Abstract
The present study aimed to evaluate control efficacy of clonorchiasis by two schemes of repeated treatment with praziquantel at two endemic villages In China. Residents of one village at Guangxi Autonomous Region were treated and examined 6-monthly and of another at Liaoning Province 12-monthly. In residents that took 25 mg/kg x3 (total 75 mg/kg) of praziquantel every 6 months for one year the egg positive rate showed a significant drop from 69.0% to 17.1%. In contrast, a group of same praziquantel medication once showed a slight marginal decrease in the egg rate from 18.9% to 12.2% after one year. Of 39 subjects examined 3 times, 56.4% were cured, 7.7% persistently positive, one (2.6%) reinfected after cure or newly infected, but 25.6% were persistently negative. The present finding suggests that 6-monthly medication with 75 mg/kg of praziquantel should effectively lower the prevalence but incomplete for control of clonorchiasis in heavy endemic areas.
-
Key words: clonorchiasis, control, praziquantel, repeated medication
INTRODUCTION
Clonorchis sinensis (Cobbold, 1875) Looss, 1907 is one of major human parasitic trematodes in East Asia. Infected population by this trematode is estimated over 10 million in China (
Li et al., 1993) and one million in Korea (
MHSW & KAH, 1997). Clonorchiasis induces several pathological changes in the infected bile ducts, such as duct dilatation, mucosal hyperplasia, periductal fibrosis, purulent cholangitis and abscess formation, cholelithiasis, and cholangiocarcinoma (
Rim, 1986). Epidemiological data strongly suggest that old infected people of clonorchiasis die earlier because of the accumulated effects of heavy infection and the associated complications (
Seo et al., 1981). Therefore, clonorchiasis is one of the major health problems to be solved in an endemic society.
In this context, well-organized activity for the control of clonorchiasis is really important for the well being of residents in the endemic zones of East Asia. After introduction of praziquantel, all of the diagnosed clonorchiasis cases were effectively treated in Korea. However, the clonorchiasis infection rate is decreasing very slowly compared to rapid decrease of ascariasis or hookworm infection in Korea (
MHSW & KAH, 1997). This slow decrease is interpreted as an outcome of either treatment failure by inappropriate medication or re-infection after cure. Recently a control trial involving clonorchiasis concluded that complete control is difficult (
Hong et al., 1998).
The present study sought to investigate control efficacy by repeated praziquantel medication to infected Chinese residents who praziquantel has never been tried.
MATERIALS AND METHODS
Subjected population and fecal examination
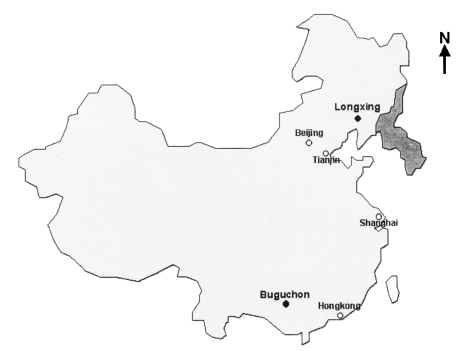
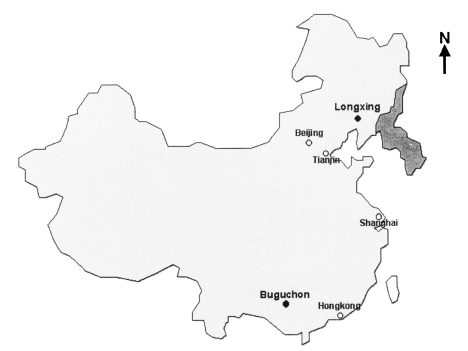
Buguchon in Guangxi Autonomous Region and Longxing in Liaoning Province in China were selected for the study area after fecal screening (
Fig. 1). Buguchon is a village of Zuang minority (population 450) and Longxing of Korean minority (population 600). All of them were verbally noticed of the program and the fecal specimens of residents were collected on voluntary contribution. One feces was examined once by the Kato-Katz method and once by the formalin-ether concentration technique. Eggs of
C. sinensis were counted by the Kato-Katz method, to arrive at an estimate of EPG (number of eggs per gram of feces). The subjected population aged from 4 to 71 and was of both genders.
