Abstract
Dirofilariasis is a common parasitic disease in both domestic and wild animals around the world, with canines as the principal reservoir host and mosquitoes as the vector. Human ophthalmic dirofilariasis is an uncommon condition, but there have been reports from many parts of the world, including Africa, Australia, the Americas, Europe, and Asia. Ophthalmic involvement with Dirofilaria may present itself as periorbital, subconjunctival, orbital, or intraocular infections. In this report, we present a case of orbital dirofilariasis with lateral rectus muscle involvement. To our knowledge, this is the first orbital dirofilariasis case reported in Iran. Although debulking of the tumor usually leads to resolution, our patient showed an episode of recurrence after biopsy. Complete recovery was achieved after a spontaneous discharge, without the need for systemic medication.
-
Key words: Dirofilaria, dirofilariasis, orbit, case report, Iran
INTRODUCTION
Dirofilariasis is a parasitic disease common in both domestic and wild animals around the world. Canines serve as the principal reservoir host of the parasite, and it is transmitted through mosquito bites which may occasionally infect humans as a zoonotic disease. Human ophthalmic dirofilariasis is uncommon, but there have been reports from many parts of the world, including Africa, Australia, the Americas, Europe, and Asia. Ophthalmic involvement with Dirofilaria may present as periorbital, subconjunctival, orbital, or intraocular infections.
In this report, we present a case of orbital dirofilariasis with lateral rectus muscle involvement. To our knowledge, this is the first orbital dirofilariasis case reported in Iran.
CASE REPORT
A 24-year-old lady was referred to our center complaining of a slightly painful mass near the temporal area of the right eye which had been unresponsive to topical steroids and palliative therapy over the last month. In the history of the present illness, there was no incident of trauma or insect bites. The only significant point was a trip to the north of Iran 2 months before initial symptoms. She gave no history of eye or systemic disease, either.
Vision tests were normal in both eyes, and there was no diplopia or limited range of motion. A mass was seen in the temporal region of the right globe. The mass was about 8 × 12 mm in size and was associated with localized conjunctival injection. Other examinations, including fundoscopy, were insignificant. The orbital magnetic resonance image (MRI) was of no significance, either. The complete blood count test was normal without any sign of eosinophilia.
Assuming a diagnosis of orbital inflammatory syndrome, surgical exploration and biopsy was performed. Upon exploration, we found a gray inflamed mass at the lateral rectus muscle insertion site and the adjacent sclera. The tumor was debulked, but since the lateral rectus tendon was involved, we avoided total removal to preserve muscle function.
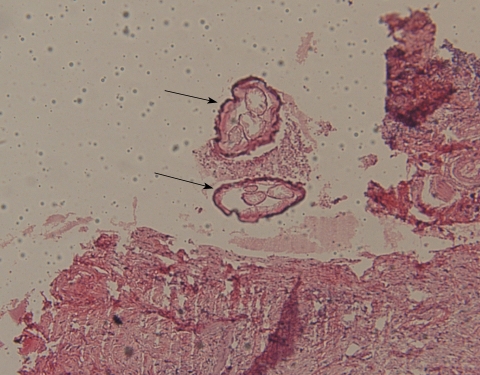
Histological examinations revealed multiple sections of a nematode with central eosinophilic and neutrophilic infiltration surrounded by granulomatous and fibrous tissues (
Fig. 1). Morphologic evaluation showed a nematode with multilayer thick cuticles, indistinct intestinal cells, numerous external ridges, distinct dorsal and ventral fields of divided coelomyarian somatic musculature, 2 internal longitudinal ridges with broad lateral chords, heavy musculature, and didelphic uterine tubes with a small extra branch empty of microflariae. These findings suggested it to be a mature female worm of
Dirofilaria repens (
Fig. 2). Treatment with topical steroids was commenced.
Two weeks after the mass removal and application of topical steroids, the mass recurred at the original site. This second mass ruptured spontaneously after 48 hr, disclosing serous bloody exudates. The consultant parasitologist attributed the recurrence to remaining parasite fragments and an inflammatory response to its antigens. However, all symptoms resolved spontaneously within the next 2 week.
