Abstract
In Iran, Plasmodium vivax is responsible for more than 80% of the infected cases of malaria per year. Control interventions for vivax malaria in humans rely mainly on developed diagnostic methods. Recombinant P. vivax apical membrane antigen-1 (rPvAMA-1) has been reported to achieve designing rapid, sensitive, and specific molecular diagnosis. This study aimed to perform isolation and expression of a rPvAMA-1, derived from Iranian patients residing in an endemic area. Then, the diagnostic efficiency of the characterized Iranian PvAMA-1 was assessed using an indirect ELISA method. For this purpose, a partial region of AMA-1 gene was amplified, cloned, and expressed in pET32a plasmid. The recombinant His-tagged protein was purified and used to coat the ELISA plate. Antibody detection was assessed by indirect ELISA using rPvAMA-1. The validity of the ELISA method for detection of anti-P. vivax antibodies in the field was compared to light microscopy on 84 confirmed P. vivax patients and compared to 84 non-P. vivax infected individuals. The ELISA cut-off value was calculated as the mean+2SD of OD values of the people living in malaria endemic areas from a south part of Iran. We found a cut-off point of OD=0.311 that showed the best correlation between the sera confirmed with P. vivax infection and healthy control sera. A sensitivity of 81.0% and specificity of 84.5% were found at this cut off titer. A good degree of statistical agreement was found between ELISA using rPvAMA-1 and light microscopy (0.827) by Kappa analysis.
-
Key words: Plasmodium vivax, AMA-1, recombinant antigen, ELISA, microscopy, Iran
INTRODUCTION
Malaria still remains as a problem for a high proportion of population in the world. The infection is responsible for about 1-2 million deaths per annum [
1] and more than 40% of the population are living in areas where malaria is endemic [
2]. It was estimated that nearly 1 billion people are exposed to malaria in hypoendemic and mesoendemic areas in southeast Asia [
3]. Although
Plasmodium falciparum shows a high mortality rate,
Plasmodium vivax malaria has a wider geographical distribution and represents the most widespread malaria parasite worldwide.
P. vivax is responsible for approximately 80 million malaria-infected cases annually [
4]. In Iran,
P. vivax is responsible for more than 80% of the infected cases per year. In recent years, Iran has been engaged with malaria control programs. With these efforts, the total malaria reported cases in Iran from 96,340 with about 55%
P. vivax in 1991 decreased to 18,966 with 88%
P. vivax in 2005, and during these years
P. vivax has been highly prevalent in the country [
5]. Contemporaneous population movement of Afghani and Pakistani refugees from endemic areas toward to the south and southeast of Iran changes the numbers of population living in the areas of malaria risk. So, we need new information about endemicity of malaria in areas where malaria has been endemic.
It is therefore important to recognize and assess the potentiality of immunodominant
P. vivax diagnostic antigens. This idea implies that the proteins bear such capacity to sensitize the immune system to produce specific antibodies [
6,
7]. The specific antibodies to the blood stages can be detected and rise to high levels during couple of days following clinical signs that are simultaneous to the emergence of parasites in the patient's blood and remain for months and rarely years, and then decline to inactive levels [
8]. Assessment of these antibodies in serological studies are generally recognized valuable to supplement parasitological data as well as transmission and immunity of malaria [
9]. Apical membrane antigen-1 (AMA-1) is a micronemal protein of apicomplexan parasites to be found on the apical organelles of merozoites that performs significant roles during the attack of host cells. After natural infection, PvAMA-1 stimulates immune responses, and the produced antibodies can have profound parasite-inhibitory effects and can be detected in human sera by using an appropriate antigen [
10].
In general, malarial parasite antigens could be obtained from parasite cultivation [
11], but
P. vivax is particularly considered as a non-cultivable parasite. In earlier studies, ELISA and indirect fluorescence methods were used to measure antibody assessment for epidemiological studies of malaria, and the antigens for established ELISA tests were achieved from
Aotus monkey. Therefore, in this study, we performed isolation and expression of a rPvAMA-1, derived from Iranian patients residing in an endemic area. Then, the diagnostic efficiency of the characterized Iranian PvAMA-1 was assessed using an ELISA method.
MATERIALS AND METHODS
Study area
The sera were collected from malaria endemic areas of Iran. These parts are located in the south-east of the country, bordered in the north coast of the Persian Gulf and Oman Sea and to the east by Pakistan and Afghanistan. These parts include the provinces of Hormozgan and Sistan & Baluchestan. Hormozgan has hot and humid weather in most months of the year, and the annual average rainfall was calculated as 196 mm. Sistan & Baluchestan has hot and dry weather for 9 months and the annual average rainfall was calculated as 65 mm.
Serum collection and microscopic examinations
A total of 168 serum samples were collected for serological analysis by venipuncture of patients. Total 84 serum samples were obtained from patients who were resident in malaria endemic regions in Iran with symptomatic P. vivax malaria confirmed by detecting parasites in thick and thin blood films using Giemsa stain. Negative controls, including 79 samples were from healthy individuals as well as 9 samples from patients infected with Toxoplasma, Leishmania infantum, and FUO (fever of unknown origin) who had never exposed to malaria, and finally 3 sera from infected patients with P. falciparum. Moreover, 60 normal sera were collected to define a cut off value; these subjects were residents in malaria endemic areas but in healthy situation. Serum samples were collected after receiving informed consent by all individuals during the period from 2009 to September 2010. The sera were frozen at -70℃ until used.
