Abstract
Ascaris lumbricoides causes one of the most common soil-transmitted helminthiases globally. The worms mostly infect the human small intestine and elicit negligible or non-specific symptoms, but there are reports of extraintestinal ectopic ascariasis. We describe a rare case of biliary ascariasis mistaken for biliary stent in a 72-year-old female patient with a history of liver resection. She visited our outpatient clinic complaining of right upper quadrant pain and fever for the past week. She had previously undergone left lateral sectionectomy for recurrent biliary and intrahepatic duct stones 2 years ago. Besides mildly elevated gamma-glutamyl transferase levels, her liver function tests were normal. Magnetic resonance cholangiopancreatography revealed a linear filling defect closely resembling an internal stent from the common bile duct to the right intrahepatic bile duct. A live female A. lumbricoides adult worm was removed by endoscopic retrograde cholangiopancreatography (ERCP). Despite a significant decrease of the ascariasis prevalence in Korea, cases of biliary ascariasis are still occasionally reported. In this study, a additional case of biliary ascariasis, which was radiologically misdiagnosed as the biliary stent, was described in a hepatic resection patient by the worm recovery with ERCP in Korea.
-
Key words: Ascaris lumbricoides, biliary ascariasis, endoscopic retrograde cholangiopancreatography
Introduction
Ascaris lumbricoides is one of the commonest helminths worldwide which infects the human small intestine [
1]. The infection used to be prevalent in Korea until the 1970s but rapidly declined as the social environment improved [
2]. Most patients with intestinal ascariasis remain asymptomatic due to negligible parasite load [
2]. However, the worms sometimes migrate to extraintestinal organs and cause ectopic ascariasis in the form of acute pancreatitis, liver abscess, or biliary stone [
3]. Biliary ascariasis is a rare manifestation that can become a serious illness; however, most physicians in developed countries may not suspect it because of its rare incidence [
3].
Notably, biliary ascariasis may be mistaken for the biliary stent on imaging due to its resemblance with the structure and shape of roundworms. There are reports of a few cases of biliary ascariasis mimicking the biliary stent diagnosed with or without endoscopic retrograde cholangiopancreatography (ERCP) [
4,
5]. However, biliary ascariasis mistaken for a biliary stent on magnetic resonance cholangiopancreatography (MRCP) has never been reported in Korea. Herein, we report a rare case of biliary ascariasis which was radiologically misdiagnosed as a biliary stent in a patient with a history of hepatic resection.
Case Description
In 2017, a 72-year-old female visited our outpatient clinic for pain in the right upper quadrant and epigastric area, accompanied by fever and a chilling sense since the last week. She had undergone ERCP in 1999 for common bile duct (CBD) stones and another ERCP and cholecystectomy in the next year for recurrent CBD stones. She had also undergone a left lateral sectionectomy of the liver for recurrent CBD and an intrahepatic duct (IHD) stone in 2015. She lived in an urban area and denied any history of eating freshwater fish. She was admitted for further evaluation.
Upon examination, her white blood cell count was 6,210×109/L (3.500–10.000×109/L) and the C-reactive protein level was 3 2.7 mg/L (0–5.0 mg/L). No specific abnormality was found on her liver function tests, apart from mildly elevated levels of gamma-glutamyl transferase to 64 IU/L (normal range: 4–34 IU/L); (aspartate transaminase=28 IU/L (normal range: 0–34 IU/L); alanine transaminase=27 IU/L (normal range: 0–40 IU/L); alkaline phosphatase= 110 IU/L (normal range: 30–120 IU/L); total bilirubin=0.6 mg/dL (normal range: 0.3–1.3 mg/dL), and direct bilirubin=0.2 (normal range: 0.0–0.4 mg/dL)).
