Abstract
The present study was performed to describe 2 cases of human thelaziasis (HT) which occurred in Gyeongsangnam- do and to briefly review the previously reported Korean cases. A 58-year old woman, residing in Hadong-gun, Gyeongsangnam-do, came to Gyeongsang National University Hospital (GNUH) complaining of foreign body sensation and itching of the right eye in March 2000. Total 6 adult nematodes of Thelazia callipaeda (2 males and 4 females) were detected in her right eye. A 80-year old man, residing in Jinju-si, Gyeongsangnam-do, came to GNUH complaining of foreign body sensation, itching, and pain of the right eye in December 2007. A total of 5 worms (4 females and 1 degenerated) were removed from his right eye. We analyzed characteristics of the total 39 Korean HT cases reported to date, including the present 2 cases. Most of the cases (71.8%) occurred in Seoul and Gyeonggi-do before 2000, and 21 cases (53.8%) were males and 18 (46.2%) were females. The prevalence was higher in younger ages below 30 years (48.7%) than 31-60 years (41.0%) and over 61 years (10.3%). The seasonal prevalence showed a higher incidence in autumn (43.6%) than in other seasons. Most of the cases (94.9%) were conjunctival sac infections and only 2 (5.1%) were intraocular cases. The present 2 HT cases are the first reported cases in Gyeongsangnam-do. Some characteristics of Korean HT cases were analyzed.
-
Key words: Thelazia callipaeda, thelaziasis, case report, review
INTRODUCTION
Nematode parasites of the genus
Thelazia are clinically important, causing insect-borne zoonoses in humans. More than 10 species have been reported in various parts of the world. Among them,
Thelazia callipaeda, the oriental eye worm, is widespread in domestic and wild animals in Asian countries, Italy, France, and Germany, and it is sometimes found in humans in China, India, Thailand, Indonesia, Japan, and Korea [
1-
4]. In the Republic of Korea, a total of 37 human infection cases were reported in the literature since the first one by Nakada (1934) [
5-
32]. Recently, we found 2 cases of human
thelaziasis (HT) that occurred in Gyeongsangnam-do, and we analyzed characteristics of the overall 39 Korean HT cases, including the present 2 cases.
CASE RECORD
Case 1
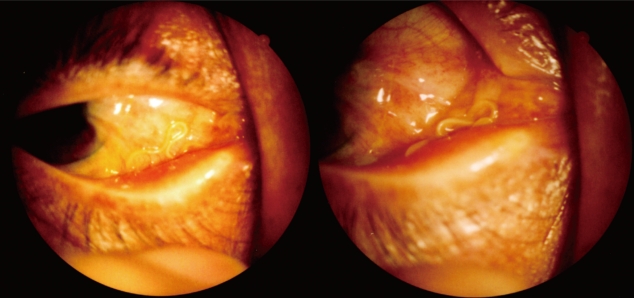
A 58-year old woman, residing in Hadong-gun, Gyeongsangnam- do, came to Gyeongsang National University Hospital (GNUH) complaining of foreign body sensation and itching of the right eye in March 2000. She had a trabeculectomy in her right eye in GNUH about 10 years ago, and lost the sight of the right eye about 1 year ago. At ordinary times, she engaged in farming and gathered wild vegetables in the mountains. Many dogs were raised in her residential village, and she used the vally water as drinking water. Thread-like worms were found in the lower conjunctival sac of the right eye, and total 6
Thelazia callipaeda adult worms (2 males and 4 females) were extracted at GNUH (
Fig. 1).
A 80-year old man, residing in Jinju-si, Gyeongsangnam-do, came to GNUH complaining of foreign body sensation, itching, and pain of the right eye in December 2007. He had climbed a mountain 1 month before. At 10 days after the mountain climbing, 1 worm was incidentally found and reISSN moved by a physician in a local hospital in Jinju-si, Gyeongsangnam- do. A total of 4 worms (3 females and 1 dead and degenerated) were extracted from his right eye. At 1 month later, 1 female worm was also removed from his right eye at GNUH.
DESCRIPTION OF WORMS
Among 10 worms collected, 6 females and 1 male were fixed with 10% hot formalin, cleared in alcohol-glycerin solution, mounted in glycerin-jelly, and observed under a light microscope (LM) with a micrometer. To observe the surface ultrastructure, remainders, 2 females and 1 male, were washed several times with 0.2 M cacodylate buffer (pH 7.2) and fixed with 2.5% glutaraldehyde at 4℃. After washing 3 times with the buffer, they were dehydrated through a graded alcohol series (50%, 70%, 80%, 90%, 95%, and absolute alcohol), dried with hexamethyldisilazane, coated (JFC-1100E ion sputtering device) with gold, and observed with a scanning electron microscope (Philips XL-30S, Einthoven, The Netherlands) at an accelerating voltage of 20 kV.
