Abstract
A 36-year old Korean woman consulted a clinic for a regular gynecological examination, and a mass was noticed in her pelvis. She was referred to the Asan Medical Center, Seoul where transvaginal ultrasonography confirmed a pelvic mass exceeding 10 cm in diameter. She received total abdominal hysterectomy and bilateral salpingoophorectomy, and a borderline serous neoplasm with micropapillary features involving the left ovary and right ovarian serosa was histopathologically confirmed. In addition, a section of a nematode with numerous eggs was found in the parenchyma of the left ovary. The worm had degenerated but the eggs were well-preserved and were identified as those of Enterobius vermicularis. She is an incidentally recognized case of ovarian enterobiasis.
-
Key words: Enterobius vermicularis, ovary, ectopic parasitism
Enterobius vermicularis is an intestinal nematode of humans and is especially prevalent among children. It is widely distributed throughout the world, even in developed countries. Normally it lives in the cecum and migrates out through the anus for oviposition. Since it is a lumen-dweller, its infection is not medically serious, but it can be troublesome on rare occasions when the worm invades tissue. The commonest site of tissue invasion is the mucosa and submucosa of the appendix and the next commonest is the female genital tract (
Beaver et al., 1984). The female genital tract is the most frequent site of extraintestinal parasitism of
E. vermicularis because the worm often migrates into the vagina and invades the uterus, uterine tube, ovary, and even the peritoneum (
Saffos and Rhatigan, 1976;
Beckman and Holland, 1981). In addition, rarely it has been reported to form a granuloma in the perineum (
Kim and Chi, 2000), the lung (
Beaver et al., 1973), and the liver (
Little et al., 1973).
When the worm invades tissue it dies within a few days and then degenerates, but its eggs may remain longer. Eggs in tissue may be helpful for diagnosis due to the longevity of the eggshell. We describe briefly a human case of ovarian enterobiasis, which was diagnosed on basis of egg morphology.
A 36-year old woman visited the gynecology clinic of the Seoul Asan Medical Center on 12 June 2001 for the further evaluation of a known pelvic mass. She had previously consulted a private clinic for a regular gynecological examination on 30 May 2001, and had been informed of a cystic mass of 13 cm diameter at her right ovary. Transvaginal ultrasonography revealed a huge pelvic mass of 11.9 × 10.1 × 10.7 cm with a solid and a nodular inner portion. Under the impression of ovarian cancer she received total abdominal hysterectomy, bilateral salpingoophorectomy and omentectomy with a selective pelvic lymph node biopsy on 18 June 2001.
The resected specimen consisted of two ovaries and tubes, uterus, omentum and lymph nodes. The left cystic ovary (12 × 12 × 11 cm, 657 g) with attached fallopian tube (3 cm in length and 0.4 cm in diameter) appeared smooth on its external surface, and the unilocular cyst was found to contain mucoid material. However, the internal surface showed multiple grape-like projections, which measured 6.5 × 6 × 1.8 cm. The cut surface of the projections glistened and was yellowish white in color. The remaining cystic wall had a maximum thickness of 0.5 cm, and showed neither hemorrhage nor necrosis. The fallopian tube was unremarkable.
The right ovary was a grape-like mass (6.5 × 4 × 2 cm and 19 g) and the fallopian tube was 7 cm in length and 0.9 cm in diameter. An aggregate of papillary masses (4.5 × 2.2 × 2 cm in total) was present on the serosal surface of the right ovary. The remaining ovarian parenchyma was unremarkable as was the fallopian tube.
The uterus was symmetric with attached pericervical fat tissue (10 × 7.5 × 4 cm, 146 g). The serosal surface of the uterus was pinkish, focally eroded and hemorrhagic. No definite mass lesion was seen in the uterine serosa. The myometrium and endometrium measured 2.2 and 0.2 cm in thickness respectively. The cervix was unremarkable but the pericervical tissue contained a well-demarcated nodule (1.5 × 1 × 1 cm).
The omentum weighed 160 g and contained no mass. The pelvic lymph nodes were three aggregates of the yellowish fibroadipose tissue, measuring up to 4 × 3 × 1.5 cm.
Histopathological diagnosis was of a borderline serous neoplasm with micropapillary features of the left and right ovary with pericervical invasive implant. The endometrium was in the proliferative phase and the cervix showed chronic inflammation and squamous metaplasia.
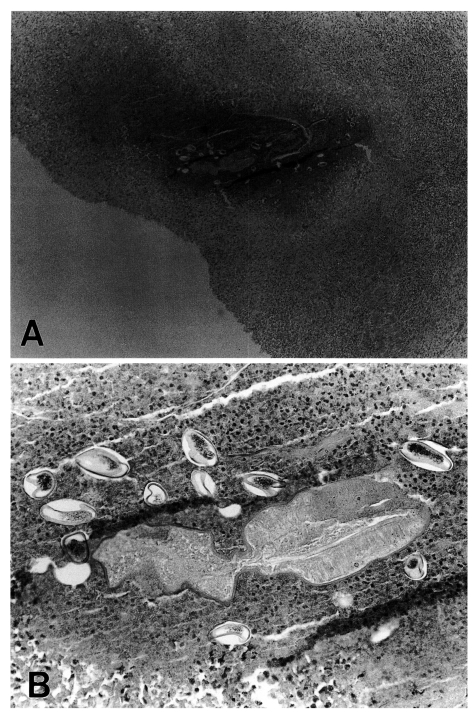
In the left ovary, a necrotic focus was found in the parenchyma, and this was surrounded by granulation tissue. A section of a nematode was observed in the center of the necrotic tissue and several eggs were scattered around the worm section (
Fig. 1A). The sectioned worm had a thick cuticular surface but the other structures had degenerated and were thus difficult to identify (
Fig. 1B). The body diameter measured 600-800 µm. Several eggs were observed amongst the inflammatory cells surrounding the worm (
Fig. 1B). Eggs included a germ in the thick chitin shell (
Fig. 1B), and measured 56-60 × 27-30 µm with one convex side. The size and shape of the eggs identified them as belonging to
