Abstract
Visceral leishmaniasis or kala-azar is an endemic parasitic disease in some parts of the world which is characterized by fever, splenomegaly, and pancytopenia in most of the cases. Herein we report an 11 month-old male infant with diagnosis of kala-azar who presented with pallor, hepatosplenomegaly, failure to gain weight, and no history of fever. Surprisingly, fever started after beginning of meglumine antimoniate treatment in this patient. As far as we are aware of, this is a rare presentation of visceral leishmaniasis. Therefore, clinicians especially in endemic areas are highly recommended to include kala-azar among differential diagnosis of unexplained anemia without fever to prevent misdiagnosis of this potentially fatal, but treatable condition.
-
Key words: Leishmania infantum, afebrile, anemia, kala-azar, splenomegaly, visceral leishmaniasis
INTRODUCTION
Visceral leishmaniasis (VL) or kala-azar is an endemic parasitic disease in some parts of Iran which is caused predominantly by
Leishmania infantum [
1,
2,
3]. Fever and splenomegaly are detected in more than 80% of patients as the most common clinical manifestations. Neutropenia, anemia, thrombocytopenia, elevated ESR, and hypergammaglobulinemia are the most common laboratory abnormalities of this disease [
4]. Herein we report a rare case of kala-azar in a pediatric age group without fever.
CASE RECORD
An 11-month-old male was referred to Ali Asghar Children Hospital following pallor and illness for 5 months. Prior to admission in our hospital, he had received packed cell 4 times and underwent bone marrow aspiration 2 times in 2 previous admissions with no definite diagnosis. He had no history of fever, icterus, bleeding tendency, and gastrointestinal or respiratory symptoms; however, irritability, anorexia, and failure to gain weight were reported by his care givers during this time.
On physical examination his vital signs were within normal range. He had hepatosplenomegaly without lymphadenopathy and rash. The span of spleen and liver measured by ultrasound examination were 122 mm×38 mm and 78 mm, respectively. His primary laboratory data was as follows: WBC 10.6×103/mm3 (normal range:6.0-13.5×103/mm3), neutrophils 21%, lymphocytes 78%, eosinophils 1%, hemoglobin (Hb) 6.4 g/dl (normal range: 11-13 g/dl), platelet 138,000/mm3 (normal range: 140,000-440,000), ESR 82 mm/hr (normal:<15 mm/hr), qualitative CRP 2+, reticulocyte count 2%, LDH 7,03I U/L (normal: up to 480). Serum albumin, total protein, and routine liver and kidney function test results were within normal limits. HIV test and direct coombs were also negative.
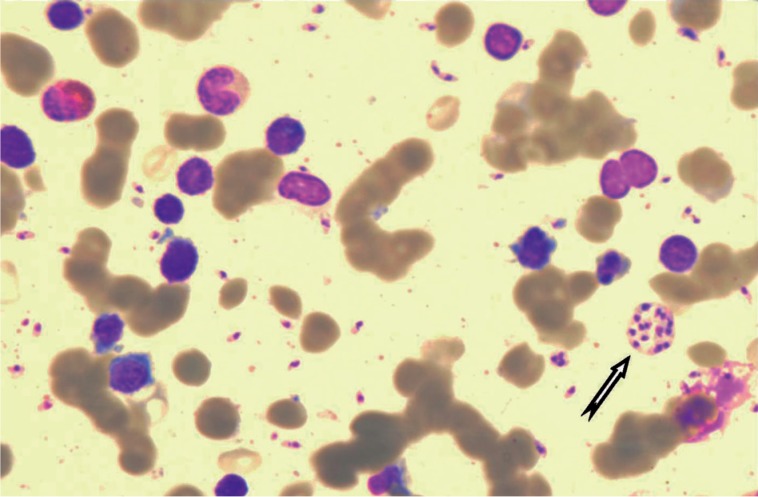
Examination of bone marrow aspirate revealed a large number (grade 5+) [
5] of
Leishmania sp. under a light microscope with high magnification (
Fig. 1). The parasite load in the bone marrow smears before, in the middle, end of the treatment, and relapse time was graded based on World Health Organization guidance [