Preparation of rPvAMA-1 antigen
Parasite DNA extraction
The genomic DNA was purified from the infected erythrocytes of a patient with vivax malaria, using Genomic DNA Extraction Kit, ACCUPreP® kit (BIONEER, Incheon, Korea) according to the manufacturer's instructions. The extracted DNA was checked by biophotometer and used as the template for PCR with primers corresponding to the AMA-1 region as will be mentioned below.
Cloning and expression of PvAMA-1 in Escherichia coli
The nucleotide sequence corresponding to amino acid (AA) residues 43-487 of PvAMA-1, involving the internal regions (domain I, domain II and domain III) of the PvAMA-1 gene, was obtained by PCR amplification using the following set of primers PvAMAF 5'-CCATGGGGCCTACCGTTGAGAGAA-3' and PvAMAR 5'-CTCGAGTCATAGTAGCATCTGCTTGTT-3'. This pair of primers was designed regarding the P. vivax Sal-1 AMA-1 (GenBank ID: XM_001615397). These primers contained restriction enzyme sites for cloning and expression in the prokaryotic host. PCR was performed as same as described elsewhere (Motevalli et al. in press). The PCR product was purified from an agarose gel using Qiaquick GEL Extraction kit (QIAGEN, Hilden, Germany) and cloned in pUC19 cloning vector using Rapid DNA ligation kit (Roche, Mannheim, Germany). The resulted recombinant plasmid was transformed into E. coli Novablue by heat shock. The transformants were plated on LB agar medium, containing ampicillin (100 µg/ml), IPTG (1 mM), and X-gal (50 µg/ml) for blue-white selection. A single white colony was picked and cultured in LB medium with ampicillin (100 µg/ml) at 37℃ with shaking (160 rpm) for 3 hr, and verification of cloning was carried out by PCR. Then, the recombinant pUC19 plasmid was purified by the High pure plasmid purification kit (Roche) and was cut by NcoI and XhoI to subclone in the pET32a as a bacterial expression vector. The recombinant pET32a-AMA-1 was transformed into E. coli Novablue as described previously, then it was purified and sent for sequencing. Transformation of E. coli BL-21(DE3) expression host cells was then carried out using a purified and verified recombinant plasmid. A single positive clone was considered for AMA-1 expression, it was cultured in LB medium containing 100 µg/ml ampicillin at 37℃ with shaking for 3 hr to reach OD 0.4, then 1 mM of IPTG as a gene expression inducer was added to the culture and the culture was continued for another 3 hr. After incubation, the culture was centrifuged and the cell mass resuspended in sonication buffer (50 mM Tris-HCl, pH 8.0, 100 mM NaCl, 1 mM EDTA, 50 mM phenylmethylsulfonyl floride [PMSF] and 80 mg/ml of lysozyme) and was lysed during 6 sonication cycles consisting of 10 sec burst at high intensity and 10 sec cooling period on ice. Then, the bacterial lysate was centrifuged at 6,500 g for 30 min at 4℃ to remove bacterial debris, and the supernatant was applied to confirm the expression by SDS-PAGE. Gel was stained with coomassie blue.
Purification of rPvAMA-1
The recombinant His-tagged protein was purified from the supernatant of the bacterial lysate by Nickel-Chelating Resin column using the ProBond purification system kit (Invitrogen, Carlsbad, California, USA) in native conditions according to the manufacturer's protocol. The resulting protein was analyzed on 12% SDS-PAGE, calculated by Bradford assay (Bio-Rad, Hercules, California, USA) and used for ELISA.
Design and assessment of an indirect ELISA method by using rPvAMA-1
Antigen coating and optimization and test sera dilutions
A checkerboard ELISA was performed to determine the working concentrations of the coating antigen and antibody to assess present malaria antibodies in suspect sera. Antigen and antibody titration was done as follows: rPvAMA-1 was titerated, using a checkerboard titration in which flat bottom plates were coated with 100 µl of rPvAMA-1 serially diluted starting from the initial protein concentration of 20 µg/ml in sodium carbonate buffer, pH 9.6 (coating buffer) per well and incubated in a humid chamber at 4℃ overnight. The wells were washed 3 times with PBS-Tween 20 (PBS-T).
Test procedure
Antigenicity studies were carried out using human serum samples from residents of a malaria-endemic area in south of Iran. ELISA was performed using rPvAMA-1 coated onto ELISA plates to detect antigen-specific antibodies. Determination of anti-PvAMA-1 antibodies was done based on binding of this antibody (present in the serum sample) to rPvAMA-1 antigen coated on ELISA plates (Nunc, Roskilde, Denmark) and finally to evaluate the sensitivity and specificity of the test, ELISA was performed on the 168 collected sera as described previously. The assay of 60 collected sera was carried out to define cut off to separate positive from negative sera in the study population.