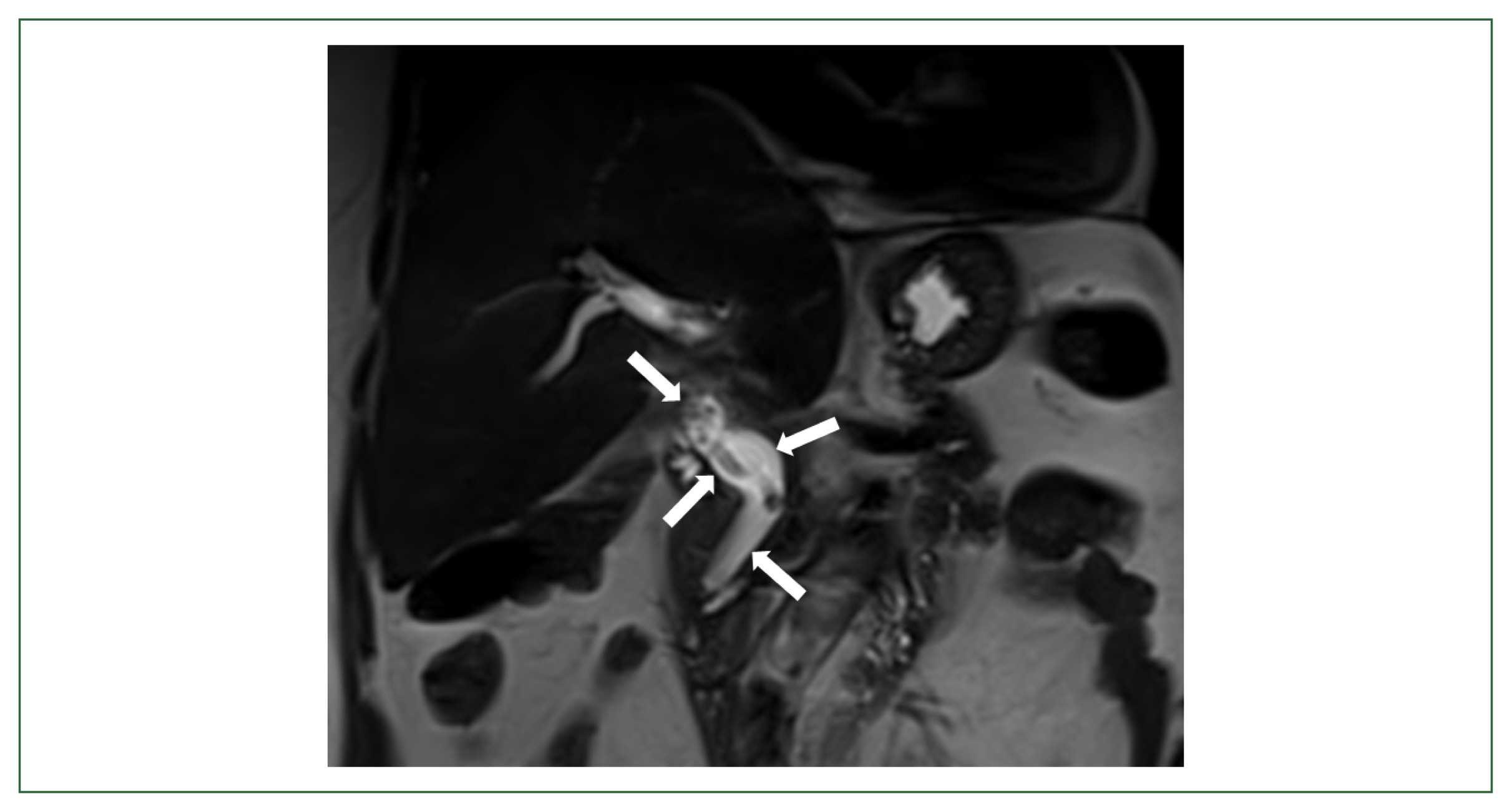
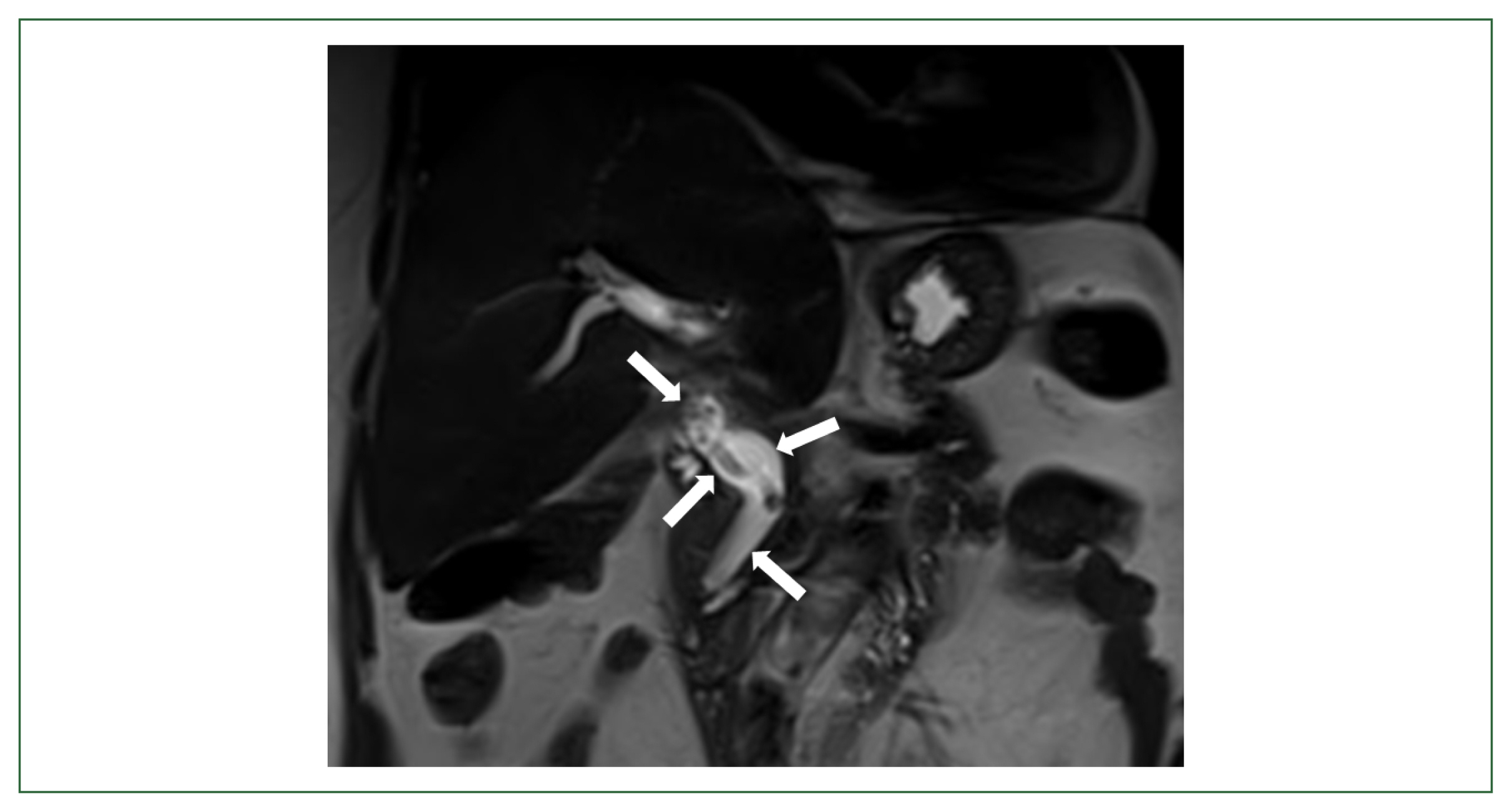
Abdominopelvic computed tomography (APCT) revealed a recurrent CBD stone accompanied by suspicious sludge in the proximal IHD and CBD. After 3 days, T2-weighted coronal MRCP was done which revealed an approximately 4.5 cm hypointense (filling defects) tubular and tortuous structure over the CBD to the right IHD, with features of an internal stent (
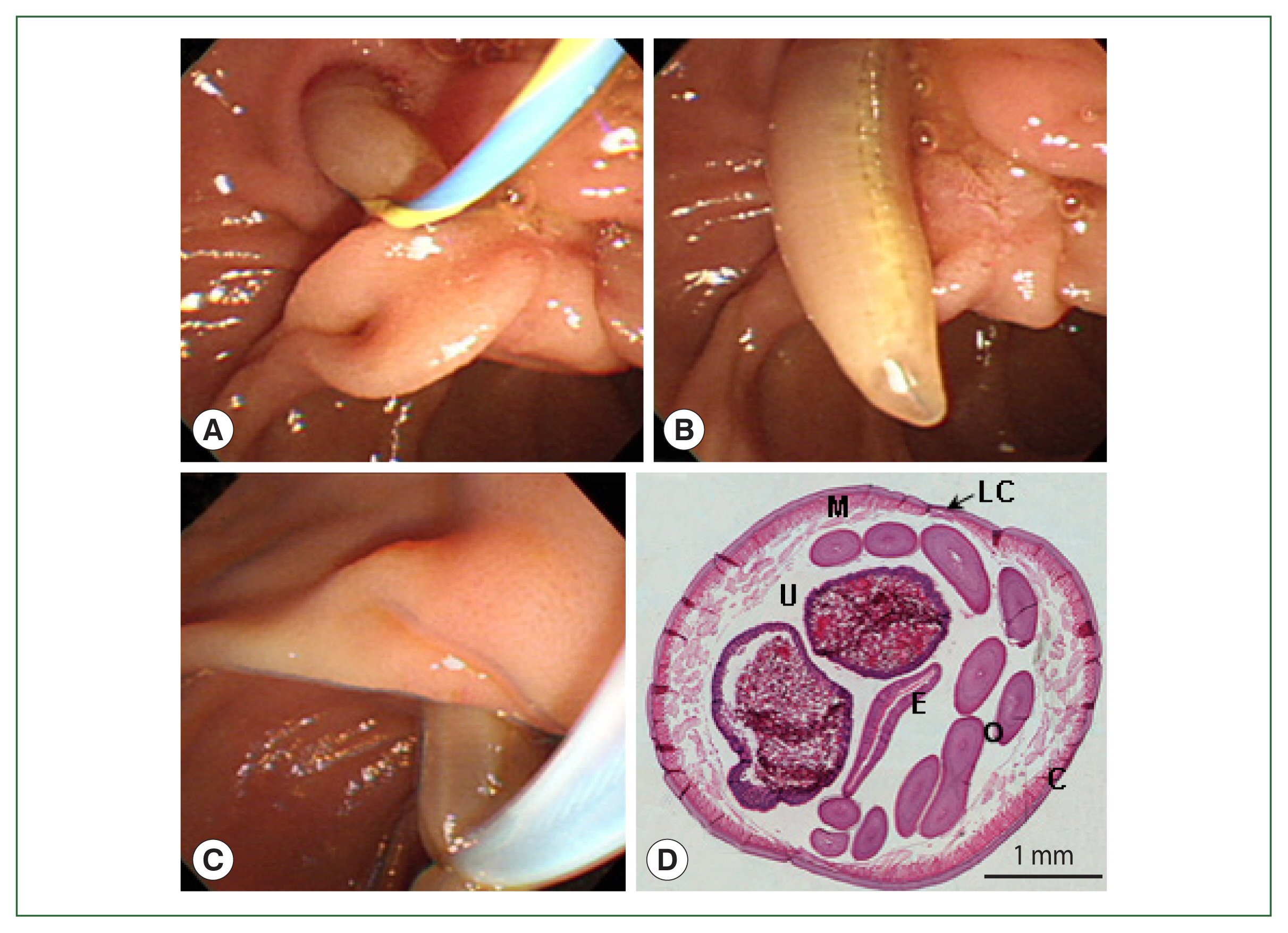
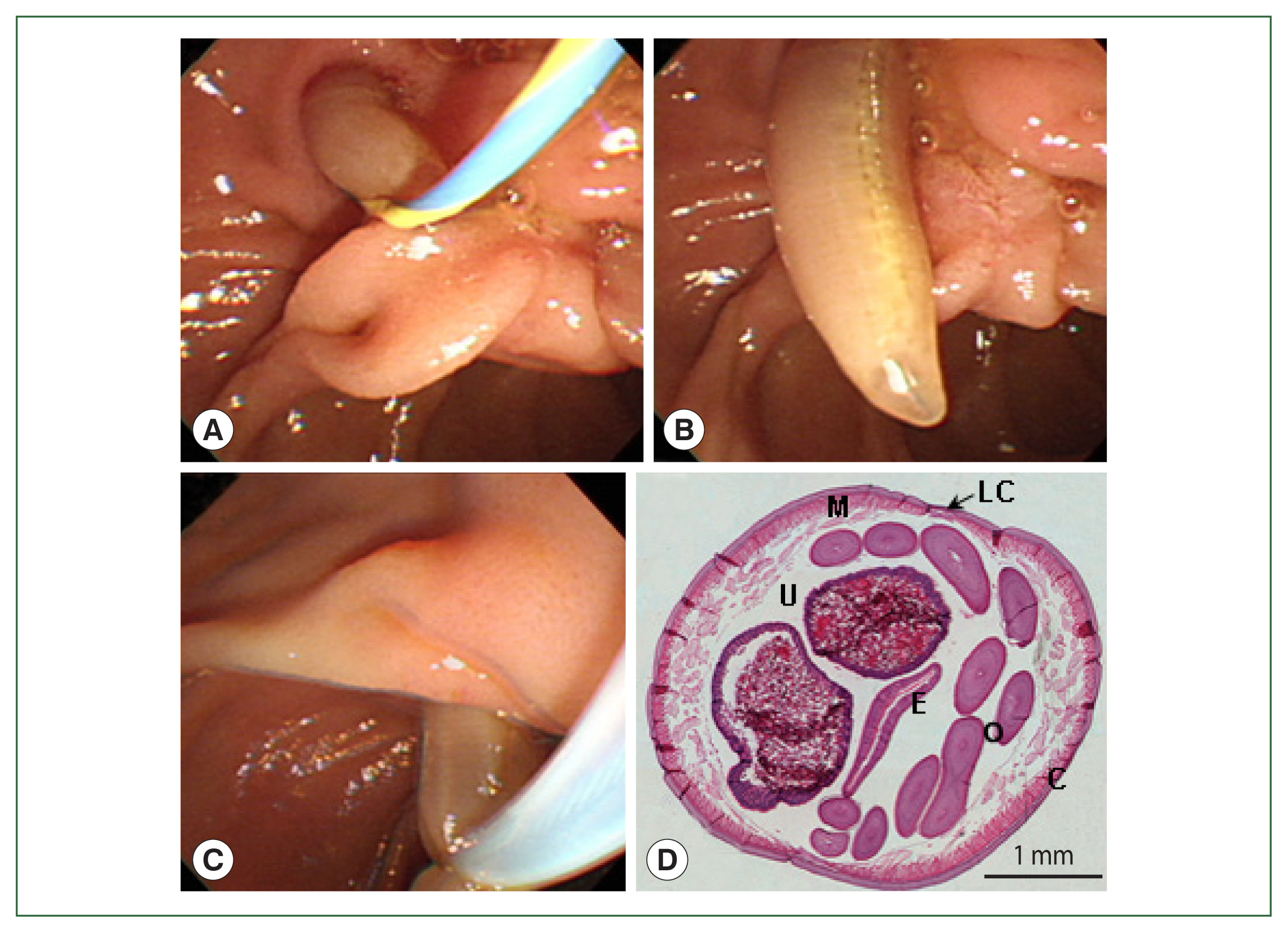
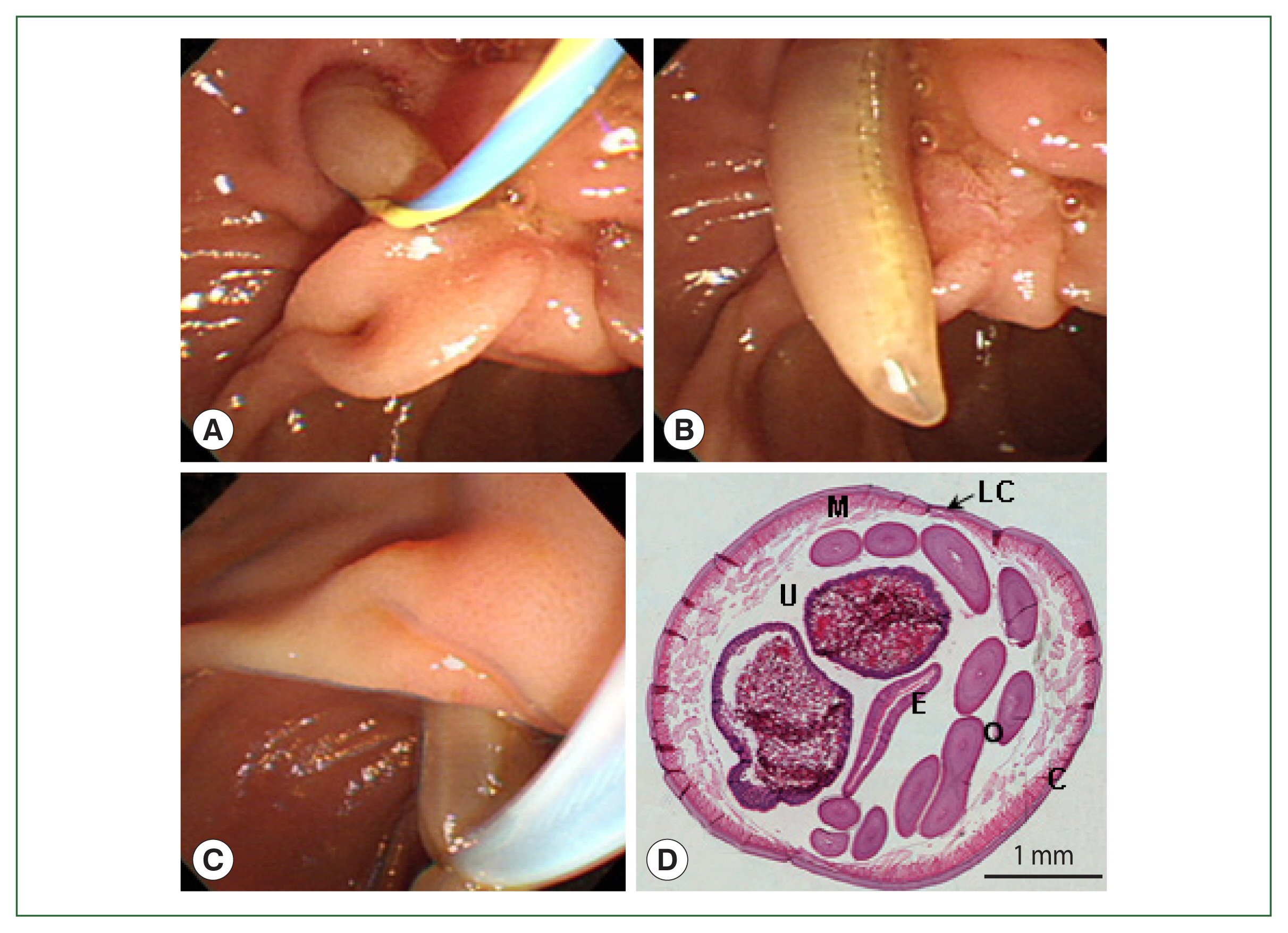