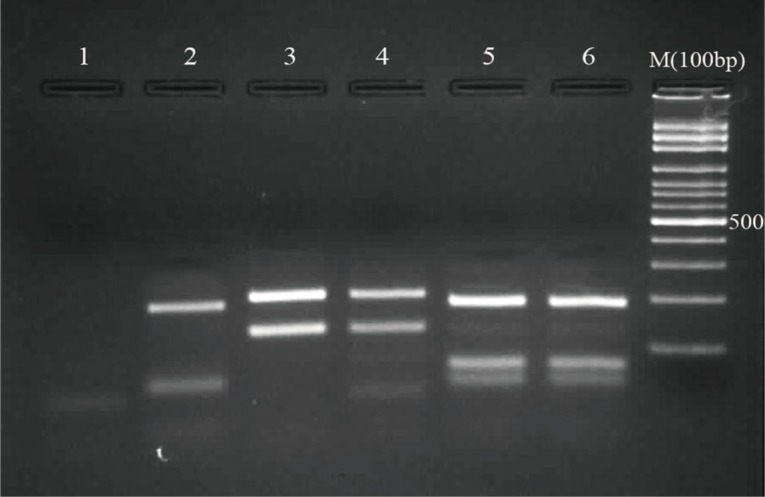
5]. DNA from the slides was extracted and subjected to PCR-reverse fragment length polymorphism (RFLP) assay. The ribosomal internal transcribed spacer 1 (ITS1) was amplified with specific primers, and the PCR products were digested with a restriction enzyme (
HaeIII).
The species of parasite documented by PCR-RFLP assay was
L. infantum (
Fig. 2). Rapid kala-azar K39 immunochromatographic dipstick serological test for
L. infantum infection was also positive. Specific anti-leishmanial antibodies detected by indirect fluorescent antibody test (IFAT) and direct agglutination test (DAT) were at titers of 1:320 and 1:3,200, respectively. Work-up for immunodeficiency disorders performed by flow cytometry showed no abnormal findings. Two days after starting treatment with meglumine antimoniate (Glucantime®), at a dose of 20 mg/kg, the patient became febrile and fever persisted despite continuing Glucantime® for 9 days.
We switched our treatment to amphotericin B deoxycolate (1 mg/kg/day), and fever was stopped 48 hr after starting this drug. He received amphotericin B for a period of 28 days. The results of bone marrow aspiration in the middle of this time showed decreasing load of Leishman bodies (grade 2+) [
5] and was negative at the end of the treatment.
Three months after discharge, he became pale and febrile again, and his liver and spleen were found to become enlarged on monthly examinations. He underwent bone marrow aspiration and was admitted with positive bone marrow aspirate for leishman bodies (grade 4+) [
5]. He was leukopenic (WBC 2,500/mm
3, neutrophils 37%, lymphocytes 61%, monocytes 1%, eosionophils 1%), anemic (Hb 7.6 mg/dl) and thrombocytopenic (platelet 79,000/mm
3). ESR was 108 mm/hr.
His treatment was started with liposomal amphotericin B (Ambisome®) 4 mg/kg on days 1-5 and at the 14th and 21th day in combination with daily subcutaneous human recombinant interferon-γ at the dose of 100 µg/m2 plus oral allopurinol at the dose of 20 mg/kg/day in 3 divided doses. He was discharged 24 hr after becoming afebrile on the 5th day of receiving Ambisome®. He received the rest of the treatment in outpatient manner. Six months follow-up showed no relapse or complications.
DISCUSSION
Visceral leishmaniasis is known as an endemic disease in some parts of the world including Iran [
1,
2,
3]. The most common clinical findings are fever, splenomegaly, and anemia. Hepatomegaly is less frequent than splenomegaly, and features such as jaundice, edema, and ascites are less frequently reported [
3]. Signs and symptoms of VL in Iran are compatible with the Mediterranean type except for the absence of significant lymphadenopathy [
3]. Fever with maximum rate of 100% is the most common symptom but may be absent in immunocompromised patients, subclinical forms especially in endemic areas, and rarely immunocompetent ones [
4].