To each previously coated well, known positive and negative sera diluted to 1:10, 1:40, 1:80, and 1:160 in PBS-T were added, respectively. Plates were incubated in a humid chamber at room temperature for 1 hr and then were washed with PBS-T 3 times. To assess the binding of antibody to rPvAMA-1 antigen coated wells, 100 µl of 1:1,000 dilution of polyclonal anti-human IgG alkaline phosphatase conjugated (DakoCytomation, Produktionsvej, Denmark) was added to the plates which were then incubated for 1 hr in a humid chamber at room temperature and finally washed 3 times with PBS-T. A 100 µl of substrate solution PNP (Sigma, St. Louis, Illinois, USA) in DiEthanolamine was added to each well, and the colour permitted to develop at room temperature for 20 min in a dark place. The reaction was stopped by adding of 50 µl 3N NaOH. The optical density (OD) of the samples was measured at 405 nm using a Titerteck (Helsinki, Finland) multiscan ELISA plate reader. All assays were tested in duplicate. Finally, the best concentrations of antigen and antibody were determined and the designed ELISA was applied to assess present antibodies in natural infections.
Statistical analysis
The cut-off value was calculated as the mean+2SD of OD value of the healthy group sera living in a malaria endemic area. Accordingly, OD values higher than mean+2SD were considered positive. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and diagnostic efficiency of ELISA compared to microscopy for detection of P. vivax infection were calculated with the following formula:
