Abstract
The aim of this study was to test the susceptibility of mice to Trypanosoma evansi treated with human plasma containing different concentrations of apolipoprotein L-1 (APOL1). For this experiment, a strain of T. evansi and human plasma (plasmas 1, 2, and 3) from 3 adult males clinically healthy were used. In vivo test used 50 mice divided in 5 groups (A to E) with 10 animals in each group. Animals of groups B to E were infected, and then treated with 0.2 ml of human plasma in the following outline: negative control (A), positive control (B), treatment with plasma 1 (C), treatment with plasma 2 (D), and treatment with plasma 3 (E). Mice treated with human plasma showed an increase in longevity of 40.9±0.3 (C), 20±9.0 (D) and 35.6±9.3 (E) days compared to the control group (B) which was 4.3±0.5 days. The number of surviving mice and free of the parasite (blood smear and PCR negative) at the end of the experiment was 90%, 0%, and 60% for groups C, D, and E, respectively. The quantification of APOL1 was performed due to the large difference in the treatments that differed in the source plasma. In plasmas 1, 2, and 3 was detected the concentration of 194, 99, and 115 mg/dl of APOL1, respectively. However, we believe that this difference in the treatment efficiency is related to the level of APOL1 in plasmas.
-
Key words: Trypanosoma evansi, mouse, treatment, human plasma, apolipoprotein-1
Trypanosoma evansi is a hemoprotozoan flagellate causing trypanosomosis in a variety of mammalian hosts [
1]. This parasite has a wide geographic distribution and causes severe diseases in animals of significant tropical areas, especially Africa and Latin America [
2].
T. evansi is spread mainly by species of bloodsucking flies (
Tabanus sp.,
Chrysops sp., and
Hematopota sp.) and hematophagous bats [
3].
Humans were considered refractory to infection by
T. evansi [
4], but a case of human infection was reported in an Indian farmer in 2005 [
5]. After this case, researchers found in an Indian village, about 22% of the population positive for the parasite through blood smears and serology techniques [
6]. It is known that humans have innate immunity against
T. brucei. Researchers attributed this condition due to the presence of apolipoprotein L-1 (APOL1) in human blood, and this protein would have a trypanocidal factor, since it has the ability to lyse
T. brucei [
7]. In the case reported by researchers [
5], later was found APOL1 deficiency in the blood, which could have contributed to the development of the disease [
8]. Our research group recently found that mice infected with
T. evansi, when exposed to human plasma and blood, had their longevity extended, and some animals shed the parasite [
9,
10]. In view of these findings, this study aimed to assess the susceptibility of mice to
T. evansi treated with human plasmas with different concentrations of APOL1.
A strain of
T. evansi from a naturally infected dog [
11] was used in this experiment. One Wistar rat was infected intraperitoneally with 0.2 ml of blood (10
6 parasites/animal) cryopreserved in liquid nitrogen. This procedure was performed to obtain a larger number of parasites in the blood for further testing in vivo.
The plasma used in this study was obtained from 3 clinically healthy men, aging 23 (plasma 1), 25 (plasma 2), and 27 (plasma 3) years old; all of them with A+ blood type. Blood was collected into tubes containing anticoagulant (EDTA 10%), and centrifuged to separate plasma, which was stored in tubes in liquid nitrogen. The state of health of humans was confirmed by complete blood count, and liver and renal biochemical analysis. Were also evaluated by a doctor, and clinical examination was normal (clinically healthy humans, and hematological and biochemical tests unchanged).
For the in vivo test 50 mice divided into 5 groups with 10 animals in each group were used: negative control (A), positive control (B), and human plasma: T2 (C), T3 (D), and T4 (E). The volume of 0.1 ml of blood from the Wistar rat containing 2.4×10
6 trypanosomes was administered to mice of groups B to E, intraperitoneally. Then, 24 hr post-inoculation, treatments were carried out with different plasmas. The dose used in the treatment was 0.2 ml of plasma for groups C, D, and E, intraperitoneally. These animals were monitored daily by blood smears stained with Quick Panoptic and analyzed at 100×magnification [
12], during 41 days of the experiment. This study evaluated the mean and SD of the prepatent period, longevity, mortality, and success of treatments in mice experimentally infected with
T. evansi after treatment with human plasma. Data were subjected to analysis of variance (ANOVA) followed by the Tukey test.