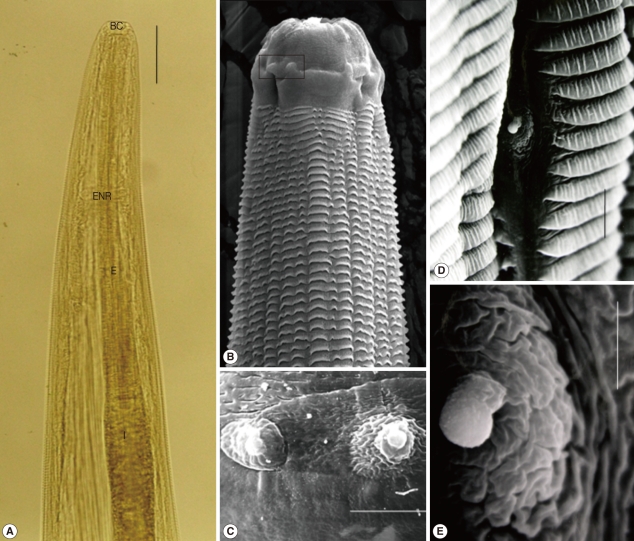
The male worm was 12.4×0.44 mm in size, had a scalariform buccal cavity (0.025×0.033 mm), a long muscular esophagus (0.65 mm long), and a coiled tail. In the scanning electron microscopic (SEM) study, the cephalic part (about 0.028×0.044 mm) with the buccal cavity, 2 cephalic papillae, and a body papilla which located at anterior 1/10 in a longitudinal groove, were characteristically observed in the anterior portion. Folded transverse striations were arranged on the anterior surface from just behind the cephalic part. Their densities were about 375 rows per 1 mm length of the cuticle (
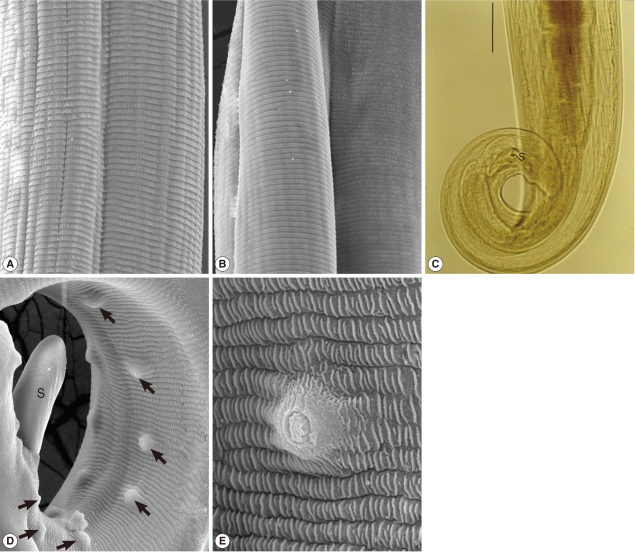
Fig. 2). Cuticular transverse striations arranged in the middle and posterior portions were about 220 and 240 rows per 1 mm length, respectively. A spicule and dome-shaped papillae, 7 pairs of preanal, and 2 pairs of postanal papillae were observed in the coiled tail part (
Fig. 3).