Sensitivity=TP/(TP+FN)×100%, specificity=TN/(TN+FP)×100%, positive predictive value (PPV)=TP/(TP+FP)×100%, negative predictive value (NPV)=TN/(TN+FN)×100%, Diagnostic efficiency=(TN+TP)/Total×100% where TP represents the true positive, TN true negative, FN false negative, and FP false positive.
The degree of agreement between ELISA and the microscopy was determined by calculating kappa (κ) values with 95% confidence intervals, using the Epi-Info software. Kappa values express the agreement beyond change, and a 'κ' value of 0.21-0.60 represents a fair to moderate agreement, 0.60-0.80 represents a substantial agreement, and >0.80 represents almost perfect agreement [
12,
13]. A probability value of
P<0.05 was considered statistically significant.
RESULTS
Cloning and expression of the PvAMA-1 gene
A 1,300 bp PCR product corresponding to the AMA-1 region was successfully cloned in pUC19. The subcloning was performed in pET32a and confirmed by sequencing (GenBank ID: HM535663.1). The rPvAMA-1 expression was detected on SDS-PAGE and purified successfully.
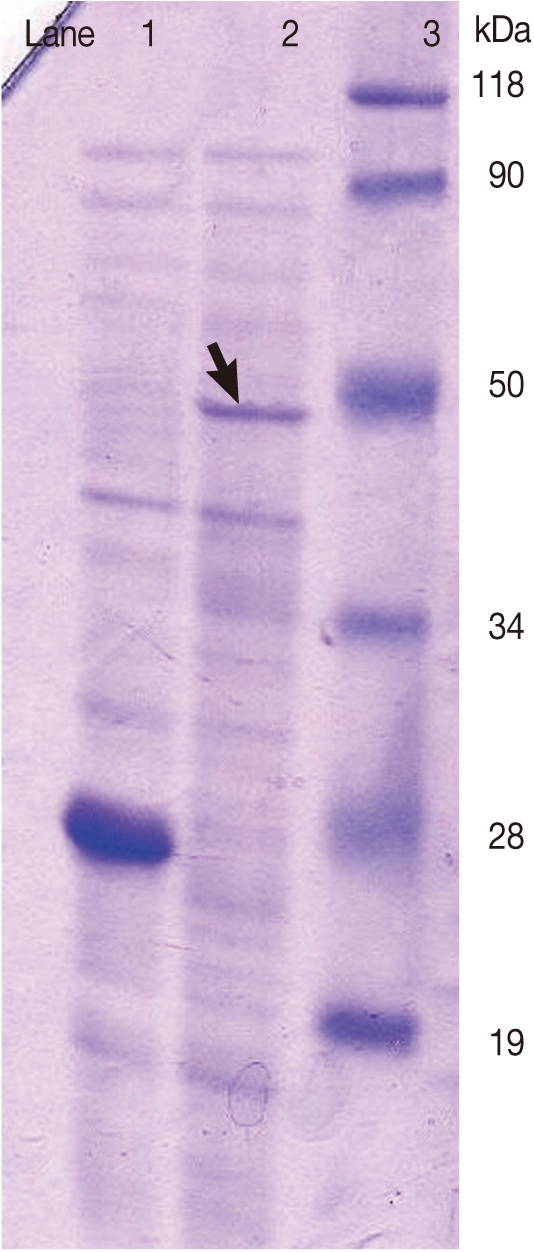
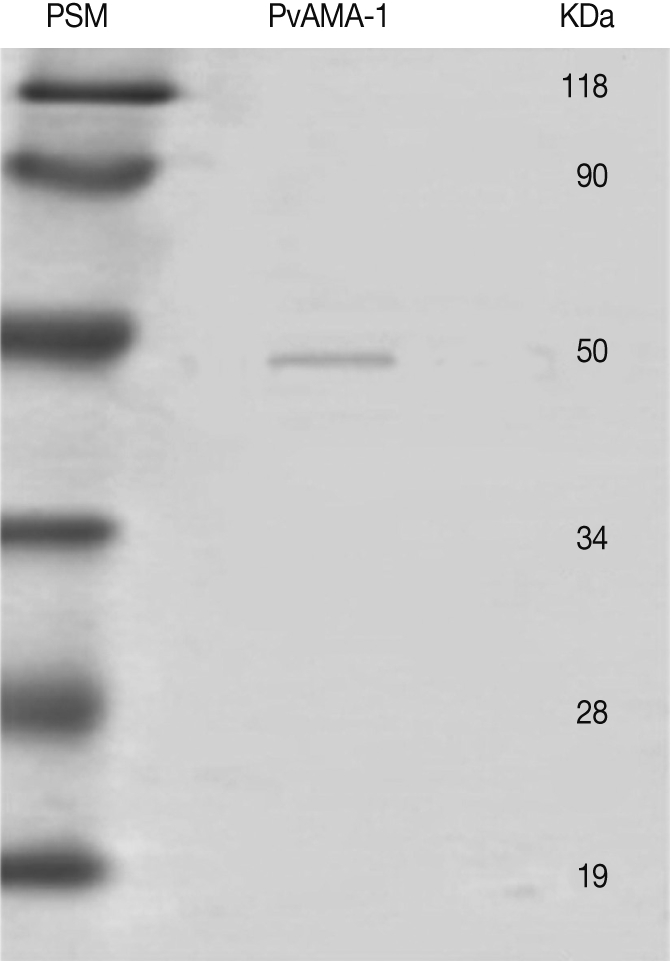
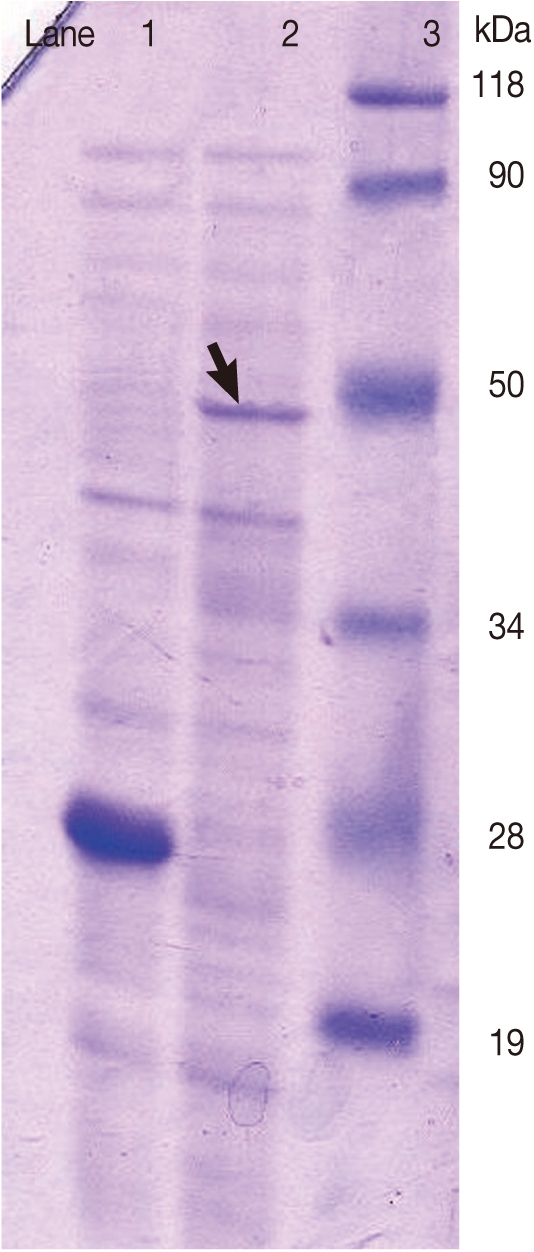
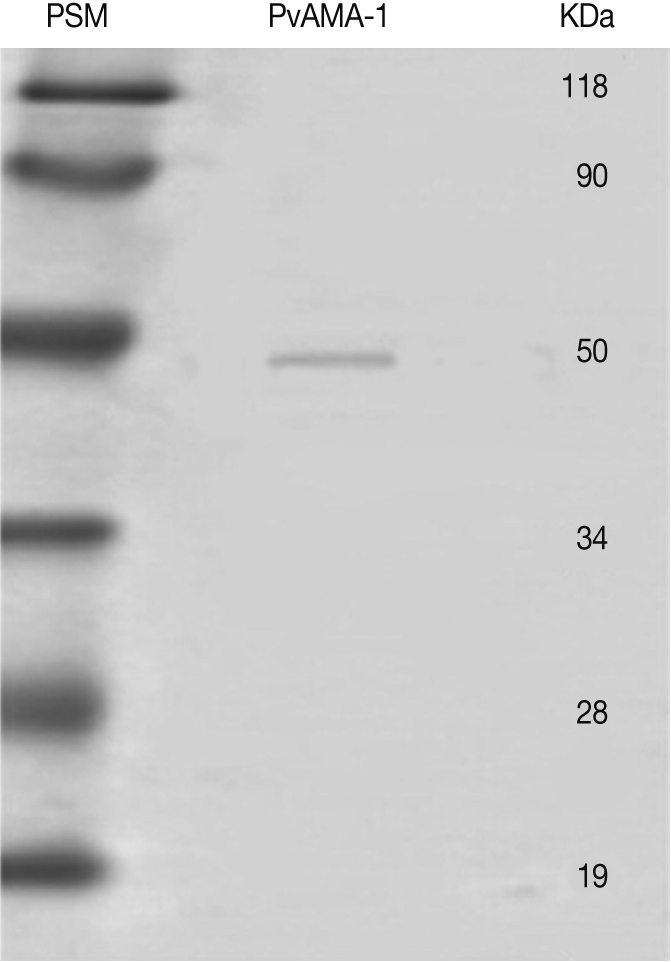
Fig. 1 shows the SDS-PAGE analysis for rPvAMA-1 production. Analysis of the purified rPvAMA-1 by SDS-PAGE showed a molecular weight of 50 kDa (
Fig. 2), and the concentration of the eluted protein was calculated as 189.2 µg/ml by the Bradford assay.
