Abstract
We report here a human case probably mixed-infected with Clonorchis sinensis and Fasciola sp. who was diagnosed by computed tomography (CT) scan, serological findings, and/or fecal examination. The patient was a 43-year-old Korean female and was admitted to Kyung Hee University Hospital with the complaints of fever and abdominal pain. On admission, marked eosinophilia was noted in her peripheral blood. CT scan showed specific lesions for clonorchiasis and fascioliasis in the liver, along with lesions suggestive of amebic abscess. Micro-ELISA revealed positive results for the 2 helminthic infections. Eggs of C. sinensis and trophozoites of Entamoeba histolytica were observed in the stool. Treatment with praziquantel followed by metronidazole and tinidazole reduced abnormalities in the liver and eosinophilia. This is the first case report of a possible co-infection with 2 kinds of liver flukes in the Republic of Korea.
-
Key words: Clonorchis sinensis, Fasciola sp., Entamoeba histolytica, co-infection, computed tomography
INTRODUCTION
Hepatobiliary parasitic infections caused by liver flukes are important public health problems in East Asia, East Europe, Africa, and Latin America. Currently, more than 780 million people are exposed to infection with these flukes [
1]. Among the liver flukes,
Fasciola sp. is a parasite of ruminants distributed worldwide. It normally infects the liver of cattle, sheep, or goats and causes a disease called 'liver-rot'. Human fascioliasis is caused accidentally by drinking water or ingestion of raw aquatic vegetables contaminated with metacercariae [
2].
Clonorchis sinensis, the Chinese liver fluke, is a common hepatobiliary parasitic disease in the Far East [
3]. Humans are infected with
C. sinensis by ingestion of raw or undercooked freshwater fish. Human infections with another species of the liver fluke,
Opisthorchis viverrini, similar in morphology and genetics to
C. sinensis, are endemic in South-East Asia [
4]. Infections with the latter 2 flukes are considered important causes of pyogenic cholangitis and cholangiocarcinoma in endemic areas.
Identification of eggs in the feces or bile can lead to a definitive diagnosis of the liver fluke infections. Serodiagnosis using ELISA also shows moderate sensitivity and specificity, but cross reactions with other parasitic infections may occur [
5]. At present, imaging diagnosis using computed tomography (CT) scan, magnetic resonance (MR), or ultrasonography (US) of the abdomen is widely used for hepatobiliary parasitic infections owing to the remarkable advances in medical imaging technology over the past decades [
6,
7]. Currently, CT scan is highly useful for obtaining a clear-cut diagnosis of the liver fluke infections and even for distinguishing the disease from other causes. We report here CT scan diagnosis combined with serological diagnosis of a probable mixed-infection case with
Fasciola sp. and
C. sinensis.
CASE REPORT
A 43 year-old Korean female suffering with fever, chill, and flank pain in the upper and lower quadrants of the abdomen admitted to a local hospital. The patient was treated primarily under an impression of acute pyelonephritis, but the symptoms did not improve. Descriptions on abdominal CT scan images taken at a local hospital revealed liver abscess and cecal wall thickening. The patient was then transferred to Kyung Hee University Hospital.
The patient complained of fever without chill, epigastric discomfort, anorexia, diarrhea, and sometimes nausea and vomiting (
Table 1). The abdomen of the patient was soft and flat, and the bowel sound was increased. There was right costovertebral angle (CVA) tenderness. Alkaline phosphatase, GOT, GPT, γ-GT, and glucose levels of the patient were all above normal limits. The hepatitis B virus surface (HBs) antigen was negative, but the HBs antibody was positive. Colonoscopy showed mild internal hemorrhoids. Blood tests showed marked eosinophilia up to 66% during the examinations. The past medical history of the patient was unremarkable except for an operation of a right ureter stone basket removal 7 years previously.
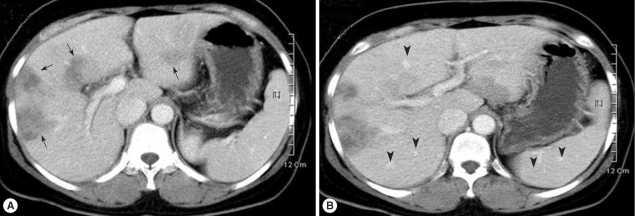
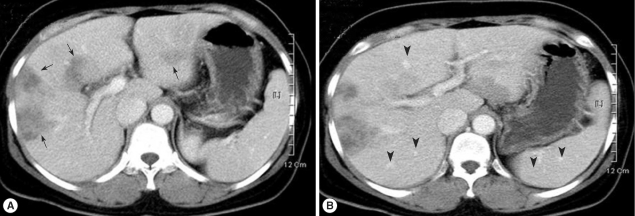
Contrast-enhanced abdominal CT scan revealed duodenal diverticulum and ascites in the pelvic cavity (data not shown) and most importantly, multiple hypodense inflammatory lesions with irregular margins and amorphous shapes in the right lobe of the liver (
Fig. 1). Mild but diffuse dilatations of intrahepatic bile ducts were also observed. Considering the morphology and size of the lesions, the patient was suspected to be mixed-infected with
Fasciola sp. and
C. sinensis. Abscess suspected to be formed by an amebic infection was also observed at the lower tip of the liver (data not shown). Serological tests by micro-ELISA were positive for cysticercosis, clonorchiasis, and fascioliasis (