Fig. 1). Because of the patient’s surgical history, we assumed this to be an internal CBD stent inserted during her earlier surgeries. Two days later, ERCP was conducted, during which, surprisingly, a part of a parasitic worm was found in the duodenum, which was then gently extracted with a grasping snare (
Fig. 2A–C). The removed worm was 10 cm long and 5 mm wide with a conical shape.
Histological examination of the cross-section of the worm stained with hematoxylin-eosin revealed characteristic features of
Ascaris lumbricoides, including hypodermal polymyarian muscles, esophagus, oviducts, a pair of lateral cords, and uteri containing numerous underdeveloped eggs (
Fig. 2D). Three days after the ERCP, no further events were observed. The patient was discharged with a prescription for albendazole for herself and her family members. When asked in detail about her medical history and dietary habits, she reported that she had been growing organic vegetables for 10 years on her private farm, using food waste as fertilizer instead of chemical fertilizer. The patient was followed up throughout 5 years at the outpatient clinic; no recurrence or other signs of infection, including in the stool examination, were detected.
Discussion
Ascariasis is one of the most common helminthic infections, especially in several Asian countries, possibly due to their traditional aquaculture and food conventions [
6]. Over the past few decades, the incidence of ascariasis has decreased significantly in Korea due to improvements in personal hygiene and the Green Revolution [
7]. However, biliary ascariasis, known as the most dreadful clinical manifestation, is still occasionally reported in Korea [
8].
Ascaris lumbricoides usually infects the small intestine but can invade the biliary system [
3,
6]. The worm can invade the ampullary orifice causing biliary obstruction, manifesting as biliary colic, obstructive cholangitis, or pancreatitis [
9]. Our patient had a history of farming organic vegetables on her private farm and using homemade organic fertilizer. We assume that she became infected with
Ascaris lumbricoides by ingesting embryonated eggs spread due to this cultivation habit.
