitis. N Engl J Med 1982;306:346-348.
- 10. Vargas-Zepeda J, Gómez-Alcalá AV, Vásquez-Morales JA, Licea-Amaya L, De Jonckheere JF, Lares-Villa F. Successful treatment of Naegleria fowleri meningoencephalitis by using intravenous amphotericin B, fluconazole and rifampicin. Arch Med Res 2005;36:83-86.
- 11. Centers for Disease Control and Prevention. May. 2014, Atlanta, USA. N. fowleri treatment. Centers for Disease Control and Prevention.
Citations
Citations to this article as recorded by

- Fatal Primary Amoebic Meningoencephalitis in Coastal Areas of North China in an Immunocompetent Patient: A Case Report and Literature Review
Qian Li Wang, Sheng Nan Teng, Xiao Jing Zhang, Yu Xin Guo, Yang Kong, Xing Han Tian, Yi Zhang
Infection and Drug Resistance.2026; Volume 19: 1. CrossRef - Enlightening the promising role of nanoparticle-based treatments against Naegleria fowleri-induced primary amoebic meningoencephalitis: A brain-eating disease
Sunita Jhulki, Biplab Bhowmik, Aparajita Pal
Microbial Pathogenesis.2025; 199: 107234. CrossRef - Naegleria fowleri Infections: Bridging Clinical Observations and Epidemiological Insights
Carmen Rîpă, Roxana Gabriela Cobzaru, Miruna Raluca Rîpă, Alexandra Maștaleru, Andra Oancea, Carmen Marinela Cumpăt, Maria Magdalena Leon
Journal of Clinical Medicine.2025; 14(2): 526. CrossRef - Naegleria fowleri: An Amoeba That Eats your Brain
Siddhi Suhas Shinde, Anuradha Prajapati, Sachin B. Narkhede, Shailesh Luhar
Research Journal of Pharmaceutical Dosage Forms and Technology.2025; : 37. CrossRef - Amoebicidal effect of chlorine dioxide gas against pathogenic Naegleria fowleri and Acanthamoeba polyphaga
Hae-Jin Sohn, A-Young Park, Jeong-Heon Lee, Kyu-Hwa Yun, Kyoung-Ju Song, Jong-Hyun Kim, Ho-Joon Shin
Parasitology Research.2024;[Epub] CrossRef - A scoping review on epidemiology and pathogenesis of death due to primary amoebic meningoencephalitis
Krishneswari Rajasekharan Nair Saraswathy
International Journal Of Community Medicine And Public Health.2024; 12(1): 598. CrossRef - Systematic Review of Brain-Eating Amoeba: A Decade Update
Mohd ‘Ammar Ihsan Ahmad Zamzuri, Farah Nabila Abd Majid, Massitah Mihat, Siti Salwa Ibrahim, Muhammad Ismail, Suriyati Abd Aziz, Zuraida Mohamed, Lokman Rejali, Hazlina Yahaya, Zulhizzam Abdullah, Mohd Rohaizat Hassan, Rahmat Dapari, Abd Majid Mohd Isa
International Journal of Environmental Research and Public Health.2023; 20(4): 3021. CrossRef - Distribution and Current State of Molecular Genetic Characterization in Pathogenic Free-Living Amoebae
Alejandro Otero-Ruiz, Leobardo Daniel Gonzalez-Zuñiga, Libia Zulema Rodriguez-Anaya, Luis Fernando Lares-Jiménez, Jose Reyes Gonzalez-Galaviz, Fernando Lares-Villa
Pathogens.2022; 11(10): 1199. CrossRef - Photolysis of sodium chloride and sodium hypochlorite by ultraviolet light inactivates the trophozoites and cysts of Acanthamoeba castellanii in the water matrix
Beni J. M. Chaúque, Marilise B. Rott
Journal of Water and Health.2021; 19(1): 190. CrossRef - Drugs used for the treatment of cerebral and disseminated infections caused by free‐living amoebae
Alexandre Taravaud, Zineb Fechtali‐Moute, Philippe M. Loiseau, Sébastien Pomel
Clinical and Translational Science.2021; 14(3): 791. CrossRef - Death From Primary Amebic Meningoencephalitis After Recreational Water Exposure During Recent Travel to India—Santa Clara County, California, 2020
Glenn R Harris, Ellora N Karmarkar, Rebecca Quenelle, Lyndsey Chaille, Jai Madhok, Vivian Tien, Jyoti Gupta, Seema Jain, Maria Liu, Shantanu Roy, Supriya Narasimhan, Akiko Kimura, Jennifer R Cope, Ibne Karim M Ali
Open Forum Infectious Diseases.2021;[Epub] CrossRef - Various brain-eating amoebae: the protozoa, the pathogenesis, and the disease
Hongze Zhang, Xunjia Cheng
Frontiers of Medicine.2021; 15(6): 842. CrossRef - Understanding the true burden of “Naegleria fowleri” (Vahlkampfiidae) in patients from Northern states of India: Source tracking and significance
Ashutosh Panda, Bijay Ranjan Mirdha, Neha Rastogi, Samander Kasuhik
European Journal of Protistology.2020; 76: 125726. CrossRef - A Fatal Case of Primary Amoebic Meningoencephalitis (PAM) Complicated with Diabetes Insipidus (DI): A Case Report and Review of the Literature
Muhammad Zain Mushtaq, Saad Bin Zafar Mahmood, Adil Aziz
Case Reports in Infectious Diseases.2020; 2020: 1. CrossRef