Our patient was afebrile at presentation despite no documented immunodeficiency, and his bone marrow aspirate showed a large number of leishman bodies. It seems that high parasite load might suppress the inflammatory response in body and prevent fever, the phenomenon which could be noted in other diseases such as tuberculosis and lepromatous leprosy [
4]. It might also address the normal leukocyte count and serum albumin/total protein ratio in our case. The patient became febrile 2 days after starting treatment, and this might be due to massive release of antigens after starting therapy with a subsequent triggering of an immune response. Subsiding fever in kala-azar is usually considered as a clinical response to the treatment. Our patient did not have fever at the beginning of the treatment but fever was started after Glucantime® treatment. We had no rapid clinical marker for response to the treatment and were compelled to discontinue Glucantime® after 9th day of fever. It was according to some documented evidence of resistance to Glucantime® against
L. infantum and
L. tropica in our area [
6,
7,
8,
9].
We switched our treatment to amphotericin B deoxycolate and continued it for 30 days. Amphotericin B deoxycolate is usually used at a dose of 0.75-1.0 mg/kg/IV/daily for 15-20 doses for VL caused by
L. donovani and up to 30 days for VL caused by
L. infantum [
10]. Three months after the end of treatment, the patient experienced an episode of relapse. Relapse could occur in kala-azar despite proper treatment and efficient immune state [
11]. In general, diseases caused by intracellular microorganisms might recur secondary to residual organisms escaped pharmacologically and/or immunologically [
11]. Heavy leishman body load at that first bone marrow aspiration might be a risk factor in our patient for relapse.
According to its high concentration in reticuloendothelial system, we decided to use Ambisome® and added human recombinant interferon-γ and allopurinol as adjuvant therapies to increase the eradication rate. The indication of using interferon-γ and allopurinol in combination with liposomal amphotericin B in patients with relapse but no documented immunosuppressant state or resistance to antimonials is poorly defined. Different regimens of Ambisome® have been recommended for treatment of kala-azar [
12,
13,
14]. The regimen which is usually administered in immunocompetent pediatric patients was scheduled for our patient [
14,
15].
In conclusion, medical practitioners especially in endemic areas should be aware of and consider VL among differential diagnosis of afebrile unexplained anemia.
Notes
-
We declare that we have no conflict of interest related to this study.
References
- 1. Mohebali M. Visceral leishmaniasis in Iran: review of the epidemiological and clinical features. Iran J Parasitol 2013;8:348-358.
- 2. Mohebali M, Edrissian GH, Shirzadi MR, Hosseingholizadeh G, Pashaei MH, Ganji A, Zarei Z, Kousha A, Akhoundi B, Hajjaran H, Malekafzalli H. Integrated visceral leishmaniasis surveillance system in primary care for children in Meshkin-Shahr district, north-western Islamic Republic of Iran. East Mediterr Health J 2010;16:1050-1054.
- 3. Alborzi A, Pouladfar GR, Aelami MH. Visceral leishmaniasis; literature review and iranian experience. Iran J Clin Infect Dis 2007;2:99-108.
- 4. Mohan A, Reddy EV, Samantaray JC, Sharma SK. A rare presentation of visceral leishmaniasis without fever or splenomegaly in an elderly person. Eur J Intern Med 2007;18:158-160.
- 5. World Health Organization. Basic Laboratory Methods in Medical Parasitology. 1991. cited 2013, Nov 18. http://www.who.int/malaria/publications/atoz/9241544104_part1/en/index.htm
- 6. Hadighi R, Mohebali M, Boucher P, Hajjaran H, Khamesipour A, Ouellette M. Unresponsiveness to glucantime treatment in Iranian cutaneous leishmaniasis due to drug-resistant Leishmania tropica parasites. PLoS Medicine 2006;3:e162.
- 7. Kazemi-Rad E, Mohebali M, Khadem-Erfan MB, Saffari M, Raoofian R, Hajjaran H, Hadighi R, Khamesipour A, Rezaie S, Abedkhojasteh H, Heidari M. Identification of antimony resistance markers in Leishmania tropica field isolates through a cDNA-AFLP approach. Exp Parasitol 2013;135:344-349.
