Abstract
The 5th outbreak of trichinosis occurred in a mountainous area of North Vietnam in 2012, involving 24 patients among 27 people who consumed raw pork together. Six of these patients visited several hospitals in Hanoi for treatment. Similar clinical symptoms appeared in these patients within 5-8 days after eating infected raw pork, which consisted of fever, muscle pain, difficult moving, edema, difficult swallowing, and difficult breathing. ELISA revealed all (6/6) positive reactions against Trichinella spiralis antigen and all cases showed positive biopsy results for Trichinella sp. larvae in the muscle. The larvae detected in the patients were identified as T. spiralis (Vietnamese strain) by the molecular analysis of the mitochondrial cytochrome c oxidase subunit III (cox3) gene.
-
Key words: Trichinella spiralis, muscle pain, pork, fever, ELISA, Vietnam
INTRODUCTION
Trichinella spiralis adult worms parasitize the intestine and their larvae encyst in muscles of humans and animals [
1-
4]. In Asia,
Trichinella spp. infection has been documented in humans in 18 countries, in domestic animals (mainly pigs) in 9 countries, and in wildlife in 14 countries [
5,
6]. Molecular identification of
Trichinella papuae was reported in Thailand [
3] and
T. spiralis in Korea [
7], but no reports have been available in Vietnam.
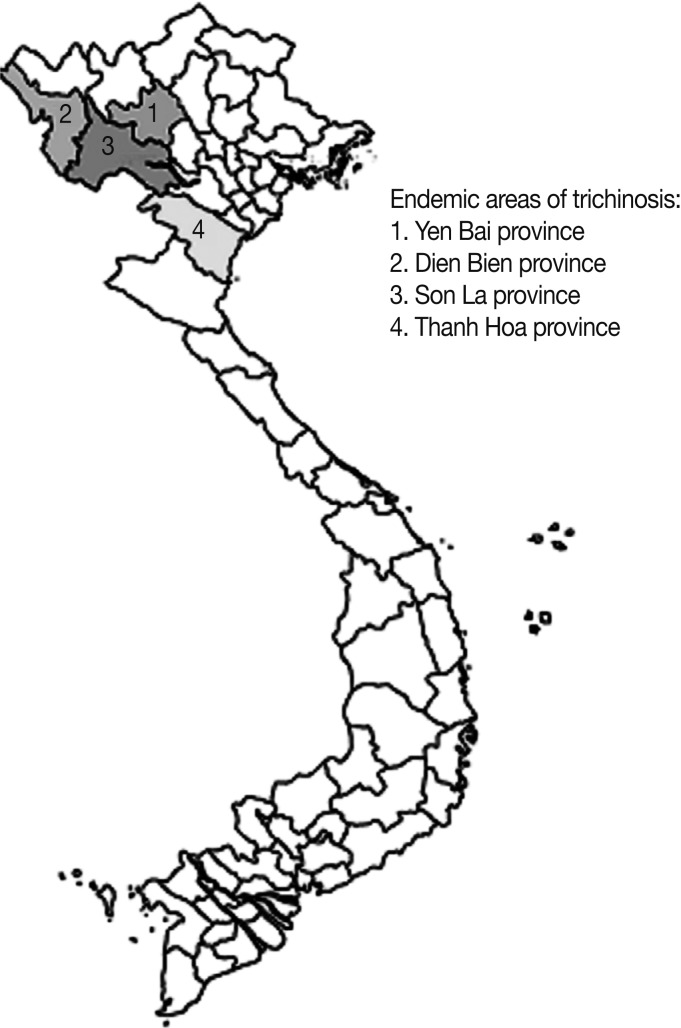
In Vietnam, the first outbreak of trichinosis was reported in 1970 in a mountainous area of Yen Bai province with 26 patients by eating raw pork in a wedding-party and 4 of them died [
2]. The second outbreak occurred in 2001 in a mountainous commune in Dien Bien province with 22 patients who ate raw pork in a wedding-party also and 2 of them died [
2]. The third outbreak was also in Dien Bien province in 2004 with 20 patients by eating raw pork in a funeral party [
2]. The fourth outbreak occurred in a mountainous area of Son La province in 2008 [
8]. In this outbreak, 22 patients were involved after eating raw pork in a wedding-party from 1 pig together, and 2 of them died. The fifth outbreak occurred in February 2012 in a mountainous area of Thanh Hoa province involving 24 patients who ate raw pork in a lunar New Year party (6 of them are reported in this paper) (
Fig. 1). However, additional reports are needed to provide better understanding of the molecular and genetic characteristics of the Vietnamese
Trichinella species.