The technique of immunoassay, i.e., quantitative sandwich-ELISA, was used. Monoclonal antibodies specific for APOL1 in a plate ELISA (anti-APOL1 antibody produced in goat) (Sigma-Aldrich, St. Louis, USA). The samples (100 µl) were pipetted, with the standards and the conjugates bound by peroxidases enzymes forming an antibody-antigen-antibody conjugate. Subsequently, the plate was washed in microplate washer (Awareness®) to remove any unbound substance, and then was added to a solution containing substrate (tetramethylbenzidine + hydrogen peroxide), observing the color development proportional to the amount of APOL1 linked. The reaction was stabilized by the addition of sulfuric acid (2 N) and the color intensity measured by an ELISA reader (Biotek®) (Biotek, Nevada, USA). The results were expressed as APOL1 mg/dl, and the calculations made from standard curves as a guidance kit, using SPSS version 10.0.
Genomic DNA was extracted from the brains using the phenol-chloroform method [
13] and subjected to electrophoresis on agarose gel at 1% for determining the quality and quantification of samples. PCRs were performed using primers specific for
T. evansi [
14]; Te664a (5' GTC AAA CCC CTC TTG GAG G 3') and Te664b (5' CAT ATC CTA AGA GTT GT 3') at a concentration of 1 µm each, 1.5 U of Platinum Taq DNA Polymerase (Invitrogen, São Paulo, Brazil) with 1×reaction buffer, 1.5 mM MgCl
2, 250 mm in each dNTP, and 1 µl of DNA. The reactions were subjected to an initial denaturation at 95℃ for 3 min, followed by 35 cycles consisting of 3 steps; 95℃ for 1 min, 56℃ for 1 min, and 72℃ for 1 min. Finally, we performed a final extension at 72℃ for 10 min. The amplified samples were analyzed by electrophoresis on 1% agarose gel at 80V for 1 hr, stained with ethidium bromide and photographed under UV light. As a positive control, we used DNA from
T. evansi purified by chromatography on DEAE-cellulose, and sterile ultrapure water was used as a negative control instead of DNA.
In mice treated with human plasma, an increase in the animal longevity was observed when compared to the positive control group (
Table 1). During the 41 days of experiment, the mortality was observed in all mice of groups B and D. Group C and E had 1 and 4 animals dead, respectively. In the negative control (group A), no mice died.
The quantification of APOL1 was performed due to the large difference in the treatments that differed in the source plasma (
Table 1). In plasmas 1, 2, and 3 was detected the concentration of 194, 99, and 115 mg/dl of APOL1, respectively. For men, the references value of APOL1 oscillated within 107-214 mg/dl.
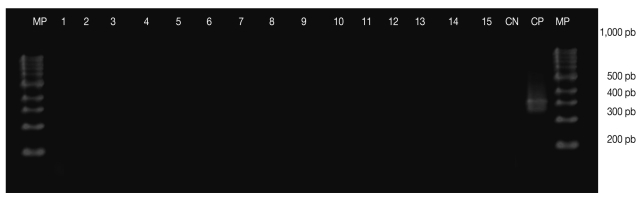
Nine animals of group C and 6 mice from group E subjected to PCR showed negative results for the parasite (
Fig. 1). Therefore, there were observed efficiencies of 90% (group C), 0% (group D), and 60% (group E) of plasma treatment against
T. evansi (
Table 1). At the end of the experiment, the rats were alive, and PCR and blood smear were negative.
Our research group has been investigating in recent years alternative treatments for therapy of infections caused by
T. evansi. The main reason for these investigations is the fact that the ordinary chemotherapy with diminazene aceturate, dipropionate imidocarb, and suramim, commonly used in the treatment of trypanosomosis, has been shown ineffective in many cases [
15-
17]. According to researchers, these drugs have limited effectiveness, due not to exceed the hematoencephalic barrier, a refuge area to the flagellate during the residual period of the drugs; or excess the barrier, but in insufficient dose to combat the parasite [
18,
19]. Therefore, research on herbal medicine, immunotherapy, and new chemical compounds are needed in attempting to combat
T. evansi, which is expanding in Brazil [
17].
In vitro tests with human plasma showed trypanocidal effects on
T. evansi in different trials [
20]. This effect of human plasma on the parasites is attributed to the presence of APOL1, which according to researches, have trypanocidal action [
7]. Thus, APOL1 would be absorbed by the parasite by endocytosis, which triggers the formation of selective anions in the pores of the lysosomal membrane, which lead to induction of an uncontrolled proliferation and osmotic swelling of this compartment with subsequent cell death by lysis of trypanosome [
7,
8,
21]. Probably this was the mechanism by which the human plasma had an action of anti-trypanosome against
T. evansi, as well as trypanocidal activity of human plasma on
T. brucei [
8].