At Buguchon, Guangxi, egg positive cases were treated with praziquantel (Distocide™, Shin Poong Pharmaceutical Co. Ltd., Seoul) every 6 months. In October 1998 and June 1999, the recommended dose (25 mg/kg, 3 times a day) of praziquantel was given. In June 1999, all of the egg positive cases of intestinal nematodes were medicated with 400 mg single dose of albendazole (Alzental™, ShinPoong Pharmaceutical Co. Ltd., Seoul). At Longxing, Liaoning, egg positive cases of C. sinensis were also treated once with praziquantel at the recommended dose (25 mg/kg, 3 times a day) and examined after one year.
A committee of Korean and Chinese experts, which was organized by the Korea Association of Health, reviewed the protocol of the examinations and treatments for feasibility and ethics, and the provincial health bureau of Guangxi Autonomous Region and Liaoning Province accepted its implementation in 1997 and 1998 respectively.
RESULTS
In Buguchon, the egg positive rate of clonorchiasis was 69.0% at the beginning of the exercise and significantly decreased to 17.1% (p < 0.001) after two medications (
Table 1). In Longxing, the rate was 18.9% pre-treatment and 12.2% (0.05 < p < 0.1) after annual chemotherapy (
Table 1). Most of them counted of their EPG and were grouped into five as presented in
Table 2. Most of them were lightly infected under EPG 999 but some of them were counted of their EPG over 10,000 (
Table 2). Total enrolled subjects, who were examined once or more, were 288 in Buguchon where the residents were 450. The compilation of subjected population is summarized in
Table 3, and also the table presents the positive rate of clonorchiasis by age and gender. The rate of males in Buguchon was 76.2% and of females 53.3% (p < 0.001). The rate of males under 10 was 25.0%, but increased according to age and up to 100% in 50s (p < 0.001,
Table 3).
The mean EPG of the whole subjected residents in Buguchon was 2,436 at the beginning but this increased to 5,603 after one year (
Table 4). This sudden increase was mainly made by 4 newly included cases of heavy burden at the third examination; their EPG counts were 30,348, 22,560, 22,080, and 27,288. The 39 subjects in Buguchon, who were examined 3 times are concerned, their mean EPG counts were 2,008 at the first examination but dropped to 1,363 at the second, and 512 at the third (
Table 4). In contrast, EPG count in Longxing dropped from 4,814 to 491 after one one-year medication, which represents good egg reduction of praziquantel (p = 0.012,
Table 4).
As for the cure rate of the mass selective treatments, two 6-monthly treatments in Buguchon showed 80% and one 12-monthly treatment In Longxing 60% (p < 0.002). The egg reduction rate of two 6-monthly treatments in Buguchon was 95.4% (p < 0.001) and one 12-monthly treatment in Longxing 95.9% (p < 0.001,
Table 4).
When subjected cases of the 3 examinations at Buguchon were concerned, 39 were included 3 times, 74 were twice, and 101 were once (
Table 5). Of the 39 subjects, 3 (7.7%) were consistently positive while 22 (56.4%) were cured during medications. Ten (25.6%) remained consistently negative in the endemic village.
DISCUSSION
Buguchon, Guangxi is a heavy endemic area of clonorchiasis. where about 70% of residents were egg positive while the other village, Longxing, Liaoning is a light endemic area. Though the endemicity is much different, both villages were in natural equilibrium state of clonorchiasis transmission because no anthelmintic intervention had been tried there. In Buguchon, males are more Infected than females and the egg positive rate increases by age up to 50s, and therefore males in 50s show the highest egg positive rate, 100%. The epidemiological characteristic of the highest rate in males of 50s in Buguchon is same as previously observed In Korea (
Seo et al., 1981;
Rim, 1986).