CASE RECORD
In February 2012, 24 of 27 people, who ate raw pork together in a lunar Year party in Muong Lat district, Thanh Hoa province, Vietnam, were proved as trichinosis patients by ELISA test using T. spiralis antigen. They all revealed similar clinical symptoms, i.e., fever and muscle pain, and were treated with albendazole 800 mg/day for 10 days. Among them, 6 patients visited hospitals in Hanoi, Vietnam, and their clinical histories were obtained as follows.
The 6 patients included 3 men and 3 women between 30 and 43 years of age. The clinical symptoms included fever in 6 of 6 patients, muscular pain in 6 of 6 patients, difficult moving in 6 of 6 patients, edema in the leg/hand in 6 of 6 patients, edema around the eyes in 6 of 6 patients, difficult swallowing in 6 of 6 patients, loss of weight in 5 of 6 patients, difficulty in breathing in 5 of 6 patients, itching in 3 of 6 patients, and diarrhea in 1 of 6 patients (
Table 1). Laboratory findings in these patients included eosinophilia in 5 of 6 patients from 18.5% to 51.8%; increased transaminase for AST in 6 of 6 patients in the range 65-219 U/L (normal values ≤37 U/L in man and ≤31 U/L in woman) and for ALT in 6 of 6 patients in the range 74-471 U/L (normal values ≤40 U/L in man and ≤31 U/L in woman). Positive ELISA test to
T. spiralis antigen was found at 30 days after eating raw pork in 6 of 6 patients, and
T. spiralis larvae were detected by muscule biopsy in 6 of 6 patients.
Leptospira test and bacterial culture were negative in 6 of 6 patients (
Table 2). The 6 patients were treated with albendazole 800 mg/day for 10 days, and the symptoms disappeared after 1 month.
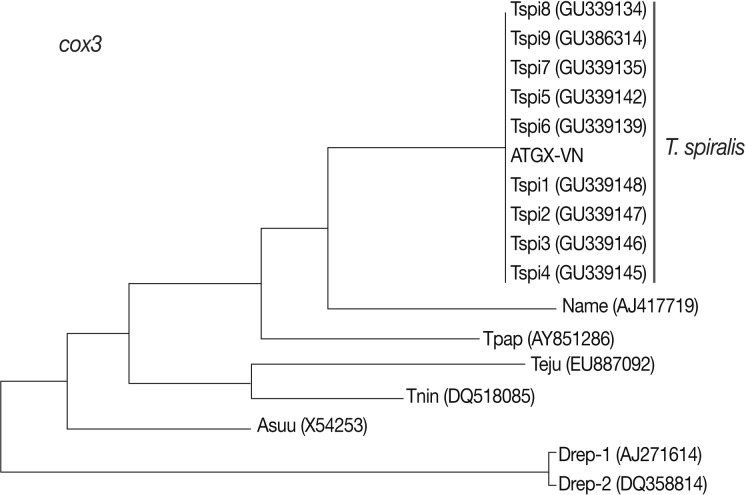
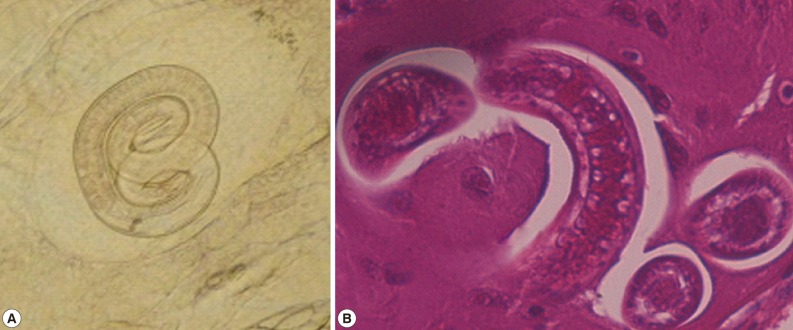
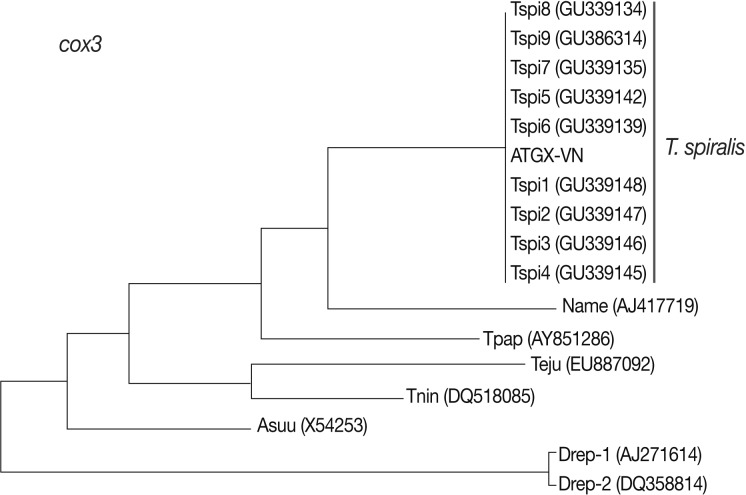
The larvae from the muscle of patients (
Fig. 2A, B) were identified by molecular methods using the mitochondrial cytochrome
c oxidase subunit III (
cox3) gene in comparison with that of the standard strains in GenBank (
Table 3). Comparison of 200 nucleotides of a portion of
cox3 mitochondrial genome between the Vietnamese (ATGX-VN) and other geographical isolates of
T. spiralis, including the Chinese (Tspi1, Tspi2, Tspi3, and Tspi4), US (Tspi5), Spanish (Tspi6), Bulgarian (Tspi7), Finnish (Tspi8), and GenBank (Tspi9) showed that the nucleotide homology between the Vietnamese and Chinese isolates were 100% and that between the Vietnamese and other isolates were 99% (
Table 4). A phylogenetic tree was constructed for
T. spiralis Vietnam and other isolates using