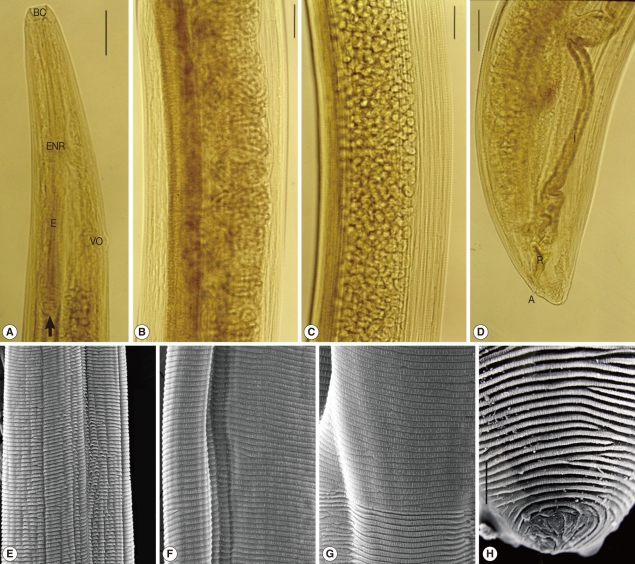
Females were 17.0-18.5×0.39-0.49 mm (17.7×0.44 mm on average) in size, had a scalariform buccal cavity (0.028×0.033 mm), a long muscular esophagus (0.70 mm long) and a conical tail. Vulva openings were located at 0.52-0.6 mm (0.57 mm on average) from the anterior end and at more anterior portion than the esophago-intestinal junction. Numerous coiled larvae were contained in the proximal part of the uterus, and lots of eggs were present in the distal part of the uterus. In the SEM study of the body surface, folded transverse striations arranged on the anterior surface were about 250 rows per 1 mm length. Cuticular transverse striations arranged in the middle and posterior portions were about 170 and 375 rows per 1 mm length, respectively. Encircled striations were distributed on the posterior end (
Fig. 4).
DISCUSSION
In the present study, 2 cases of HT were reported for the first time in Gyeongsangnam-do. Therefore, including the present 2 cases, a total of 39 cases of HT have been documented in the Republic of Korea. Among them, 28 cases (71.8%) occurred in Seoul and Gyeonggi-do (Province), and the remainders (11 cases) occurred in Chungcheongbuk-do (2 cases), Jeollabuk-do (1 case), Gyeongsangbuk-do (1 case), Daegu (1 case), Gyeongsangnam-do (2 cases), Busan (1 case), and other areas (3 cases). It is interesting to note that all 5 cases reported from Southeastern parts (Gyeongsangbuk-do, Daegu, Gyeongsangnam- do, and Busan) occurred after 2000, whereas all cases of Seoul and Gyeonggi-do occurred before 2000 (
Table 1). The plenty of HT cases in Seoul and Gyeonggi-do may be related to an abundance of academic facilities and manpowers which can aware and report the parasitic disease, as well as to the increase of outdoor activities of residents. However, it is meaningful to see that HT cases are now being reported chiefly in Southeastern parts after 2000. In China, a total of 371 HT cases had been reported by 2005, and most of them occurred in rural populations unlike in Korea [
4].
Total 3 cases were reported before the 1960s. Among them, 2 cases occurred in the Northern part of Korea, Hwanghae-do and Pyeonganbuk-do [
5-
7]. There were no reports during the 1960s, 6 (15.4%) in the 1970s, 11 (28.2%) in the 1980s, 13 (33.3%) in the 1990s, and 6 (15.4%) after 2000. A total of 21 (53.8%) cases were males and 18 (46.2%) were females. By age groups, 19 cases (48.7%) occurred below 30 years of age, 16 cases (41.0%) in 31-60 years, and 4 cases (10.3%) at over 61 years (
Table 1). On the other hand, a review on the analysis of 179 Chinese HT cases revealed 51% from females and 49% from males, and showed that the majority (64.2%) of patients were children younger than 6 years [
4].
Seasonal prevalences were clearly shown in the cases of Korean HT. The highest incidence of 17 cases (43.6%) occurred in autumn (6 cases in September: 5 in October, and 6 in November). In the summer season, total 7 (17.9%) cases (1 case in June, 3 in July, and 3 in August) occurred. A total of 5 (12.8%) and 3 (7.7%) cases were encountered in winter (4 cases in December and 1 in January) and spring (each 1 case in March, April, and May). There was no case in February, and the occurrence date was unknown in 7 (17.9%) cases. The prevalence (69.2%) of the second half year, from July to December, is much higher than that (12.8%) of the first half year, from January to June. Therefore, seasonal tendency may be related to increasing outdoor activities of humans and increase of the vector population.
A total of 146 worms (44 males, 62 females, and 40 unknown) were recovered from all 39 Korean cases. The individual worm burden was 1-15 worms per patient (3.7 on average). In the case of the maximum worm burden (15 worms), the infection recurred at 25 days after the primary worm recovery (10 worms) [
31]. Kim and Shin [
24] removed 14 worms at once from the right eye of a 7-year old girl in July 1989. A total of 21 cases (52.5%) had infection in the right eye, 16 (40.0%) in the left eye, 3 (7.5%) unknown, and only 1 case had infection in both eyes. Only in 2 cases (5.1%), worms were found in the intraocular sites, whereas in the most of cases (94.9%), worms were detected in the conjunctival sac [
30,
32].