Tests in mice infected with
T. evansi showed differences between groups (plasma) to the longevity and therapeutic efficacy. Similar to other studies in rats and mice [
9,
10], the parasites disappear from circulation within 24 hr post-administration of treatment with plasma, and they had extended their longevity. However, when treatments were compared, animals of groups C (90%) and E (60%) left free of the parasite and longevity increased. By the other hand, all mice of group D had a recurrence of parasitemia and died of trypanosomosis. Since the volume of plasma administered was the same among groups, it is possible that the difference was due to the different amount of APOL1 in plasma of each man. This hypothesis has greater acceptance when the protein was quantified in samples of plasma and showed a great difference in concentration of APOL1. The highest concentrations of the protein were detected in plasma 1 (194 mg/dl) and 3 (115 mg/dl), exactly the samples which were more effective and curative for infected mice with
T. evansi (group C and E). The plasma 2, showed no curative effectiveness and had the lowest concentration of APOL1. This study emphasizes the fact that humans are refractory to
T. evansi, due to the presence of blood APOL1 [
8].
Besides APOL1 which is one of the 2 primate specific proteins, however, TLF-1 also contains haptoglobin (Hp)-related protein (Hpr), as well as apolipoprotein A-1 (APOA1) which are both directly and indirectly related to the toxicity to trypanosomes. Another related protein complex, TLF-2, although poorly characterized, is also likely to contribute to trypanosome killing [
22-
24].
Based on these results, we conclude that T. evansi is susceptible to treatment with human plasma in vivo. Treatment with human plasma prolongs the survival of mice infected with T. evansi, but the curative effectiveness differs according to the plasmas used. Probably this difference among groups is related to levels of APOL1 in plasma.
Committee of Ethics and Animal Welfare
The study was approved by the Animal Welfare, Federal University of Santa Maria (UFSM), no. 91/2009.
References
- 1. Silva RAMS, Seidl A, Ramirez L, Dávila AMR. Trypanosoma evansi e Trypanosoma vivax: biologia diagnóstico e controle. 2002, Corumbá. Embrapa Pantanal; p 166.
- 2. Lun ZR, Desser SS. Is the broad range of hosts and geographical distribution of Trypanosoma evansi attributable to the loss of maxicircle kinetoplast DNA? Parasitol Today 1995;11:131-133.
- 3. Hoare CA. The Trypanosomes of mammals: A zoological monograph. 1972, Oxford, UK. Blackwell Publ. Co; p 749.
- 4. Kubiak GVL, Molfi A. Tripanosomíase equina (Mal das Cadeiras). Boletim n.33. Instituto de Biologia e Pesquisas Tecnológicas do Estado do Paraná. 1954, Curitiba, Tip. João Haupt & Cia. Ltda; p 72.
- 5. Joshi PP, Shegokar VR, Powar RM, Herder S, Katti R, Salkar HR, Dani VS, Bhargava A, Jannin J, Truc P. Human trypanosomosis caused by Trypanosoma evansi in India: The first case report. Am J Trop Med Hyg 2005;73:491-495.
- 6. Shegokar VR, Powar RM, Joshi PP, Bhargava A, Dani VS, Katti R, Zare VR, Khanande VD, Jannin J, Truc P. Short report: Human trypanosomiasis caused by Trypanosoma evansi in a village in India: preliminary serologic survey of the local population. Am J Trop Med Hyg 2006;75:869-870.
- 7. Pérez-Morga D, Vanhollebeke B, Paturiaux-Hanocq F, Nolan DP, Lins L, Homblé F, Vanhamme L, Tebabi P, Pays A, Poelvoorde P, Jacquet A, Brasseur R, Pays E. Apolipoprotein L-I promotes trypanosome lysis by forming pores in lysosomal membranes. Science 2005;309:469-472.
- 8. Vanhollebeke B, Truc P, Poelvoorde P, Pays A, Joshi PP, Katti R, Jannin JG, Pays E. Human Trypanosoma evansi infection linked to a lack of apolipoprotein L-I. N Engl J Med 2006;355:2752-2756.
- 9. Otto MA, da Silva AS, Gressler LT, Farret MH, Tavares KC, Zanette RA, Miletti LC, Monteiro SG. Susceptibility of Trypanosoma evansi to human blood and plasma in infected mice. Vet Parasitol 2010;168:1-4.
- 10. Otto MA, da Silva AS, Gressler LT, Dall'Agnol LP, Bottam J, Zanette RA, Oliveira DC, Monteiro SG. Trypanosoma evansi: therapy with human plasma in infected rats. Comp Clin Pathol 2011;20:139-141.