cox3 nucleotide sequences as estimated by neighbor-joining (NJ) using MEGA4.0 [
9]; Vietnamese
T. spiralis was 1 group together with
T. spiralis in the world (
Fig. 3).
DISCUSSION
All 5 trichinosis outbreaks were in the mountainous region of North Vietnam (
Fig. 1). The local people have the habit of feeding pigs outside (free-roaming) and eating raw pork, particularly at parties. This habit in Vietnam is similar in Thailand, Laos, India, and other parts of Asia and the South Pacific [
4]. The second outbreak occurred 31 year after the first outbreak in Vietnam [
2]. It is questioned why there were no other cases of trichinosis for such a long duration. Sometimes, parasitic diseases such as trichinosis may be neglected or misdiagnosed as other diseases by local health authorities due to lack of knowledge. Actually, all the trichinosis patients in 5 outbreaks of Vietnam were misdiagnosed as leptospirosis at first (because this disease caused clinical symptoms, such as fever, illness, and muscle pain), and treated with antibiotics but not anthelmintic drugs. Only after some patients died, they made contact with the national health level and diagnosed as trichinosis. Moreover, trichinosis can be clinically mild and can resemble other diseases, because it does not have pathognomonic signs or symptoms, and in endemic areas, if people frequently eat
Trichinella-infected meat, they can develop an asymptomatic form of the disease [
5]. Hence, the first step for reasonable diagnosis of diseases is thinking every reasons, including parasites. Therefore, the diagnostic clue to differentiate trichinosis from leptospirosis for future outbreaks will become better, especially in the mountainous areas.
The main clinical symptoms in our 6 patients were fever, muscle pain, difficult moving, edema, difficult swallowing, and others which were similar in each patient (
Table 1). Comparing with review of 98 trichinosis patients in 3 outbreaks in Vietnam [
2], the clinical symptoms were similar in all patients and the symptoms developed within 1-30 days after eating infected raw pork (7.9 days in average). The symptoms included fever (100% of patients), muscle pain (100%), difficult moving (90.9-100%), edema (90.9-95.5%), difficult swallowing (11.5-90.9%), weight loss (90.0-90.9%), itching (85.0-86.4%), difficulty in breathing (50.0-80.0%), diarrhea (50.0%), lisping (40.0-68.2%), abdominal pain (35.0-100%), and stool with blood (0-9.1%), and 6 patients died. In an outbreak, serum ELISA test was performed in 21 patients using
T. spiralis antigen, which showed 100% positivity [
2].