The present finding clearly demonstrates that repeated selective mass treatments with praziquantel at 6-months interval would significantly reduce the prevalence of clonorchiasis while one 12-monthly medication induces a little decrease. Although two 6-monthly medications produce 80% of overall cure rate, the cure rate of one 6-monthly medication showed a poor cure rate of 30%, which is quite unusual. Several factors may interfere the cure but improper medication of the subjects at the first trial is mostly possible.
The mean EPG counts at Buguchon increased one year after two full-dose medications. At the second examination, the cases of higher EPGs disappeared but they reappeared at the third. All of the four cases whose EPGs were over 20,000 at the third examination were included for the first time and had neither examination nor medication previously. They undoubtedly caused the sudden increase of EPGs at the third examination. As only EPG counts of previously treated cases are concerned, mean EPGs drop to 512 from 2008 after two 6-monthly medications with the egg reduction rate of 95.4% and that of one 12-monthly medication 95.9%. These rates are very similar to the known rate (
Rim et al., 1981;
Seo et al., 1983).
One paper (
Hong et al., 1998) recorded an experience on control of clonorchiasis in Korea with repeated praziquantel treatments, which concerned residents of a moderately endemic village in which the egg positive rate was 22.7% before treatment. Egg positive cases detected by 6-monthly examinations were selectively treated with 75 mg/kg of praziquantel every 6 months 7 times, and the final rate was successfully decreased to 6.3%. That study involved about 100 residents of a small rural village and was actively supported by well-trained field workers. In addition, the residents were very cooperative and took health education, and therefore, the result should be viewed as the best achievable at the village level. Furthermore, most of the infected cases were lightly infected, and the control activity was continued over a 3-year period. Nonetheless, the control activity of clonorchiasis was incomplete, which suggests prolonged and wide scale activity is required for complete control.
Another paper recorded poor cure effect of praziquantel on clonorchiasis in Vietnam (
Tinga et al., 1999). They treated 21 subjects with praziquantel 25 mg/kg o.d. for 3 days and found 29% cure. They described the result surprising and discussed many factors for the poor cure. The problem of the trial is undoubtedly the dosage, which is definitely under-dosed for proper cure of the worms In the bile duct. Since metabolized praziquantel in bile juice kills the worms (
Andrews et al., 1983), three consecutive doses of 25 mg/kg praziquantel with 5-hours interval in a day are essential to keep its effective concentration in bile (
Rim, 1986). The recommended full dosage of praziquantel gives the best cure rate of 83-85% in clonorchiasis (
Rim et al., 1981;
Seo et al., 1983).
When the 39 residents, who were subjected 3 times, were considered, 23 (59%) were cured during the study period but 3 (7.8%) of them remained persistently positive. The three positives may result from treatment failure or reinfection. Since three (7.8%) of the subjects became more heavily or re-infected after cure, about 10% of them contracted new infection during the period of control activity. Contrary to this, though the transmission force of clonorchiasis was strong in the village 10 (25.6%) remained negative throughout the study period. Since, eating raw freshwater fish exclusively contracts C. sinensis infection, these people must have avoided eating raw fish.
It is apparent that praziquantel is not completely effective at its recommended dosage, but it is the drug of choice for clonorchiasis. Furthermore, it is recommended that praziquantel should be taken in three separate doses, and it is difficult to ensure that people adequately take the three doses. The second or third dose is easily dropped, forgotten or delayed, and thus, the real cure rate becomes much lower than expected. This is an important limiting factor of the control activity offered by the praziquantel medication program in the field. The present low cure rate may suggest an actual outcome of three doses of praziquantel in the field.
In addition, there is another limitation of such a human study, because some of the subjects were temporarily unavailable during the study period. This kind of control study at the field level should consider dropping or adding new cases during the study period because of moving activity in their regular life. In the present study total 288 subjects were enrolled in Buguchon where whole population was 450, and actually only 39 of them were continuously included during the 3 examinations and treatments.