The chief complaints of Korean cases with
T. callipaeda, especially conjunctival sac infections, were foreign body sensation (78.8%), itching (48.5%), and lacrimation (36.4%). They sometimes complained of hyperemia and hemorrhage of the eyes, mild visual disturbances, blurring sensation, and pain as the minor symptoms. The visual disturbance, floaters, myodesopsia, and vitreous opacity were manifested in intraocular cases [
30,
32].
For diagnosis of HT, identification of worms extracted from the eye is important. Therefore, many researchers observed morphological characteristics, including surface ultrastructure, of worms recovered from human cases [
21,
23,
27,
33-
35]. We also examined the morphologies of
T. callipaeda worms recovered from a case to provide more clear and profitable information in this study. Internal structures, such as the scalariform buccal cavity, muscular esophagus, esophageal nerve ring, intestine, rectum, anus, spicule, vulva opening, vagina, and larvae and eggs in uteri, were well visualized in light microscopic observations. Surface ultrastructures, including the cephalic part, cephalic papillae, body papilla, transverse striations by body portions, spicule, and preanal and postanal papillae, were well revealed by the SEM study. The morphological findings observed in this study were well coincided with those of the previous studies. However, the fine and clear LM and SEM images obtained in this study will be helpful to identify
T. callipaeda from HT cases [
21,
23,
27,
33-
35].
References
- 1. Miyazaki I. Section III. Nematode Zoonoses. 32. Thelaziasis. An Illustrated Book of Helminthic Zoonoses. 1991, Tokyo, Japan. International Medical Foundation of Japan; pp 362-368.
- 2. Otranto D, Ferroglio E, Lia R, Traversa D, Rossi L. Current status and epidemiological observations of Thelazia callipaeda (Spirurida, Thelaziidae) in dogs, cats and foxes in Italy: A 'coincidence' or a parasitic disease of the Old Continent? Vet Parasitol 2003;116:315-325.
- 3. Kosin E, Kosman ML, Depary AA. First case of human thelaziasis in Indonesia. Southeast Asian J Trop Med Public Health 1989;20:233-236.
- 4. Shen J, Gasser RB, Chu D, Wang Z, Yuan X, Cantacessi C, Otranto D. Human thelaziosis-A neglected parasitic disease of the eye. J Parasitol 2006;92:872-876.
- 5. Nakada K. Examples of the parasite Thelazia callipaeda in humans in Korea. J Chosen Med Assoc 1934;24:939-944.
- 6. Suzuki H. A case of Thelazia callipaeda infection in conjunctival sac. Juoganka Iho 1935;27:1129-1130.
- 7. Sillman ET. A Korean case of infection with Thelazia callipaeda with notes on human thelaziasis. J Parasitol 1953;39:669-670.
- 8. Chu JK, Cho YJ. A case report of human thelaziasis. Korean J Parasitol 1973;11:83-86. (in Korean).
- 9. Im KI, Kim SJ, Min DY, Kim SD, Lew HM. A human infection with Thelazia sp. in Korea. Yonsei Rep Trop Med 1974;5:136-139.
- 10. Oh CK, Youn WS, Cho SY, Seo BS. A case report of human thelaziasis. J Korean Ophthalmol Soc 1975;16:431-434. (in Korean).
- 11. Choi WY, Lee WK, Lee OR, Shin HH, Shin NY. A case of human thelaziasis in Seoul. Korean J Parasitol 1977;15:127-132.
- 12. Choi DK, Cho SY. A case of human thelaziasis concomitantly found with a reservoir host. J Korean Ophthalmol Soc 1978;19:125-129. (in Korean).
- 13. Lee KH, Kim YT, Sohn MS, Lee JS, Rim HJ. A case report of human thelaziasis in Korea. J Korean Ophthalmol Soc 1979;20:135-138. (in Korean).
- 14. Hong ST, Lee SH, Shim YB, Choi JS, Choe JK. A human case of thelaziasis in Korea. Korean J Parasitol 1981;19:76-80. (in Korean).
- 15. Im KI, Ahn MH, Kim JJ, Kim HB. A case of human thelaziasis in Korea. Korean J Parasitol 1982;20:60-63. (in Korean).
- 16. Cha IS, Kim HJ. A case of thelaziasis. J Korean Ophthalmol Soc 1983;24:651-653. (in Korean).
- 17. Hong ST, Lee SH, Han H. A human case of thelaziasis in Korea. Korean J Parasitol 1985;23:324-326.