In our report, the biopsy for detection of larvae in the muscles of patients showed 100% positive results for
Trichinella larvae (
Fig. 2A, B). The results of ELISA test with
T. spiralis antigen were positive in 6 of 6 patients and 18 other patients in this outbreak. The number of leukocytes, especially eosinophils, increased remarkably. Transaminases increased also in 6 of 6 patients. However, the results of
Leptospira test and bacterial culture were negative.
In every outbreak, patients ate raw pork from domestic pigs, and the pigs were infected with
T. spiralis larvae. For example, in the first outbreak, a pig used for eating was a female pig 8 years old and weighed 50 kg and was infected with 879 larvae/g muscle [
2]. Another male pig in this area was 7 years old, which was infected with 70 larvae/g muscle. In the second outbreak, the patients ate raw pork from a female pig, which was 5 years old and weighed 70 kg and was infected with encysted larvae of
T. spiralis. In the third outbreak, the patients consumed raw pork from a female pig, which was 3 years old and weighed 60 kg. In the fourth outbreak, the patients ate raw pork from a female pig, which was 5 years old and weighed 70 kg and was infected by 1-3 larvae/g muscle [
2,
8]. In the fourth outbreak, 206 (19.9%) of 1,035 domestic pigs (free-roaming) were positive for
T. spiralis ELISA. Muscle samples from 76 serologically positive pigs were tested by artificial digestion, and
Trichinella larvae were detected in 11 (14.5%) of them [
8]. Appearance of clinical symptoms in our cases was not longer (6.0 days in average) than in cases of previous outbreaks (7.9 days in average). In our study, the larvae from humans were identified by molecular methods as
T. spiralis. This is the first time when
T. spiralis from human infections was identified by the molecular method in Vietnam.
ACKNOWLEDGMENTS
We acknowledge the funds supported from the National Foundation for Science and Technology Development (NAFOSTED) in Vietnam (No. 106.12-2011.13 to Nguyen Van De), National Hospital of Tropical Diseases, Bach Mai Hospital and National Centre for Veterinary Diagnosis, Hanoi, Vietnam.
References
- 1. Cook GC. Trichinosis (Trichinella spiralis). Manson's Tropical Diseases. 1997, London, UK. W.B. Saunder Co. Ltd; pp 1403-1407.
- 2. De NV, Dorny P, Waikagul J. Trichinelliasis in Vietnam. Seminar on Food- and Water-borne Parasitic Zoonoses (5th FBPZ). 28-30 November 2006.
- 3. Intapan PM, Chotmongkol V, Tantrawatpan C, Sanpool O, Morakote N, Maleewong W. Molecular identification of Trichinella papuae from a Thai patient with imported trichinellosis. Am J Trop Med Hyg 2011;84:994-997.
- 4. Miyazaki I. Trichinelliasis. Helminthic Zoonoses. 1991, Tokyo, Japan. Southeast Asian Medical Information Center; pp 452-459.
- 5. Owen IL, Morales G, Pezzotti MA, Pozio E. Trichinella infection in a hunting population of Papua New Guinea suggests an ancient relationship of Trichinella with human beings. Trans R Soc Trop Med Hyg 2005;99:618-624.
- 6. Pozio E. World distribution of Trichinella spp. infections in animals and humans. Vet Parasitol 2007;149:3-21.
- 7. Sohn WM, Huh S, Chung DI, Pozio E. Molecular identification of Korean Trichinella isolates. Korean J Parasitol 2003;41:125-126.
- 8. Vu Thi N, Dorny P, La Rosa G, To Long T, Nguyen Van C, Pozio E. High prevalence of anti-Trichinella IgG in domestic pigs of the Son La province, Vietnam. Vet Parasitol 2010;168:136-140.