In Thailand, opisthorchiasis, which is epidemiologically and clinically similar with clonorchiasis, was the target of a decade long control program (
Jongsuksuntigul and Imsom-boon, 1997). The program was comprehensive in scope and included 3 synergistic approaches; fecal examination and treatment of egg positive cases, health education to prevent new infection, and the sanitary disposal of feces. The program made some success in decreasing the prevalence of infection from 34.6% to 24.0% after one year, However, the comprehensive measures are theoretically excellent for controlling liver fluke disease but practically not looking so good as expected. Another experience of opisthorchiasis control recorded that seven of 32 subjects were egg positive after praziquantel treatment in Thailand (
Pungpak et al., 1998). Comparing the efforts and expenses involved, the outcome of the control activity of opisthorchiasis looks no better than that of the present study or that of a previous control study of clonorchiasis (
Hong et al., 1998).
Control of a helminthiasis by a selective mass chemotherapy should consider the impact of the chemotherapy on transmission dynamics of the helminthiasis (
Anderson and Medley, 1985). Effective control may be achieved when the mass chemotherapy is strong enough to interrupt the reinfection. The reinfection force depends upon egg seeding power of the helminth, environmental factors for completion of larval development, and behavioral or social factors (
Anderson and Medley, 1985). Egg seeding into the environment is the beginning of transmission of clonorchiasis and thus the amount of eggs in the environment determines the reinfection power. Therefore praziquantel has been quite promising for control of clonorchiasis because its egg reduction rate is excellent enough to minimize the egg seeding. When a mass selective praziquantel medication is introduced in a large scale over a long enough period, transmission of clonorchiasis must be controlled.
In conclusion, repeated treatment with praziquantel at 6-monthly intervals is an effective method of reducing the endemicity and infection intensity of clonorchiasis. However complete control is difficult unless the control activity runs for a long period and in wide enough area.
Notes
-
The present study was supported by the research grant (HMP-97-M-2-0015) from the Ministry of Health and Welfare, Korea, 1997.
ACKNOWLEDGMENTS
The authors appreciate assistance of Dr. Lan Yang, Dr. Hongman Zhang and staff at the Guangxi Institute of Parasitic Diseases, Nanning, Guangxi, and Dr. Fenghua LI and staff at the Liaoning Province Public Health and Anti-Epidemic Station, Shenyang, Liaoning, China. The staff of the Korea Association of Health also supported this study technically and administratively. Prof. Keun-Young Yoo at Department of Preventive Medicine Seoul National University College of Medicine kindly helped statistical analysis of the data.
References
- 1. Anderson RM, Medley GF. Community control of helminth infections of man by mass and selective chemotherapy. Parasitology 1985;90:629-660.
- 2. Andrews P, Thomas H, Pohlke R, Seubert J. Praziquantel. Med Res Rev 1983;3:147-200.
- 3. Hong ST, Yoon K, Lee M, et al. Control of clonorchiasis by repeated praziquantel treatment and low diagnostic efficacy of sonography. Korean J Parasitol 1998;36:249-254.
- 4. Jongsuksuntigul P, Imsomboon T. The impact of a decade long opisthorchiasis control program in Northeastern Thailand. Southeast Asian J Trop Med Publ Health 1997;28:551-557.
- 5. Li B, Wang E, Cao Y, Cao Y. Clonorchis sinensis and clonorchiasis. 1997, Shenyang, China. Shenyang Publ Co..
- 6. Ministry of Health and Welfare, Korea Association of Health. Prevalence of intestinal parasitic infections in Korea - the Sixth Report. 1997, Seoul, Korea.
- 7. Pungpak S, Radomyos P, Radomyos BE, Schelp FP, Jongsuksuntigul P, Bunnag D. Treatment of Opisthorchis viverrini and intestinal fluke infections with praziquantel. Southeast Asian J Trop Med Publ Health 1998;29:246-249.
- 8. Rim HJ. The current pathobiology and chemotherapy of clonorchiasis. Korean J Parasitol 1986;24(suppl):5-141.