- 18. Ryu JS, Im KI, Byun YJ, Kim SC. A case of human thelaziasis in Korea. Korean J Parasitol 1987;25:83-84.
- 19. Lee BS, Jung HR, Eom KS, Joo KH, Rim HJ. A case of human thelaziasis in Korea. J Korean Ophthalmol Soc 1986;27:85-90. (in Korean).
- 20. Lee PW, Kim CW, Cho BC. A case report of human thelaziasis. J Korean Ophthalmol Soc 1987;28:495-498. (in Korean).
- 21. Hong ST, Lee SH, Kim SI. A human case of Thelazia callipaeda infection with reference to its internal structure. Korean J Parasitol 1988;26:137-140.
- 22. Min HK, Chun KS. A case of human thelaziasis occurred in both eyes. Korean J Parasitol 1988;26:133-135.
- 23. Choi WY, Youn JH, Nam HW, Kim WS, Kim WK, Park SY, Oh YW. Scanning electron microscopic observation of Thelazia callipaeda from humans. Korean J Parasitol 1989;27:217-223.
- 24. Kim DC, Shin H. Two cases of human thelaziasis. J Korean Ophthalmol Soc 1990;31:801-805. (in Korean).
- 25. Lee SW, Kang SW, Lee JO, Eom KS. Two cases of Thelazia callipaeda infestation. J Korean Ophthalmol Soc 1994;35:1132-1136. (in Korean).
- 26. Kim YK, Song BR, Yoo JH, Yong TS. Two cases of human thelaziasis. J Korean Ophthalmol Soc 1994;35:223-228. (in Korean).
- 27. Hong ST, Park YK, Lee SK, Yoo JH, Kim AS, Chung YH, Hong SJ. Two human cases of Thelazia callipaeda infection in Korea. Korean J Parasitol 1995;33:139-144.
- 28. Lee CH, Kim SY, Kim DC, Choi TY. Five cases of human thelaziasis. J Korean Ophthalmol Soc 1998;39:2827-2831. (in Korean).
- 29. Oh TS, Ahn Y. A cases of Thelazia callipaeda conjunctival infestation. J Korean Ophthalmol Soc 2000;41:1437-1440. (in Korean).
- 30. Jeong JW, Park JW, Kong HH, Chung DI, Kwak MS, Cho YW. A cases of intraocular Thelazia callipaeda infestation. J Korean Ophthalmol Soc 2006;47:1517-1523. (in Korean).
- 31. Lee SM, Shin KM, Kim DH, Kang BN. A cases of Thelazia callipaeda recurred at a one-month interval. J Korean Ophthalmol Soc 2010;51:895-898. (in Korean).
- 32. Kim HW, Kim JL, Kho WG, Hwang SY, Yun IH. Intraocular Infestation with Thelazia callipaeda. Jpn J Ophthalmol 2010;54:370-372.
- 33. Arizono N, Yoshida Y, Kondo K, Kurimoto H, Oda K, Shiota T, Shimata Y, Ogino K. Thelazia callipaeda from man and dogs in Kyoto and its scanning electron microscopy. Jpn J Parasitol 1976;25:402-408.
- 34. Kagei N, Uga S, Kugi G. On the caudal papillae of male of Thelazia callipaeda Railliet and Henry, 1910. Jpn J Parasitol 1983;32:481-484.
- 35. Otranto D, Lia RP, Traversa D, Giannetto S. Thelazia callipaeda (Spirurida, Thelaziidae) of carnivores and humans: Morphological study by light and scanning electron microscopy. Parassitologia 2003;45:125-133.
Fig. 1The right eye of the first case (58-year-old man) infected with Thelazia callipaeda adult worms.

Fig. 2Light microscopic (LM) (A) and scanning electron microscopic (SEM) views (B-E) of the anterior portion of T. callipaeda male worms. (A) The buccal cavity (BC), muscular esophagus (E), esophageal nerve ring (ENR), and intestine (I) are seen (scale bar=0.1 mm). (B) Anterior portion with the buccal cavity, 2 cephalic papillae (in box) and cuticular folded striations, which were arranged about 375 rows per 1 mm length. (C) Enlarged view of 2 nipple-like cephalic papillae (scale bar=5 µm). (D) A body papilla located at anterior 1/10 in a longitudinal groove (scale bar=5 µm). (E) Enlaged view of a body papilla (scale bar=2.5 µm).