- 9. Tamura K, Nei M, Kumar S. Prospects for inferring very large phylogenies by using the neighbor-joining method. Proc Natl Acad Sci U S A 2004;101:11030-11035.
Fig. 1Map of the endemic areas of trichinosis in Vietnam.

Fig. 2A Trichinella spiralis larva in the human muscle (A) and section of a T. spiralis larva in the muscle (B).

Fig. 3Phylogenetic tree of
Trichinella spiralis Vietnam and other strains from a part of
cox3 nucleotide sequences estimated by Neighbor-Joining (NJ) method using MEGA4.0 [
6]. Note: ATGX-VN=Vietnamese; Tspi1, Tspi2, Tspi3, Tpsi4=Chinese; Tspi5=US; Tspi6=Spanish; Tspi7=Bulgarian; Tspi8=Finnish; Tspi9=GenBank; Name=
Necator americanus (GenBank no. AJ417719); Tpap=
Trichinella papuae (GenBank no. AY851286); Teju=
Troglosiro cf. juberthiei (GenBank no. EU887092); Tnin=
Troglosiro ninqua (GenBank no. DQ518085); Asuu=
Ascaris suum (GenBank no. X54253); Drep-1 and Drep-2=
Italian Dirofilaria repens (GenBank no. AJ271614 and DQ358814).
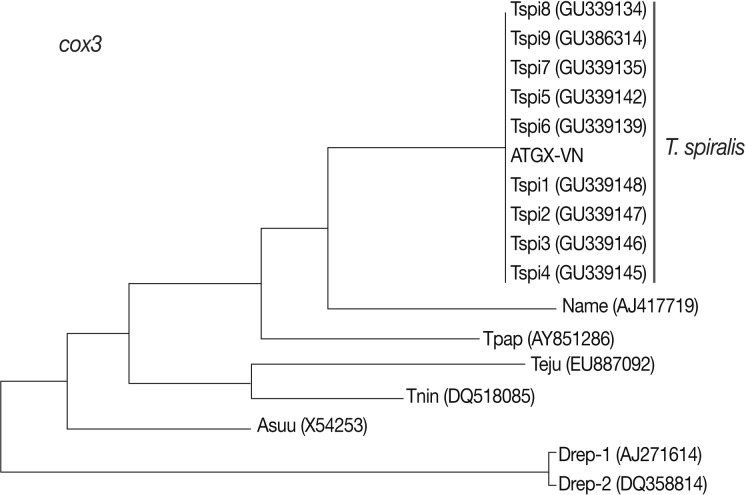
Table 1.The clinical symptoms in 6 trichinosis patients
Table 1.
|
Symptoms |
Patient 1 |
Patient 2 |
Patient 3 |
Patient 4 |
Patient 5 |
Patient 6 |
|
Gender |
Man |
Man |
Woman |
Woman |
Man |
Woman |
|
Age |
39 |
43 |
41 |
30 |
30 |
30 |
|
Fever |
+ |
+ |
+ |
+ |
+ |
+ |
|
Muscular pain |
+ |
+ |
+ |
+ |
+ |
+ |
|
Edema in leg/hand |
+ |
+ |
+ |
+ |
+ |
+ |
|
Edema around eyes |
+ |
+ |
+ |
+ |
+ |
+ |
|
Difficult moving |
+ |
+ |
+ |
+ |
+ |
+ |
|
Difficult swallowing |
+ |
+ |
+ |
+ |
+ |
+ |
|
Difficult breath |
+ |
+ |
+ |
- |
+ |
+ |
|
Loss of weight |
+ |
+ |
+ |
- |
+ |
+ |
|
Itching |
+ |
+ |
+ |
- |
- |
- |
|
Diarrhea |
+ |
- |
- |
- |
- |
- |
|
Time of symptom appearance (days) |
5 |
6 |
7 |
8 |
5 |
5 |
Table 2.Clinical laboratory findings in 6 trichinosis patients
Table 2.