- 9. Rim HJ, Lyu KS, Lee JS, Joo KH. Clinical evaluation of the therapeutic efficacy of praziquantel (Embay 8440) against Clonorchis sinensis infection in man. Ann Trop Med Parasitol 1981;75:27-33.
- 10. Seo BS, Lee SH, Cho SY, et al. An epidemiological study on clonorchiasis and metagonimiasis in riverside areas in Korea. Korean J Parasitol 1981;19:137-150.
- 11. Seo BS, Lee SH, Chai JY, Hong ST. Praziquantel (Distocide) in treatment of Clonorchis sinensis infection. Korean J Parasitol 1983;21:241-245.
- 12. Tinga N, Van De N, Vien HV, et al. Little effect of praziquantel or artemisinin on clonorchiasis in northern Vietnam. A pilot study. Trop Med Internat Health 1999;4:814-818.
Fig. 1Sites of the study; Buguchon, Guangxi province and Longxing, Liaoning province, People's Republic of China.
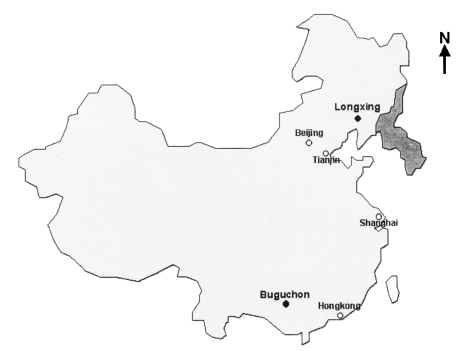
Table 1.Egg positive rate of Clonorchis sinensis and other intestinal helminths in Buguchon, Guangxi, and Longxing, Liaoning, China
Table 1.
|
Villages/Date |
No. of exam. |
No (%) of egg positive subjects
|
|
Csa)
|
Al |
Tt |
Hw |
Total |
|
Buguchon, Guangxi |
|
|
|
|
|
|
|
Oct. 98 |
100 |
69 |
21 |
22 |
6 |
82 |
|
|
(69.0) |
(21.0) |
(22.0) |
(6.0) |
(82.0) |
|
Jun. 99 |
101b)
|
38 |
38 |
16 |
1 |
64 |
|
|
(37.6) |
(37.6) |
(15.8) |
(1.0) |
(63.4) |
|
Nov. 99 |
181 |
31 |
24 |
18 |
4 |
58 |
|
|
(17.1) |
(13.3) |
(9.9) |
(2.2) |
(32.0) |
|
Longxing, Liaoning |
|
|
|
|
|
|
|
Oct. 98 |
487b)
|
92 |
16 |
2 |
0 |
106 |
|
|
(18.9) |
(3.3) |
(0.4) |
|
(21.8) |
|
Sep. 99 |
139 |
17 |
0 |
0 |
0 |
17 |
|
|
(12.2) |
|
|
|
(12.2) |
Table 2.Proportion of clonorchiasis subjects by EPG grades in Buguchon, Guangxi and Longxing, Liaoning
Table 2.
|
Villages/Date |
No. of subjects by EPG Grades
|
|
1-999 |
1000-4999 |
5000-9999 |
10000-19999 |
20000- |
Total |
|
Buguchon, Guangxi |
|
|
|
|
|
|
|
Oct. ‘98 |
36 |
14 |
7 |
2 |
2 |
61 |
|
Jun. ‘99 |
30 |
10 |
1 |
4 |
0 |
45 |
|
Nov. ‘99 |
12 |
7 |
2 |
l |
4 |
26 |
|
Longxing, Liaoning |
|
|
|
|
|
|
|
Oct, ‘98 |
27 |
11 |
3 |
1 |
3 |
45 |
|
Sep. '99 |
18 |
0 |
0 |
0 |
0 |
18 |
Table 3.Positive rate of clonorchiasis by age and sex among whole examined residents in Buguchon, Guangxi
Table 3.