- 11. Colpo CB, Colpo ETB, Stainki DR, Monteiro SG. Infecção Natural por Trypanosoma evansi em cão no Rio Grande do Sul. Ciência Rural 2005;35:717-719.
- 12. da Silva AS, Doyle RL, Monteiro SG. Método de contenção e confecção de esfregaço sanguíneo para pesquisa de hemoparasitas em ratos e camundongos. FZVA 2006;13:83-87.
- 13. Sambrook J, Fritsch EF, Maniatis T. Molecular cloning: a laboratory manual. 1989, Second edition. New York. Cold Spring Harbor Laboratory Press; p 300.
- 14. Ventura RM, Takeda GF, Silva RA, Nunes VL, Buck GA, Teixeira MM. Genetic relatedness among Trypanosoma evansi stocks by random amplification of polymorphic DNA and evaluation of a synapomorphic DNA fragment for species-specific diagnosis. Int J Parasitol 2002;32:53-63.
- 15. Tuntasuvan D, Jarabrum W, Viseshakul N, Mohkaew K, Borisutsuwan S, Theeraphan A, Kongkanjana N. Chemotherapy of surra in horses and mules with diminazene aceturate. Vet Parasitol 2003;110:227-233.
- 16. da Silva AS, Tochetto C, Zanette RA, Pierezan F, Rissi DR, Santurio JM, Monteiro SG. Aceturato de diminazeno e dipropionato de imidocarb no controle de infecção por Trypanosoma evansi em Rattus norvegicus infectados experimentalmente. Ciênc Rural 2008;38:1357-1362.
- 17. Da Silva AS, Andrade Neto OAS, Costa MM, Wolkmer P, Mazzanti CM, Santurio JM, Lopes STA, Monteiro SG. Tripanossomose em equinos na região sul do Brasil. Acta Sci Vet 2010;38:113-120.
- 18. Jennings FW, Whitelaw DD, Urquhart GM. The relationship between duration of infection with Trypanosoma brucei in mice and the efficacy of chemotherapy. Parasitology 1977;75:143-153.
- 19. Spinosa HS, Górniak SL, Bernardi MM. Farmacologia aplicada à medicina veterinária. 1999, Rio de Janeiro. Guanabara koogan; p 946.
- 20. Lai DH, Wang QP, Li Z, Luckins AG, Reid SA, Lun ZR. Investigations into human serum sensitivity expressed by stocks of Trypanosoma brucei evansi. Int J Parasitol 2010;40:705-710.
- 21. Pays E, Vanhollebeke B, Vanhamme L, Paturiaux-Hanocq F, Nolan DP, Pérez-Morga D. The trypanolytic factor of human serum. Nat Rev Microbiol 2006;4:477-486.
- 22. Rifkin MR. Identification of the trypanocidal factor in normal human serum: high density lipoprotein. Proc Natl Acad Sci USA 1978;75:3450-3454.
- 23. Hajduk SL, Moore DR, Vasudevacharya J, Siqueira H, Torri AF, Tytler EM, Esko JD. Lysis of Trypanosoma brucei by a toxic subspecies of human high density lipoprotein. J Biol Chem 1989;264:5210-5217.
- 24. Raper J, Fung R, Ghiso J, Nussenzweig V, Tomlinson S. Characterization of a novel trypanosome lytic factor from human serum. Infect Immun 1999;67:1910-1916.
Fig. 1Diagnosis of Trypanosoma evansi in blood samples of a mice experimentally infected and treated with human plasma, using the PCR. (MP) 100 pb ladder (Ludwig Biotec®); (1-9) blood samples of group C post-treatment; (10-15) blood samples of group E post-treatment. (CN) negative control and (CP) positive control for T. evansi-315 pb.

Table 1.Media and standard deviation of the pre-patent period, longevity, mortality and success of therapy using treatment with human plasma in mice experimentally infected with T. evansi
Table 1.
|
Groups (n = 10) |
Treatment |
Pre-patent period |
Longevity |
Mortality |
Success of therapy (%)a
|
|
A |
Negative control |
- |
41.0a (± 0.0) |
0/10 |
- |
|
B |
Positive control |
1.9a (± 0.3) |
4.3 (± 0.5) |
10/10 |
- |
|
C |
T2 |
1.9a (± 0.3) |
40.9a (± 0.3) |
1/10 |
90.0 |
|
D |
T3 |
1.6a (± 0.4) |
20.0 (± 9.0) |
10/10 |
0.0 |
|
E |
T4 |
1.4a (± 0.5) |
35.6a (± 9.3) |
4/10 |
60.0 |