- 8. Kazemi-Rad E, Mohebali M, Khadem-Erfan MB, Hajjaran H, Hadighi R, Khamesipour A, Rezaie S, Saffari M, Raoofian R, Heidari M. Over expression of ubiquitin and amino acid permease genes in association with antimony resistance in Leishmania tropica field isolates. Korean J Parasitol 2013;51:413-419.
- 9. Bagher Khadem Erfan M, Mohebali M, Kazemi-Rad E, Hajjaran H, Edrissian G, Mamishi S, Saffari M, Raoofian R, Heidari M. Down regulation of calcineurin gene is associated with Glucantime® resistance in Leishmania infantum. Iran J Parasitol 2013;8:359-366.
- 10. McGwire BS, Satoskar AR. Leishmaniasis: clinical syndromes and treatment. QJM 2013;107:7-14. doi: 10.1093/qjmed/hct116
- 11. Murray HW. Treatment of visceral leishmaniasis (kala-azar): a decade of progress and future approaches. Int J Infect Dis 2000;4:158-177.
- 12. Thakur CP. A single high dose treatment of kala-azar with ambisome (amphotericin B lipid complex): a pilot study. Int J Antimicrob Agents 2001;17:67-70.
- 13. Griensven JV, Balasegaram M, Meheus F, Alvar J, Lynen L, Boelaert M. Combination therapy for visceral leishmaniasis. Lancet Infect Dis 2010;10:184-194.
- 14. Tunccan OG, Tufan A, Telli G, Akyürek N, Pamukçuoğlu M, Yılmaz G, Hızel K. Visceral leishmaniasis mimicking autoimmune hepatitis, primary biliary cirrhosis, and systemic lupus erythematosus overlap. Korean J Parasitol 2012;50:133-136.
- 15. Garcia LS, Nielsen-Saines K. Leishmaniasis. In Feigin RD, Cherry JD, Demmler-Harrison GJ, Kaplan SL eds, Feigin and Cherry's Textbook of Pediatric Infectious Diseases. Philadelphia, USA. Saunders; 2009, pp 2920-2930.
Fig. 1Bone marrow aspiration slide (Giemsa stain) showing Leishmania infantum bodies (arrow).

Fig. 2Restriction fragment length polymorphism (RFLP) patterns obtained from Leishmania stocks and patient's sample. Lane 1, negative control; Lane 2, L. tropica; Lanes 3, 4, L. major; Lane 5, L. infantum; Lane 6, PCR product from patient's sample, L. infantum. M, 100-bp size marker (Fermentas).

Citations
Citations to this article as recorded by

- Leishmaniasis – Still a diagnostic challenge: An individual participant data systematic review
Azza Sarfraz, Zouina Sarfraz, Maryyam Liaqat, Muhammad Hadi Khan, Hafiza Aqsa Abdul Jabbar, Muhammad Abdullah
Tropical Doctor.2024; 54(4): 352. CrossRef - Visceral Leishmaniasis After Kidney Transplant: An Unusual Presentation and Mode of Diagnosis
Abhyudaysingh Rana, Ashwini Gadde, Lipika Lippi, Shyam B. Bansal
Experimental and Clinical Transplantation.2022; 20(3): 311. CrossRef - Filariasis presenting as pancytopenia in a child
Anusree Krishna Mandal, Jadab Kumar Jana, Soumya Gayen, Abhay Charan Pal
BMJ Case Reports.2022; 15(5): e248930. CrossRef - A case of visceral leishmaniasis found by left oblique hernia: A case report
Guoqiang Zhang, Jihua Zhong, Ting Wang, Lu Zhong
Experimental and Therapeutic Medicine.2020;[Epub] CrossRef - T cell suppression in the bone marrow of visceral leishmaniasis patients: impact of parasite load
P Kumar, P Misra, C P Thakur, A Saurabh, N Rishi, D K Mitra
Clinical and Experimental Immunology.2018; 191(3): 318. CrossRef - Diversity and incrimination of sandflies (Psychodidae: Phlebotominae) captured in city and suburbs of Hamadan, Hamadan province, west of Iran
Aref Salehzadeh, Somayeh Rafatbakhsh Iran, Milad Latifi, Motahare Mirhoseini
Asian Pacific Journal of Tropical Medicine.2014; 7: S177. CrossRef