Table 1). Eggs of
C. sinensis and trophozoites of
E. histolytica were found in stool examinations.
The patient was treated with praziquantel 1,200 mg 3 times a day (total 3,600 mg), and eosinophilia was reduced to < 24%. After the praziquantel treatment, she still complained of nausea, vomiting, and diarrhea. The right flank pain and right lower quadrant tenderness still remained. She was recommended to take metronidazole or tinidazole for a week to treat amebiasis. After the treatment, the CT scan showed improvement of the hepatic lesions and pleural effusion (data not shown). The patient was then discharged with good conditions.
DISCUSSION
The present case reports CT scan diagnosis combined with serological test on hepatobiliary parasitic infections with marked eosinophilia. Since eosinophilia may be regarded as an adaptive response to damage the parasites [
8,
9], it seems to be the most frequent laboratory abnormality in acute infections with hepatobiliary parasites, in particular, fascioliasis. In our case,
C. sinensis infection was confirmed by CT findings, ELISA results, and detecting eggs in the feces.
Fasciola sp. infection was suggested strongly by CT findings and ELISA results. However, we regret that
Fasciola eggs were not detected in fecal examinations.
Human fascioliasis sometimes occurs due to dietary habits eating raw liver of ruminant animals in Korea [
10]. However, the present patient denied having eaten any suspicious raw animal liver. Eating contaminated vegetables may have caused the infection in this patient. Clonorchiasis is caused by eating raw freshwater fish [
3]. However, it was uncertain whether the patient had a preference of eating raw or undercooked fish. Clonorchiasis is currently the most common helminth infection in Korea. Therefore, when clinical symptoms of suspicious fascioliasis appear in a patient, a possibility of mixed-infection with
C. sinensis can be considered.
Human fascioliasis has 2 types of clinical features and manifestations; biliary fascioliasis (infecting the bile duct) and ectopic fascioliasis (infecting the abdominal muscle, intestinal wall, eye, or brain). In the biliary tract infection, there are 2 clinical stages with different signs and symptoms. The first is the hepatic (acute and invasive) stage. At this stage, the fluke perforates the liver and begins to migrate through the liver parenchyma towards the biliary radicles [
11]. Fever, urticaria, pain in the right hypochondrium, hepatomegaly, hypergammaglobulinemia, and marked eosinophilia are common signs and symptoms of this stage. CT imaging may show the migration path as a tunnel-like abscess from the entry site to the parenchyma, and reveal hypodense lesions with irregular margins [
7]. The second is the biliary (chronic) stage. At this stage, the fluke penetrates the wall and enters the lumen of the bile duct. Intermittent right upper quadrant pain with or without cholangitis or cholestasis and sometimes eosinophilia are presented at this stage [
11]. Eosinophilia can also be detected. Ultrasonography, percutaneous cholangiography, or endoscopic retrograde cholangiopancreatography (ERCP) are more helpful than CT or MR for the diagnosis of the biliary stage [
12].
Since abnormal image findings similar to fascioliasis may represent viral hepatitis, malignancy, cholecystitis, cholangitis, and other parasitic infections [
13], differential diagnosis of fascioliasis is important. In the case of clonorchiasis, important CT images include diffuse and uniform dilatation of the peripheral intrahepatic bile ducts with or without minimal dilatation of extrahepatic bile ducts [
6]. No focal obstruction sign is found in clonorchiasis. Although differences in CT images between clonorchiasis and fascioliasis are clear, routine parasitological examinations should be recommended to draw a confirmatory diagnosis.
Unlike the case of C. sinensis or O. viverrini infections, eggs of Fasciola spp. are hardly found by stool examinations even in biliary tract fascioliasis. The eggs are excreted in the feces mostly at the chronic biliary stage, and moreover, the number of egg-producing mature flukes is small, i.e., only a few, in human fascioliasis. In the present case, the eggs of Fasciola sp. were not found, although the eggs of C. sinensis were detected. CT scan of the present patient did not reveal typical images of tunnel-like abscesses as seen in the acute biliary stage of fascioliasis. However, the most probable diagnosis was C. sinensis infection combined with Fasciola sp. infection. Combined parasitic infections may have worsened the hepatic lesions and clinical symptoms of the patient.
Praziquantel is well tolerated and effective against almost all species of trematodes and cestodes [
14], and some successful effects are also known for
Fasciola spp. [
14]. Currently, however, its low efficacy for the treatment of fascioliasis is generally accepted. Triclabendazole, an alternative drug, is currently the most effective agent against fascioliasis and other helminthic infections [
15,
16]. Because of unavailability of triclabendazole, the patient was treated with a relatively high dose of praziquantel, i.e., 3,600 mg within a day. According to a local report, a long-term or a high-dose treatment of praziquantel could reduce eosinophilia and liver abscess caused by fascioliasis [
17]. In our patient, clinical symptoms may have been caused mainly by
C. sinensis and amebic infections; therefore, praziquantel was used as the primary agent, followed by metronidazole and tinidazole. Unfortunately, follow-up examinations were not performed because there was no more contact with the patient after discharge from our hospital. Therefore, recurrence of fascioliasis which is not uncommon in praziquantel-treated patients [
14] could not be confirmed.