Based on the results from the checkerboard test, the best concentration for antigen was defined as 2.36 µg of rPvAMA-1/ml of sodium carbonate buffer, pH 9.6 in each well, and the best dilution to detect malaria antibody was determined as 1/80 dilution. So, in order to attach all specific antibodies to the antigen, all tested sera were diluted at an optimal dilution of 1/80 and added to the ELISA plates coated with rPvAMA-1. Human antibodies against PvAMA-1 were detected by an indirect ELISA. The highest dilution that made an absorbance value over the highest absorbance of the negative control was considered as the best point titer to assess present antibodies in sera. The cut off point for rPvAMA-1 was calculated as OD 0.311.
Assay of clinical sensitivity of ELISA
As shown in
Table 1, ELISA test showed 81.0% clinical sensitivity for patients with proven malaria vivax infection.
The results indicated that a total of 15.5% of the 84 subjects reacted with rPvAMA-1. The specificity was then determined as 84.5%. Although the rPvAMA-1 showed reactivity with 3 samples from P. falciparum sera but no cross reaction was observed with other samples collected from other diseases.
Diagnostic value of indirect ELISA
Table 2 gives determination of the sensitivity, specificity, PPV, NPV provided, and the diagnostic efficiency of anti-PvAMA-1 antibody using indirect ELISA.
DISCUSSION
Vivax malaria is considered as a highly prevalent infection with a global geographic distribution. It is extremely a prerequisite to find immunological antigens of malaria parasites causing natural immune responses to design a suitable diagnostic method [
14]. However, the difficulty of vivax malaria in vitro cultivation to isolate candidate immunodiagnostic antigens, makes it difficult to perform. Several recombinant constructs obtained from asexual blood-stages of parasites have been recognized as potential antigenic candidates, and studies on human sera from patients infected with
Plasmodium have shown antibody titers to them [
15-
18]. Studies have also addressed the potential use of rPvAMA-1 as a potential malaria antigen for diagnosis [
19,
20]. AMA-1 is a unique protein of
Plasmodium that has been well-characterized and its function can be blocked by antibodies [
21,
22]. Moreover, the protein corresponding to the sequence of
P. vivax AMA-1 is strongly immunogenic to humans exposed to natural infections [
10,
23]. The rationale of the present study was to identify the human naturally acquired immune responses to rPvAMA-1 representing the 3 domains of PvAMA-1 in Iran. In the current work, a recombinant plasmid, pET32a-AMA-1, was constructed and the related protein was used as a coated antigen in ELISA plates. Our results provided a suitable expression vector with a potential power to express the AMA gene in prokaryotic cells, and therefore, it will be easily accessible to prepare related recombinant protein in large amount in the future. This product could be used to investigate about vaccination as well as to establish a diagnostic method to conduct epidemiological studies.
Recognition of the rPvAMA-1 was then assessed by detection of circulating natural antibodies using
P. vivax-infected sera collected from endemic regions in Iran. A total of 81.0% of the individuals showed antibodies to this recombinant antigen, showing relatively high frequency of reacting sera from individuals with patent
P. vivax infection to rPvAMA-1 antigen. Serum antibody responses to rPvAMA-1 in different areas of Brazil, Sri Lanka, and Korea [
10,
23,
24] have been reported. In a study from Brazil [
10], antibody assay using ELISA test has demonstrated 85.0% (for IgG) and 48.5% (for IgM) sensitivity, respectively. The test was based on an antibody assay against rPvAMA-1 corresponding 3 domains of PvAMA-1in individuals infected with
P. vivax malaria. Kim et al. [
24] showed that the ELISA test based on multiple proteins of blood stages has resulted in 80.3% sensitivity with serum samples. While only 46.1% of sera reacted with rPvAMA-1, Wickramarachchi et al. [
23] reported that cytophilic antibodies against 3 domains of PvAMA-1 were more obvious when residents in endemic areas stayed more exposures to infection. There is no previous report on anti-PvAMA-1 antibodies in Iran, but Mehrizi et al. [
25] described higher immune responses of PvMSP-1. The antibodies to PvMSP-1 were detected in 86.1% in serum samples from patient with patent P.vivax infection.