E. vermicularis.
Ovarian enterobiasis is rare but several cases have been recorded (
Beckman and Holland, 1981). The uterine tubes and peritoneal serosa are common sites of ectopic enterobiasis. The majority of the cases have reported symptom of abdominal pain. All of the cases have been identified by surgical biopsy of the involved organs. The present case showed no specific subjective symptoms related with ovarian enterobiasis probably because of coincidental ovarian cancer. Ovarian enterobiasis is rare but it still occurs in Korea.
References
- 1. Beaver PC, Jung RC, Cupp EW. Clinical Parasitology. 1984, 9th ed. Philadelphia. Lea & Febiger.
- 2. Beaver PC, Kriz JJ, Lau TJ. Pulmonary nodule caused by Enterobius vermicularis. Am J Trop Med Hyg 1973;22:711-713.
- 3. Beckman EN, Holland JB. Ovarian enterobiasis - a proposed pathogenesis. Am J Trop Med Hyg 1981;30:74-76.
- 4. Kim S, Chi JG. Perianal granuloma caused by a female pinworm (Enterobius vermicularis) - A case report -. Korea J Pathol 2000;34:605-607.
- 5. Little MD, Cuello CJ, D'Alessandro A. Granuloma of the liver due to Enterobius vermicularis report of a case. Am J Trop Med Hyg 1973;22:567-569.
- 6. Saffos RO, Rhatigan RM. Unilateral salpingitis due to Enterobius vermicularis. Am J Clin Pathol 1976;67:296-299.
Fig. 1Histopathological finding of the ovary, HE stained. A. A section of a nematode in the necrotic tissue, original magnification × 15. B. High power view of the nematode section and nearby eggs, original magnification ×300.

Citations
Citations to this article as recorded by

- "Diagnostic challenges, atypical presentations, and therapeutic implications in ectopic Enterobius vermicularis infections: a global systematic review."
Sadaf Roodbarani, Reza Ghasemikhah
Diagnostic Microbiology and Infectious Disease.2026; 114(2): 117136. CrossRef - Pinworm (Enterobius Vermicularis) Infestation: An Updated Review
Alexander K.C. Leung, Joseph M. Lam, Benjamin Barankin, Alex H.C. Wong, Kin F. Leong, Kam L. Hon
Current Pediatric Reviews.2025; 21(4): 333. CrossRef - Imaging microwave field of chip surfaces based on scanning microwave microscopy
Fan Cheng, Zhenrong Zhang, Tao Pei, Xudong Jia, Yifan Xue, Huan Fei Wen, Zhonghao Li, Hao Guo, Zongmin Ma, Jun Tang, Jun Liu
Physica Scripta.2023; 98(7): 075502. CrossRef - Ovarian Filariasis in a Wild Southern Tamandua (Tamanduatetradactyla; Mammalia: Myrmecophagidae)
Lilja Fromme, Débora Regina Yogui, Mario Henrique Alves, Josué Díaz-Delgado, Arnaud Leonard Jean Desbiez, André Luis Quagliatto Santos, Juliana Mariotti Guerra, Marion Langeheine, Ursula Siebert, Ralph Brehm, José Luiz Catão-Dias, Pedro Enrique Navas-Suár
Pathogens.2022; 11(8): 918. CrossRef - The incidence of pinworm (Enterobius vermicularis) in pre-school and school aged children in the Eastern Slovakia
A. Dudlová, P. Juriš, P. Jarčuška, Z. Vasilková, V. Vargová, M. Sumková, V. Krčméry
Helminthologia.2018; 55(4): 275. CrossRef - Recurrent paediatric pinworm infection of the vagina as a potential reservoir for Enterobius vermicularis
B. Kashyap, J.C. Samantray, S. Kumar, R. Jhamb, A.K. Singh, I.R. Kaur
Journal of Helminthology.2014; 88(3): 381. CrossRef - Clinical Update on Parasitic Diseases
Min Seo
Korean Journal of Medicine.2013; 85(5): 469. CrossRef - Spontaneous Premature Ovarian Failure in the Very Young: The Enigma Continues
Nirmala Duhan, Krishna Dahiya, Kiran Yadav, Sunita Singh, Veena Gupta
Journal of Gynecologic Surgery.2011; 27(4): 231. CrossRef -
Enterobius vermicularis in the kidney: an unusual location
Estelle Cateau, Mokrane Yacoub, Christian Tavilien, Bertrand Becq-Giraudon, Marie-Hélène Rodier
Journal of Medical Microbiology
.2010; 59(7): 860. CrossRef - Enterobius Vermicularis Infection of Female Genital Tract
A. Siochou, H. Birtsou, M. Papazahariadou
International Journal of Immunopathology and Pharmacology.2008; 21(4): 1031. CrossRef - Enterobius vermicularis infection in uterine cavity mimicking endometrial cancer: a case report
Yucel Karaman, Banu Bingol, Ziya Gunenc, Onat Akýn
Gynecological Surgery.2007; 4(3): 217. CrossRef - Enterobius vermicularis in the male urinary tract: a case report
Athanasios Zahariou, Maria Karamouti, Polyanthi Papaioannou
Journal of Medical Case Reports.2007;[Epub] CrossRef