Ascariasis is diagnosed when the parasite’s eggs or adult worms are observed in stool microscopy tests [
1]. In our patient, MRCP was conducted first followed by ERCP because of her history of recurrent CBD stones and cholangitis. On ERCP, we identified the worm and confirmed the diagnosis based on its typical histological features. Typical findings of biliary ascariasis on MRCP are a linear hyperintense tubular structure with a hypointense signal in the central area on T1-weighted images [
8]. In our case, because of the patient’s surgical history and the tubular structure visualized on the MRCP, the worm was mistaken for a stent in her biliary tract at first. Since it is difficult to radiologically discriminate between parasites and stents, the surgeon conducting the ERCP must be clearly communicated about any possible stent placement prior to the procedure to avoid such misidentification.
In conclusion, if a patient presents with recurrent obstructive biliary disease, biliary ascariasis may be suspected based on the patient’s dietary and personal habits. A confirmatory diagnosis can be made based on imaging findings suggestive of tubular internal stentlike features.
Notes
-
Author contributions
Conceptualization: Chae H, Suh SK, Choi YS
Investigation: Sohn HJ
Supervision: Choi YS
Visualization: Park HJ
Writing – original draft: Chae H, Suh SK, Sohn HJ
Writing – review & editing: Lee SE, Do JH
-
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Acknowledgment
This study was performed in accordance with the Declaration of Helsinki and an informed consent for publication was obtained from the patient.
Fig. 1Images of the magnetic resonance cholangiopancreatography. The arrows show a linear filling defect (tubular and tortuous appearance) from the common bile duct to the right intrahepatic duct.
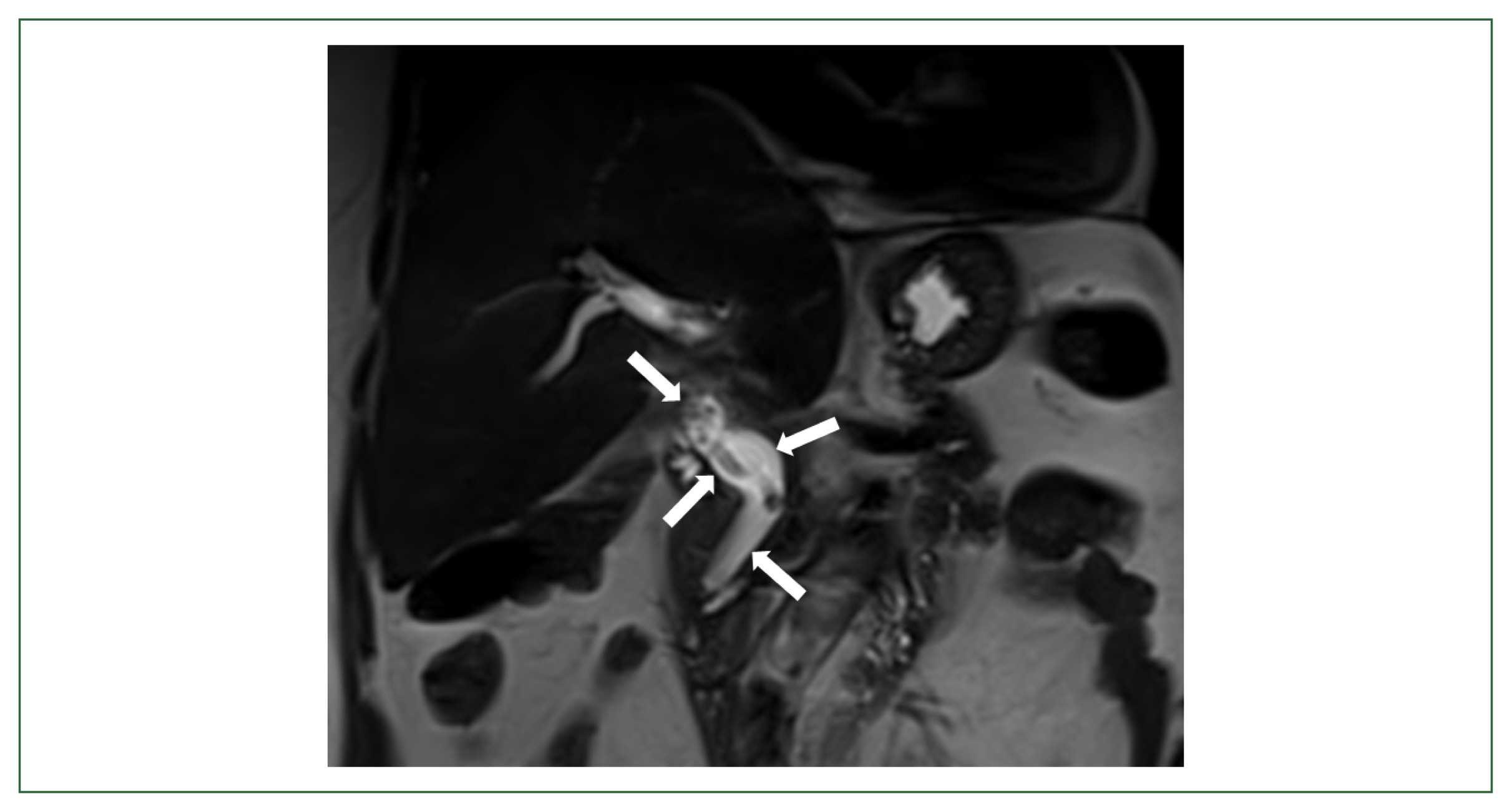
Fig. 2Images of the endoscopic retrograde cholangiopancreatography. (A) The common bile duct was swept with an endoscopic balloon. (B) The parasite was pulled to the duodenum. (C) The parasite was captured and pulled out with an endoscopic snare. (D) Cross-sectional histological features of worm extracted from the bile duct. The section was stained with hematoxylin-eosin×40. C, cuticle; O, ovary/oviduct; E, esophagus; LC, lateral cord; M, myocyte; U, uterus.