However, rPvAMA-1 could be applied as an immunodominant antigen for the diagnosis vivax malaria. In a separate assessment, the results of ELISA were compared with those of IFA. The frequencies of individuals who responded to a recombinant protein derived from PvAMA-1in ELISA were significantly higher than the frequency of responders to IFAT using a conventional intact whole parasite antigen. The percentage of P. vivax samples which reacted with IFA was 36%, while ELISA antibody test showed more than 2 times highly sensitive as IFA test.
In our study, the rPvAMA-1 reacted with 3 samples from
P. falciparum. This seemingly cross-reactivity can be explained either by possible previous infection with
P. vivax because of the residential situation of the residents in the endemic areas, or by dominancy of
P. falciparum AMA-1 according to previous reports explaining that PfAMA-1 is highly immunogenic for the most individuals who exposed to
P. falciparum infection against
P. vivax [
26]. In either explanation, this implies that AMA-1 is an extremely immunogenic molecule during natural
Plasmodium infection.
There exists an old report done by Eddrissian and others in 1979 in Iran, who employed an ELISA test to detect infections in human sera. As they reported, natural antibodies were detected with Aotus monkey-derived P. falciparum and P. fieldi malaria antigens for ELISA. Anti-malaria antibodies were detected in titers ≥1/40 in 24.3% and 34.9% residents from villages in Bandar Abbas and Minab areas of southern Iran, respectively. They also reported that IFA showed higher positivity rate than ELISA.
The presence of antibodies in sera from humans infected with
P. vivax that recognized the recombinant protein related to the partial region of PvAMA-1 indicated that the expression systems successfully rebuilt domains conformation relating to cysteine residues and epitopes resembling the native PvAMA-1 that induce natural immunity in patients. These residues remained as the natural protein expressed in blood stage form of parasites [
27,
28]. It is accordingly suggested that multiple proteins should be constructed and used to evaluate humoral immunity in cases of vivax malaria, because the complexity of immunity occurs in patients and the sensitivity of a multiple antigens are considered more convincing [
29].
Our results showed that there is reasonable agreement in the results between microscopy, as a standard method, and ELISA using rPvAMA-1 for detection of P. vivax infection.
ACKNOWLEDGMENTS
The authors would like to thank Dr. Sabouri and Dr. Hajjaran for their precious collaboration. This study (grant number 88-04-27-9255) was financially supported by the School of Public Health, Tehran University of Medical Sciences (TUMS), Tehran, Iran. The authors declare that they have no conflict of interests.
References
- 1. Snow RW, Guerra CA, Noor AM, Myint HY, Hay SI. The global distribution of clinical episodes of Plasmodium falciparum malaria. Nature 2005;434:214-217.
- 2. Greenwood B, Mutabingwa T. Malaria in 2002. Nature 2002;415:670-672.
- 3. Hay SI, Guerra CA, Tatem AJ, Noor AM, Snow RW. The global distribution and population at risk of malaria: Past, present, and future. Lancet Infect Dis 2004;4:327-336.
- 4. Mendis K, Sina BJ, Marchesini P, Carter R. The neglected burden of Plasmodium vivax malaria. Am J Trop Med Hyg 2001;64(1-2 suppl):97-106.
- 5. Edrissian GH. Malaria in Iran: past and present situation. Iranian J Parasitol 2006;1:1-14.
- 6. Soler E, Houdebine LM. Preparation of recombinant vaccines. Biotechnol Annu Rev 2007;13:65-94.
- 7. Giraldo MA, Arevalo-Pinzon G, Rojas-Caraballo J, Mongui A, Rodriguez R, Patarroyo MA. Vaccination with recombinant Plasmodium vivax MSP-10 formulated in different adjuvants induces strong immunogenicity but no protection. Vaccine 2009;28:7-13.
- 8. Voller A, Meuwissen JHE, Verhave H. In Kreier JP ed, Methods of measuring the immunological response to Plasmodia. Immunology and Immunisation. Malaria. 1980, Vol. 3. New York, USA. Academic Press; pp 67-109.
- 9. Voller A, Huldt G, Thors C, Engvall E. New serological test for malaria antibodies. Br Med J 1975;1:659-661.
- 10. Rodrigues MH, Rodrigues KM, Oliveira TR, Cômodo AN, Rodrigues MM, Kocken CH, Thomas AW, Soares IS. Antibody response of naturally infected individuals to recombinant Plasmodium vivax apical membrane antigen-1. Int J Parasitol 2005;35:185-192.
- 11. Serological testing in malaria. Bull World Health Organ 1974;50:527-535.