References
- 1. Keiser J, Utzinger J. Emerging foodborne trematodiasis. Emerg Infect Dis 2005;11:1507-1514.
- 2. Arjona R, Riancho JA, Aguado JM, Salesa R, González-Macías J. Fascioliasis in developed countries: A review of classic and aberrant forms of the disease. Medicine (Baltimore) 1995;74:13-23.
- 3. Rim HJ. Clonorchiasis: An update. J Helminthol 2005;79:269-281.
- 4. Marcos LA, Terashima A, Gotuzzo E. Update on hepatobiliary flukes: Fascioliasis, opisthorchiasis and clonorchiasis. Curr Opin Infect Dis 2008;21:523-530.
- 5. Choi BI, Han JK, Hong ST, Lee KH. Clonorchiasis and cholangiocarcinoma: Etiologic relationship and imaging diagnosis. Clin Microbiol Rev 204;17:540-552.
- 6. Choi D, Hong ST. Imaging diagnosis of clonorchiasis. Korean J Parasitol 2007;45:77-85.
- 7. Lim JH, Mairiang E, Ahn GH. Biliary parasitic diseases including clonorchiasis, opisthorchiasis and fascioliasis. Abdom Imaging 2008;33:157-165.
- 8. Rothenberg ME. Eosinophilia. N Engl J Med 1998;338:1592-1600.
- 9. Weller PF. Human eosinophils. J Allergy Clin Immunol 1997;100:283-287.
- 10. Paik JW, Choi CS, Choi YK. A case of fascioliasis in the common bile duct. Korean J Gastroenterol 1997;30:553-558.
- 11. Aksoy DY, Kerimoğlu U, Oto A, Ergüven S, Arslan S, Unal S, Batman F, Bayraktar Y. Infection with Fasciola hepatica. Clin Microbiol Infect 2005;11:859-861.
- 12. Gulsen MT, Savas MC, Koruk M, Kadayifci A, Demirci F. Fascioliasis: a report of five cases presenting with common bile duct obstruction. Neth J Med 2006;64:17-19.
- 13. Aksoy DY, Kerimoğlu U, Oto A, Ergüven S, Arslan S, Unal S, Batman F, Bayraktar Y. Fasciola hepatica infection: Clinical and computerized tomographic findings of ten patients. Turk J Gastroenterol 2006;17:40-45.
- 14. Harnett W. The anthelmintic action of praziquantel. Parasitol Today 1988;4:144-146.
- 15. Bacq Y, Besnier JM, Duong TH, Pavie G, Metman EH, Choutet P. Successful treatment of acute fascioliasis with bithionol. Hepatology 1991;14:1066-1069.
- 16. Keiser J, Engels D, Büscher G, Utzinger J. Triclabendazole for the treatment of fascioliasis and paragonimiasis. Expert Opin Investig Drugs 2005;14:1513-1526.
- 17. Kim CG, Kim SM, Lee HS, Chai JY, Kim CY. Clinical response to 7-day praziquantel therapy in Fasciola liver abscess. Korean J Infect Dis 1997;29:417-421.
Fig. 1Abdominal CT scan of the patient. (A) Contrast enhancement using iodine dye revealed multiple inflammatory lesions (arrows). (B) Dilatations of intrahepatic bile ducts (arrow heads) are seen in the liver parenchyme.
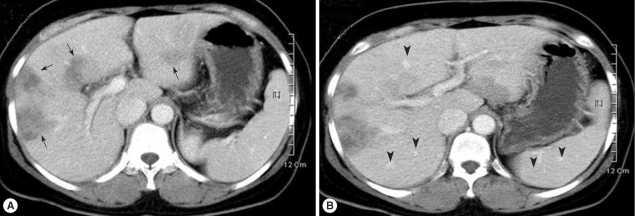
Table 1.Summary of the present case of Clonorchis sinensis and Fasciola sp. co-infection
Table 1.
|
Clinical symptoms |
Notes in laboratory examinations |
Stool examinations
|
ELISA positive |
CT findings |
Medica-tion |
Resolution
|
|
1st |
2nd |
Eggs |
CT |
|
Fever, chill, RUQ & RLQ pain, CVA pain, epigastric discomfort, anorexia, diarrhea, nausea, vomiting |
Eosinophils 46% - 66% |
Cs |
Cs |
Cy |
Duodenal diverticulum, ascites in the pelvic cavity, hypodense inflammatory lesions in liver, dilatations of intrahepatic bile ducts, amebic abscess in the lower tip of liver |
praziquantel metronidazole tinidazole |
ND |
Improved |
|
HBs antigen (-) |
Eh |
Cs |
|
HBs antibody (+) |
Fh |