Fig. 3Middle and posterior portions of T. callipaeda males. (A) SEM view of the middle portion with cuticular striations, which were arranged in about 220 rows per 1 mm length. (B) SEM view of the posterior portion with cuticular striations, which were arranged about 240 rows per 1 mm length. (C) LM view of posterior end with a coiled tail (scale bar=0.1 mm). (D) SEM view of the posterior end with a spicule (S) and 7 pairs of postanal papillae (arrow marks). (E) Enlarged view of a postanal papilla.

Fig. 4LM (A-D) and SEM views (E-H) of T. callipaeda females. (A) Anterior portion with the scalariform buccal cavity (BC), a long muscular esophagus (E), and a vulva opening (VO) which is located at more anterior portion than the esophago-intestinal junction (arrow) (scale bar=1 mm). (B) The proximal part of the uterus with numerous coiled larvae (scale bar=1 mm). (C) The distal part of the uterus with lots of eggs (scale bar=1 mm). (D) The posterior end of a worm with the rectum (R) and anus (A) (scale bar=1 mm). (E) The anterior portion with folded transverse striations, which were arranged about 250 rows per 1 mm length. (F) The middle portion with transverse striations, which were arranged about 170 rows per 1 mm length. (G) The posterior portion with transverse striations, which were arranged about 375 rows per 1 mm length. (H) The posterior end with encircled striations (scale bar=10 µm).

Table 1.Analytical summery of thelaziasis cases reported in the Republic of Korea
Table 1.
|
Items |
No. of cases reported in
|
Total (%) |
|
Before the 1960’s |
1970’s |
1980’s |
1990’s |
2000-present |
|
Sex |
|
|
|
|
|
|
|
Male |
2 |
3 |
6 |
9 |
1 |
21 (53.8) |
|
Female |
1 |
3 |
5 |
4 |
5 |
18 (46.2) |
|
Total (%) |
3 (7.7) |
6 (15.4) |
11 (28.2) |
13 (33.3) |
6 (15.4) |
39 (100.0) |
|
Age |
|
|
|
|
|
|
|
Below 20 |
3 |
2 |
1 |
2 |
1 |
9 (23.1) |
|
21-30 |
- |
4 |
4 |
2 |
- |
10 (25.6) |
|
31-40 |
- |
- |
3 |
1 |
- |
4 (10.3) |
|
41-50 |
- |
- |
2 |
4 |
- |
6 (15.4) |
|
51-60 |
- |
- |
1 |
3 |
2 |
6 (15.4) |
|
61-70 |
- |
- |
- |
1 |
- |
1 (2.6) |
|
Over 71 |
- |
- |
- |
- |
3 |
3 (7.7) |
|
Total |
3 |
6 |
11 |
13 |
6 |
39 (100.0) |
|
Residential district of cases |
|
|
|
|
|
|
|
Seoul |
1 |
6 |
5 |
5 |
- |
17 (43.6) |
|
Gyeonggi-do |
- |
- |
5 |
6 |
- |
11 (28.2) |
|
Chungcheogbuk-do |
- |
- |
- |
2 |
- |
2 (5.1) |
|
Jeollabuk-do |
- |
- |
1 |
- |
- |
1 (2.6) |
|
Gyeongsangbuk-do |
- |
- |
- |
- |
1 |
1 (2.6) |
|
Daegu |
- |
- |
- |
- |
1 |
1 (2.6) |
|
Gyeongsangnam-do |
- |
- |
- |
- |
2 |
2 (5.1) |
|
Busan |
- |
- |
- |
- |
1 |
1 (2.6) |
|
Others |
2a
|
- |
- |
- |
1b
|
3 (7.7) |
|
Total |
3 |
6 |
11 |
13 |
6 |
39 (100.0) |
|
Eyes infected |
|
|
|
|
|
|
|
Right |
- |
3 |
5 |
10 |
3 |
21 (52.5) |
|
Left |
1 |
3 |
7 |
2 |
3 |
16 (40.0) |
|
Unknown |
2 |
- |
- |
1 |
- |
3 (7.5) |
|
Total |
3 |
6 |
12c
|
13 |
6 |
40 (100.0) |
|
No. of worms detected |
|
|
|
|
|
|
|
Male |
1 |
5 |
11 |
20 |
7 |
44 (30.1) |
|
Female |
1 |
3 |
20 |
20 |
18 |
62 (42.5) |
|
Unknown |
1 |
5 |
7 |
20 |
7 |
40 (27.4) |
|
Total |
3 (2.1) |
13 (8.9) |
38 (26.0) |
60 (41.1) |
32 (21.9) |
146 (100.0) |