|
Findings |
Patient 1 |
Patient 2 |
Patient 3 |
Patient 4 |
Patient 5 |
Patient 6 |
|
Erythrocyte/mm3
|
4.2 |
5.5 |
4.8 |
3.3 |
4.5 |
3.4 |
|
Leukocyte/mm3
|
17.0 |
13.6 |
12.4 |
12.4 |
11.1 |
10.2 |
|
Eosinophils (%) |
51.8 |
18.6 |
5.1 |
15.9 |
28.4 |
18.5 |
|
AST (U/L) |
219 |
115 |
219 |
65 |
106 |
112 |
|
ALT (U/L) |
471 |
314 |
471 |
74 |
146 |
106 |
|
Serum ELISA test for Trichinella
|
+ |
+ |
+ |
+ |
+ |
+ |
|
Biopsy on Trichinella larvae |
+ |
+ |
+ |
+ |
+ |
+ |
|
Leptospira test |
- |
- |
- |
- |
- |
- |
|
Bacterial culture |
- |
- |
- |
- |
- |
- |
Table 3.Sequencing of a portion of cox3 of different Trichinella isolates from GenBank compared with Trichinella spiralis in Vietnam
Table 3.
|
Notation |
Origin |
Host |
Length |
Species |
GenBank no. |
Author |
|
ATGX-VN |
Vietnama
|
Human |
200 bp |
Trichinella spiralis
|
- |
De et al.a
|
|
Tspi1 |
China |
Sus scrofa
|
200 bp |
Trichinella spiralis
|
GU339148.1 |
Rosenthal et al., 2008 |
|
Tspi2 |
China |
Sus scrofa
|
200 bp |
Trichinella spiralis
|
GU339147.1 |
Rosenthal et al., 2008 |
|
Tspi3 |
China |
Sus scrofa
|
200 bp |
Trichinella spiralis
|
GU339146.1 |
Rosenthal et al., 2008 |
|
Tspi4 |
China |
Sus scrofa
|
200 bp |
Trichinella spiralis
|
GU339145.1 |
Rosenthal et al., 2008 |
|
Tspi5 |
USA |
Mephitis mephitis
|
200 bp |
Trichinella spiralis
|
GU339142.1 |
Rosenthal et al., 2008 |
|
Tspi6 |
Spain |
Sus scrofa
|
200 bp |
Trichinella spiralis
|
GU339139.1 |
Rosenthal et al., 2008 |
|
Tspi7 |
Bulgaria |
Sus scrofa
|
200 bp |
Trichinella spiralis
|
GU339135.1 |
Rosenthal et al., 2008 |
|
Tspi8 |
Finland |
Sus scrofa
|
200 bp |
Trichinella spiralis
|
GU339134.1 |
Rosenthal et al., 2008 |
|
Tspi9 |
GenBank |
Sus scrofa
|
200 bp |
Trichinella spiralis
|
GU386314.1 |
Webb et al., 2010 |
Table 4.Percentage identity in nucleotide sequences of cox3 of a Vietnamese Trichinella spiralis isolate in comparison with other T. spiralis in GenBank
Table 4.
|
ATGX-VN |
Tspi1 |
Tspi2 |
Tspi3 |
Tspi4 |
Tspi5 |
Tspi6 |
Tspi7 |
Tspi8 |
Tspi9 |
|
ATGX-VN |
|
100 |
100 |
100 |
100 |
99 |
99 |
99 |
99 |
99 |
|
Tspi1 |
100 |
|
100 |
100 |
100 |
99 |
99 |
99 |
99 |
99 |
|
Tspi2 |
100 |
100 |
|
100 |
100 |
99 |
99 |
99 |
99 |
99 |
|
Tspi3 |
100 |
100 |
100 |
|
100 |
99 |
99 |
99 |
99 |
99 |
|
Tspi4 |
100 |
100 |
100 |
100 |
|
99 |
99 |
99 |
99 |
99 |
|
Tspi5 |
99 |
99 |
99 |
99 |
99 |
|
100 |
100 |
100 |
100 |
|
Tspi6 |
99 |
99 |
99 |
99 |
99 |
100 |
|
100 |
100 |
100 |
|
Tspi7 |
99 |
99 |
99 |
99 |
99 |
100 |
100 |
|
100 |
100 |
|
Tspi8 |
99 |
99 |
99 |
99 |
99 |
100 |
100 |
100 |
|
100 |
|
Tspi9 |
99 |
99 |
99 |
99 |
99 |
100 |
100 |
100 |
100 |
|