- 12. Altman DG. Practical statistics for medical research. 2001, London, UK. Chapman & Hall.
- 13. Babakhan L, Mohebali M, Akhoundi B, Edrissian GH, Keshavarz H. Rapid detection of Leishmania infantum infection in dogs: A comparative study using fast agglutination screening test (FAST) and direct agglutination test (DAT) in Iran. Parasitol Res 2009;105:717-720.
- 14. James S, Miller L. Malaria vaccine development: Status report. Nature Med Suppl 2000.
- 15. Vekemans J, Ballou WR. Plasmodium falciparum malaria vaccines in development. Expert Rev Vaccines 2008;7:223-240.
- 16. Morais CG, Soares IS, Carvalho LH, Fontes CJ, Krettli AU, Braga EM. Antibodies to Plasmodium vivax apical membrane antigen 1: Persistence and correlation with malaria transmission intensity. Am J Trop Med Hyg 2006;75:582-587.
- 17. Mahanty S, Saul A, Miller LH. Progress in the development of recombinant and synthetic blood-stage malaria vaccines. J Exp Biol 2003;206(Pt 21):3781-3788.
- 18. Herrera S, Corradin G, Arévalo-Herrera M. An update on the search for a Plasmodium vivax vaccine. Trends Parasitol 2007;23:122-128.
- 19. Bueno LL, Morais CG, Soares IS, Bouillet LE, Bruna-Romero O, Fontes CJ, Fujiwara RT, Braga EM. Plasmodium vivax recombinant vaccine candidate AMA-1 plays an important role in adaptive immune response eliciting differentiation of dendritic cells. Vaccine 2009;27:5581-5588.
- 20. Remarque EJ, Faber BW, Kocken CH, Thomas AW. Apical membrane antigen 1: A malaria vaccine candidate in review. Trends Parasitol 2008;24:74-84.
- 21. Thomas AW, Deans JA, Mitchell GH, Alderson T, Cohen S. The Fab fragments of monoclonal IgG to a merozoite surface antigen inhibit Plasmodium knowlesi invasion of erythrocytes. Mol Biochem Parasitol 1984;13:187-199.
- 22. Deans JA, Alderson T, Thomas AW, Mitchell GH, Lennox ES, Cohen S. Rat monoclonal antibodies which inhibit the in vitro multiplication of Plasmodium knowlesi. Clin Exp Immunol 1982;49:297-309.
- 23. Wickramarachchi T, Premaratne PH, Perera KL, Bandara S, Kocken CH, Thomas AW, Handunnetti SM, Udagama-Randeniya PV. Natural human antibody responses to Plasmodium vivax apical membrane antigen 1 under low transmission and unstable malaria conditions in Sri Lanka. Infect Immun 2006;74:798-801.
- 24. Kim S, Ahn HJ, Kim TS, Nam HW. ELISA detection of vivax malaria with recombinant multiple stage-specific antigens and its application to survey of residents in endemic areas. Korean J Parasitol 2003;41:203-207.
- 25. Mehrizi AA, Zakeri S, Salmanian AH, Sanati MH, Djadid ND. IgG subclasses pattern and high-avidity antibody to the C-terminal region of merozoite surface protein 1 of Plasmodium vivax in an unstable hypoendemic region in Iran. Acta Trop 2009;112:1-7.
- 26. Thomas AW, Trape JF, Rogier C, Goncalves A, Rosario VE, Narum DL. High prevalence of natural antibodies against Plasmodium falciparum 83-kilodalton apical membrane antigen (PF83/AMA-1) as detected by capture-enzyme-linked immunosorbent assay using full-length baculovirus recombinant PF83/AMA-1. Am J Trop Med Hyg 1994;51:730-740.
- 27. Nair M, Hinds MG, Coley AM, Hodder AN, Foley M, Anders RF, Norton RS. Structure of domain III of the blood-stage malaria vaccine candidate, Plasmodium falciparum apical membrane antigen 1 (AMA1). J Mol Biol 2002;322:741-753.
- 28. Holder AA. In Hoffman SL ed, Preventing merozoite invasion of erythrocytes. Malaria vaccine development: A multi-immune response approach. 1996, Washington DC, USA. American Society of Microbiology; pp 77-104.
- 29. Krotoski WA. Discovery of the hypnozoite and a new theory of malarial relapse. Trans R Soc Trop Med Hyg 1985;79:1-11.
Fig. 1SDS-PAGE analysis for rPvAMA-1 production. Lane 1: E. coli BL21(DE 3) bacterial lysate containing pET 32 a plasmid (negative control). Lane 2: E. coli BL21(DE 3) bacterial lysate containing pET 32 a-AMA-1 recombinant plasmid. Lane 3: Protein size marker.