References
- 1. Jourdan PM, Lamberton PHL, Fenwick A, Addiss DG. Soil-transmitted helminth infections. Lancet 2018;391(10117):252-265. https://doi.org/10.1016/S0140-6736(17)31930-X
- 2. Kim TS, Cho SH, Huh S, Kong Y, Sohn WM, et al. A nationwide survey on the prevalence of intestinal parasitic infections in the Republic of Korea, 2004. Korean J Parasitol 2009;47(1):37-47. https://doi.org/10.3347/kjp.2009.47.1.37
- 3. Khuroo MS, Rather AA, Khuroo NS, Khuroo MS. Hepatobiliary and pancreatic ascariasis. World J Gastroenterol 2016;22(33):7507-7017. https://doi.org/10.3748/wjg.v22.i33.7507
- 4. Singh D, Yang S, Cappell MS. Biliary ascariasis diagnosed and extracted by ERCP in states. ACG Case Rep J 2016;3(4):e188. https://doi.org/10.14309/crj.2016.161
- 5. Sharma M, Somani P, Prasad R, Jindal S, Pathak A. Biliary ascariasis: mimicker of biliary stent. VideoGIE 2017;2(7):179-181. https://doi.org/10.1016/j.vgie.2017.04.001
- 6. Bethony J, Brooker S, Albonico M, Geiger SM, Loukas A, et al. Soil-transmitted helminth infections: ascariasis, trichuriasis, and hookworm. Lancet 2006;367(9521):1521-1532. https://doi.org/10.1016/S0140-6736(06)68653-4
- 7. Chai JY, Cho SY, Lee SH, Seo BS. Reduction in the incidence of biliary and other surgical complications of ascariasis according to the decrease of its national egg prevalence in Korea. Korean J Parasitol 1991;29(2):101-111. https://doi.org/10.3347/kjp.1991.29.2.101
- 8. Hwang CM, Kim TK, Ha HK, Kim PN, Lee MG. Biliary ascariasis: MR cholangiography findings in two cases. Korean J Radiol 2001;2(3):175-178. https://doi.org/10.3348/kjr.2001.2.3.175
- 9. Das AK. Hepatic and biliary ascariasis. J Glob Infect Dis 2014;6(2):65-72. https://doi.org/10.4103/0974-777X.132042
Citations
Citations to this article as recorded by

- A case of acute pancreatitis caused by biliary ascariasis
Ru-Yu Zheng, Zi-Yue Hu, Yan-Min Kan, Xiang Jing
Asian Journal of Surgery.2025; 48(11): 7178. CrossRef
 , Suk Won Suh1,†
, Suk Won Suh1,† , Yoo Shin Choi1,*, Hee Ju Sohn1, Seung Eun Lee1, Jae Hyuk Do2, Hyun Jeong Park3
, Yoo Shin Choi1,*, Hee Ju Sohn1, Seung Eun Lee1, Jae Hyuk Do2, Hyun Jeong Park3