DISCUSSION
Dirofilariasis is a zoonotic infection that may occasionally infect humans. There are about 40 species of Dirofilaria, but only a small number can cause human infections. The most common species in man is Dirofilaria immitis, the common parasite of dogs, Dirofilaria tenuis, a parasite of raccoons, D. repens, a parasite of cats and dogs, and Dirofilaria ursi, which occurs in bears. Humans are accidental and terminal dead-end hosts of Dirofilaria. Microfilariae usually fail to complete maturation, and reproduction occurs rarely. Therefore, pathologic evaluation in humans only demonstrates degenerated immature juvenile worms or adult worms. In response to infection, an inflammatory granulomatous reaction is seen which is associated with infiltration of neutrophils, eosinophils, and foreign body giant cells.
Human dirofilariasis usually presents as the form of pulmonary, subcutaneous, ocular, cardiovascular, or testicular involvement. Ophthalmic dirofilariasis is an uncommon condition, but there have been reports from Africa [
1], Australia [
2,
3], the Americas [
4], Europe [
5], and Asia [
6]. Ophthalmic involvement may present as periorbital [
7], subconjunctival [
6], orbital [
2,
3], or intraocular infections [
5]. Orbital infections may appear as the involvement of the lacrimal glands [
8], the superior rectus and levator palpebralis muscles [
2,
3], or an orbital tumor [
9-
11]. In our case, the lateral rectus muscle tendon was involved.
Dirofilariasis may be associated with eosinophilia. In the present case, however, blood tests were normal. ELISA is a weak test and may not be very helpful because of delayed serocon-version [
3] and of cross reactivity with other helminthic organisms [
12]. Western blot assays yield higher sensitivity by using polypeptide molecular markers, and can therefore be more useful in the detection of human dirofilariasis [
12].
There are few reports on the imaging features of dirofilariasis. In a case of orbital involvement, MRI findings were described as a discrete low intensity tubular signal in the center of the nodule surrounded by contrast-enhancing inflammatory tissues [
10]. In another report, extraconal orbital dirofilariasis was studied with high resolution ultrasound and they found actively motile folded tubular structures with parallel echogenic walls [
11]. In the present case, there were no abnormal findings in the orbital MRI, possibly due to the small size and external location of the mass.
Definite diagnosis requires surgical removal and pathological examination of the specimen. Diagnosis is made through histological and morphological evaluation of the worm. The presence of thick laminated cuticles, large muscle cells, and wide lateral chords is diagnostic for this parasite. Identification of the species depends on macroscopic examination of the mature worm. In cases of deep tissue involvement where only histopathologic specimens are available, studying the size and features of the body wall, i.e., cuticle thickness and structure, ridges, number of lateral chords, and muscle cell type can help the differential diagnosis of the species. An accurate diagnosis can also be made through PCR-based DNA analysis especially when conventional morphologic assessment is not possible due to poor worm conservation [
1,
12].
Surgical removal is not only diagnostic, but also leads to definite cure in most cases. Although human dirofilariasis is thought to be an infection caused by a single worm, when systemic infection is suspected, a single dose of oral ivermectin is recommended. An interesting observation in our case was the recurrence of the mass which ruptured spontaneously and ended in definite cure without application of systemic treatment.
In Iran, human and animal dirofilariasis with
D. immitis and
D. repens has been reported from 11 provinces; the former in east and west Azerbaijan, Ardebil, Tehran, Khorasan, Khoozestan, Fars, Golestan, Mazandaran, and Hormozgan, and
D. repens in Tehran, Khorasan, Gilan, and Mazandaran [
13]. To date, 14 cases of human dirofilariasis have been reported in Iran. These include 1 case of testicular hydrocele, 2 cases of pulmonary involvement [
13,
14], 7 cases of subcutaneous infections [
6,
13,
15,
16], and 4 cases of ocular dirofilariasis which presented as a subconjunctival infection [
6,
13,
17]. There has also been an unreported case of ocular dirofilariasis in Golestan [
13] (personal communication, Mobedi).