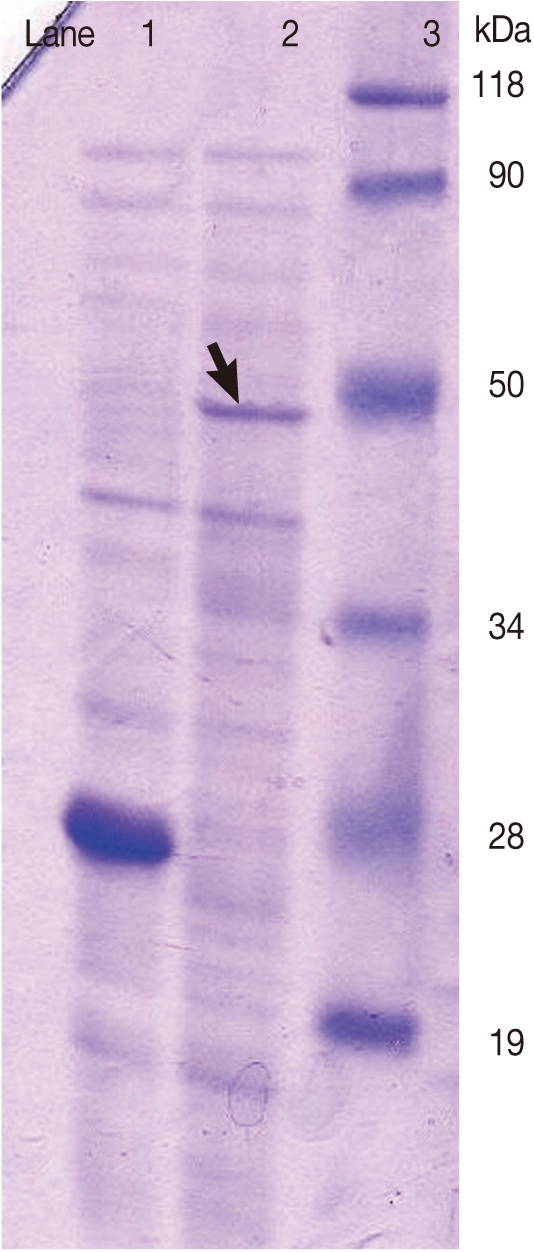
Fig. 2SDS-PAGE analysis of rPvAMA-1 expression. PSM: protein size marker (kDa). PvAMA-1: His tagged recombinant antigen purified by Ni-NTA affinity column after IPTG induction.
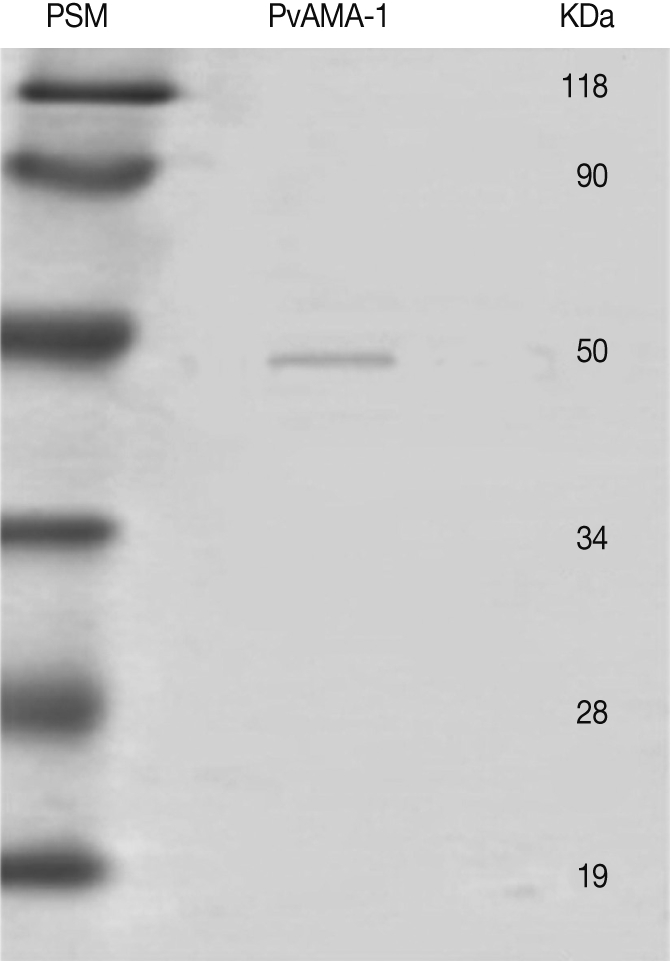
Table 1.Comparison between ELISA using recombinant protein PvAMA-1 (cut-off=0.311) and microscopy results
Table 1.
|
ELISAa+
|
ELISA-
|
Total
|
|
No. (%) |
No. (%) |
No. (%) |
|
Microscopy (positive) |
68 (81.0) |
16 (19.1) |
84 (100.0) |
|
Microscopy (negative) |
13 (15.5) |
71 (84.5) |
84 (100.0) |
|
Total |
81 (48.2) |
87 (51.8) |
168 (100.0) |
Table 2.Diagnostic performance of anti-PvAMA-1 indirect ELISA assay
Table 2.
|
Assay |
Sensitivity (%) |
Specificity (%) |
PPV (%) |
NPV (%) |
Diagnostic efficiency |
|
ELISA |
81.0 |
84.5 |
84.0 |
80.7 |
82.7 |