|
Age group |
Sex |
No. of cases
|
Positive rate (%) |
|
Examineda)
|
Positive |
|
0-9 |
Male |
24 |
6 |
25.0 |
|
Female |
22 |
7 |
31.8 |
|
Total |
46 |
13 |
28.3 |
|
10-19 |
Male |
24 |
15 |
62.5 |
|
Female |
21 |
10 |
47.6 |
|
Total |
45 |
25 |
55.6 |
|
20-29 |
Male |
26 |
22 |
84.6 |
|
Female |
18 |
8 |
44.4 |
|
Total |
44 |
30 |
68.2 |
|
30-39 |
Male |
36 |
33 |
91.7 |
|
Female |
30 |
17 |
56.7 |
|
Total |
66 |
50 |
75.8 |
|
40-49 |
Male |
25 |
24 |
96.0 |
|
Female |
26 |
18 |
69.2 |
|
Total |
51 |
42 |
82.3 |
|
50-59 |
Male |
4 |
4 |
100.0 |
|
Female |
8 |
6 |
75.0 |
|
Total |
12 |
10 |
83.3 |
|
60-69 |
Male |
12 |
11 |
91.7 |
|
Female |
10 |
7 |
70.0 |
|
Total |
22 |
18 |
81.8 |
|
70# |
Male |
0 |
0 |
- |
|
Female |
2 |
0 |
0 |
|
Total |
2 |
0 |
0 |
|
Total |
Male |
151 |
115 |
76.2 |
|
Female |
137 |
73 |
53.3 |
|
Total |
288 |
188 |
65.3 |
Table 4.Changes of egg positive rates and EPG counts of Clonorchis sinensis during repeated praziquantel treatments
Table 4.
|
Medication schemes |
Changes by examinations at
|
|
Pre-treatment |
6-months post-treatment |
12-months post-treatment |
|
Egg positive rate (%) |
|
|
|
|
25 mg/kg x3, 6-months |
69.0a)
|
37.6a)
|
17.1a)
|
|
25 mg/kg x3, 6-monthsb)
|
66.7a)
|
41.0a)
|
15.4a)
|
|
25 mg/kg x3, 12-months |
18.9 |
- |
12.2 |
|
Mean EPG counts (± S.D.) |
|
|
|
|
25 mg/kg x3, 6-months |
2436 (± 4168) |
2181 (± 4242) |
5603 (± 9531) |
|
25 mg/kg x3, 6-monthsb)
|
2008 (± 4952)a)
|
1363 (± 3118)a)
|
512 (± 541)a)
|
|
25 mg/kg x3, 12-months |
4814 (± 5011)a)
|
- |
491 (± 523)a)
|
|
Cure rate (%)c)
|
|
|
|
|
25 mg/kg x3. 6-months |
- |
30.0a)
|
80.0a)
|
|
25 mg/kg x3, 12-months |
- |
- |
60.0 |
|
Egg reduction rate (%)c)
|
|
|
|
|
25 mg/kg x3, 6-months |
- |
36.6a)
|
95.4a)
|
|
25 mg/kg x3, 12-months |
- |
- |
95.9 |
Table 5.Number of cases by results during the 3 examinations in Buguchon
Table 5.
|
Examined |
Results at the exam.
|
No, of cases (%) |
|
1st |
2nd |
3rd |
|
|
|
|
39 |
|
3 times |
+ |
+ |
+ |
3 (7.7) |
|
+ |
- |
- |
11 (28.2) |
|
+ |
- |
- |
11 (28.2) |
|
+ |
- |
+ |
1 (2.6) |
|
- |
+ |
+ |
1 (2.6) |
|
- |
+ |
- |
1 (2.6) |
|
- |
- |
+ |
1 (2.6) |
|
- |
- |
- |
10 (25.6) |
|
|
|
|
77 |
|
2 times |
|
+ |
+ |
14 (18.2) |
|
|
+ |
- |
26 (33.8) |
|
|
- |
+ |
2 (2.6) |
|
|
- |
- |
35 (45.5) |
|
|
|
|
101 |
|
once |
|
|
+ |
37 (36.6) |
|
|
|
- |
64 (63.4) |