Dirofilariasis is considered an emerging zoonotic disease, and the number of human cases has been increasing in recent years [
13]. Therefore, although the present case is the first report of orbital involvement with
Dirofilaria in Iran, it seems necessary to include this infection in the differential diagnosis of orbital inflammations or masses.
References
- 1. Abdel-Rahman SM, Mahmoud AE, Galal LA, Gustinelli A, Pampiglione S. Three new cases of human infection with Dirofilaria repens, one pulmonary and two subcutaneous, in the Egyptian governorate of Assiut. Ann Trop Med Parasitol 2008;102:499-507.
- 2. Stringfellow GJ, Francis IC, Coroneo MT, Walker J. Orbital dirofilariasis. Clin Exp Ophthalmol 2002;30:378-380.
- 3. Angunawela RI, Ataullah S, Whitehead KJ, Sullivan TJ, Rosser P. Dirofilarial infection of the orbit. Orbit 2003;22:41-46.
- 4. Skidmore JP, Dooley PD, DeWitt C. Human extrapulmonary dirofilariasis in Texas. South Med J 2000;93:1009-1010.
- 5. Gorezis S, Psilla M, Asproudis I, Peschos D, Papadopoulou C, Stefaniotou M. Intravitreal dirofilariasis: a rare ocular infection. Orbit 2006;25:57-59.
- 6. Maraghi S, Rahdar M, Akbari H, Radmanesh M, Saberi A. Human dirofilariasis due to Dirofilaria repens in Ahvaz-Iran: a report of three cases. Pak J Med Sci 2006;22:211-213.
- 7. Kersten RC, Locastro AJ, Eberhard ML, Spaulding AG, Kulwin DR. Periorbital dirofilariasis. Ophthal Plast Reconstr Surg 1994;10:293-296.
- 8. Yuen KS, Tse MW, Choi PC, Chan WM, Lam DS. Unusual presentation of dirofilariasis as a lacrimal mass. Eye 2004;18:959-960.
- 9. Braun H, Koele W, Stammberger H, Ranner G, Gröll R. Endoscopic removal of an intraorbital "tumor": a vital surprise. Am J Rhinol 1999;13:469-472.
- 10. Groell R, Ranner G, Uggowitzer MM, Braun H. Orbital dirofilariasis: MR findings. AJNR Am J Neuroradiol 1999;20:285-286.
- 11. Smitha M, Rajendran VR, Devarajan E, Anitha PM. Case report: Orbital dirofilariasis. Indian J Radiol Imaging 2008;18:60-62.
- 12. Cancrini G, Prieto G, Favia G, Giannetto S, Tringali R, Pietrobelli M, Simón F. Serological assays on eight cases of human dirofilariasis identified by morphology and DNA diagnostics. Ann Trop Med Parasitol 1999;93:147-152.
- 13. Azari-Hamidian S, Yaghoobi-Ershadi MR, Javadian E, Mobedi I, Abai MR. Review of dirofilariasis in Iran. J Med Facul Guilan Univ Med Sci 2006;15:102-113.
- 14. Rokni MB. The present status of human helminthic diseases in Iran. Ann Trop Med Parasitol 2008;102:283-295.
- 15. Negahban S, Daneshbod Y, Atefi S, Daneshbod K, Sadjjadi SM, Hosseini SV, Bedayat GR, Abidi H. Dirofilaria repens diagnosed by the presence of microfilariae in fine needle aspirates: a case report. Acta Cytol 2007;51:567-570.
- 16. Radmanesh M, Saberi A, Maraghi S, Emad-Mostowfi N, Radmanesh M. Dirofilaria repens: a dog parasite presenting as a paranasal subcutaneous nodule. Int J Dermatol 2006;45:477-478.
- 17. Jamshidi A, Jamshidi M, Mobedi I, Khosroara M. Periocular dirofilariasis in a young woman: a case report. Korean J Parasitol 2008;46:265-267.
Fig. 1Microscopic view of 2 cross sections (arrows) of the nematode which is surrounded by necrotizing granulomatous and eosinophilic inflammation. ×40.

Fig. 2Microscopic view of the nematode showing diagnostic features, including lateral chords and a multilayered cuticle. ×100.