Abstract
Gnathostoma spinigerum can cause subarachnoid hemorrhage (SAH). The detection of specific antibodies in serum against G. spinigerum antigen is helpful for diagnosis of neurognathostomiasis. There is limited data on the frequency of G. spinigerum infection in non-traumatic SAH. A series of patients diagnosed as non-traumatic SAH at the Srinagarind Hospital, Khon Kaen University, Thailand between January 2011 and January 2013 were studied. CT or MR imaging of the brain was used for diagnosis of SAH. Patients were categorized as aneurysmal subarachnoid hemorrhage (A-SAH) or non-aneurysmal subarachnoid hemorrhage (NA-SAH) according to the results of cerebral angiograms. The presence of specific antibodies in serum against 21- or 24-kDa G. spinigerum antigen was determined using the immunoblot technique. The detection rate of antibodies was compared between the 2 groups. Of the 118 non-traumatic SAH patients for whom cerebral angiogram and immunoblot data were available, 80 (67.8%) patients had A-SAH, whereas 38 (32.2%) had NA-SAH. Overall, 23.7% were positive for specific antibodies against 21- and/or 24-kDa G. spinigerum antigen. No significant differences were found in the positive rate of specific antibodies against G. spinigerum in both groups (P-value=0.350).
-
Key words: Gnathostoma spinigerum, non-traumatic subarachnoidal hemorrhage, intracranial aneurysm, cerebral angiogram, gnathostomiasis, immunoblot
Non-traumatic subarachnoid hemorrhage (SAH) is a serious neurological condition causing very severe headache and with a mortality rate that may be as high as 60% [
1]. In 41-82.5% of cases, cerebral aneurysm is the cause of SAH [
2-
4]. However, the cause cannot be determined in about half of all SAH patients.
Gnathostoma spinigerum, a nematode, is endemic in Thailand and Japan [
5]. Infection in humans is caused by consuming raw or uncooked infected meats of intermediate host fish or other paratenic hosts such as the snake and poultry. The majority of gnathostomiasis patients present with cutaneous lesions such as mobile nodular erythema or serpigenous eruption. Involvement of the eyes [
6] and central nervous system (CNS) [
7] has also been sporadically reported.
In particular, CNS involvement is almost exclusively reported from Thailand.
Gnathostoma spinigerum is one possible cause of SAH in Thailand [
8], but clinical data on the frequency of gnathostomiasis in SAH patients is still limited even in areas where gnathostomiasis is endemic. The diagnosis of neurognathostomiasis by detection of
G. spinigerum larva is extremely rare [
9]. It is, therefore, worthwhile to use immunoblot analyses to diagnose neurognathostomiasis. In this study, we examined anti-
G. spinigerum antibody-positive rate in sera of non-traumatic SAH patients in Thailand to elucidate the significance of
G. spinigerum infection as a cause of SAH.
We enrolled non-traumatic SAH patients diagnosed at the Srinagarind Hospital, Khon Kaen University, Khon Kaen, Thailand between January 2011 and January 2013. SAH was verified by non-contrast CT or MR imaging of the brain.
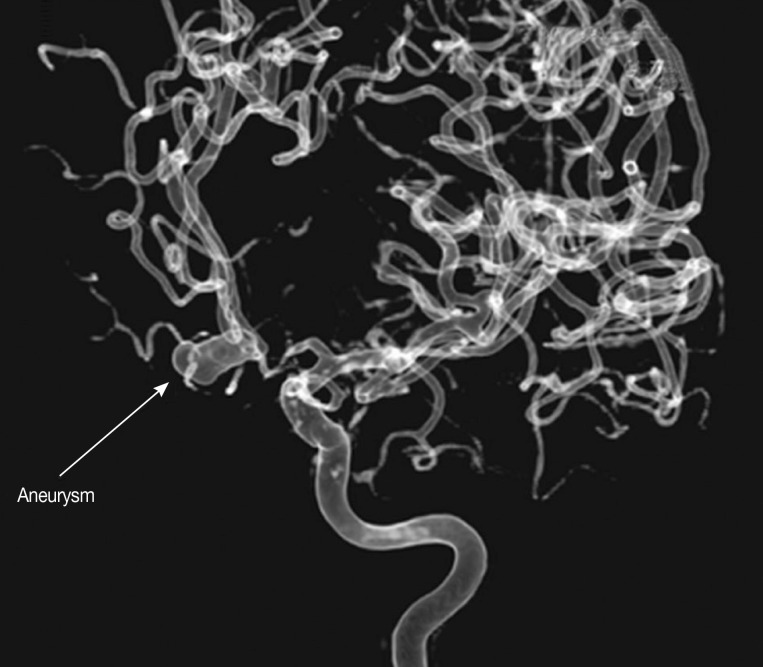
The inclusion criteria included non-traumatic SAH patients for whom 1) results of CT brain imaging (
Fig. 1) or MR imaging of the brain were available, 2) results of CT angiography (CTA) or MR angiography (MRA) or 3-dimensional digital subtraction cerebral angiography (DSA) were available (
Fig. 2) to identify any intracranial aneurysm that might be present (
Fig. 3), and 3) results of immunoblot analysis for antibodies against 21-or 24-kDa antigen band of
G. spinigerum were avaiable. The sensitivity and specificity of immunoblot analysis were 83.3-91.7% and 100%, respectively [
10].
All eligible patients were categorized into 2 groups; aneurysmal SAH (A-SAH) and non-aneurysmal SAH (NA-SAH). The former group included those SAH patients with intracranial aneurysm detected by CTA and/or MRA and/or DSA. The technique and procedures of DSA have been described elsewhere [
11]. Patients with no abnormal cerebral vessels according to DSA were included in the NA-SAH group. Sera of members of both groups were examined for the presence of anti-
G. spinigerum antibody and levels of seropositivity compared between the groups. The study protocol was approved by the Khon Kaen University Ethics Committee for Human Research (HE551056).
During the study period, 118 patients met the criteria. The antibody positive rate in A-SAH group was 26.2% (21/80) and that of NA-SAH group was 18.4% (7/38). Although the antibody-positive rate of A-SAH group was somewhat higher than in NA-SAH group, there was no statistically significant difference between them (
P=0.350). Also, there was no significant difference in age and gender among 4 groups, namely, antibody-positive and negative SAH and antibody-positive and negative NA-SAH groups (
Table 1).
In this study, an overall antibody-positive rate in non-traumatic SAH was 23.7%, but the antibody-positive rate between A-SAH and NA-SAH groups was not significantly different from each other, suggesting that
G. spinigerum infection is a risk factor for SAH but not associated with particular background status of SAH. The samples were selected not just from suspected gnathostomiasis patients but also from overall SAH patients. This is the seroprevalence value of
Gnathostoma antibodies in SAH patients in Thailand. Since the sample size of this study is too small, further accumulation of the samples is necessary to draw any solid conclusion. Gnathostomiasis patients with neurological manifestations do not always have cutaneous intermittent migratory swelling or radicular pain [
7,
12-
14]. Therefore, physicians working in gnathostomiasis endemic areas should aware that gnathostomiasis can be a cause of SAH. In this study, IgG antibody detection using immunoblotting was employed to detect
G. spinigerum infection, so that there is a risk of surpassing antibody-negative or IgM-antibody positive acute stage cases. However, this possibility is rather unlikely because most of neurognathostomiasis patients in Thailand have infections for years before development of neurological complications [
7].
In conclusion, the detection rate of G. spinigerum antibodies in non-traumatic SAH was 23.7%. The rate was somewhat higher in A-SAH than in NA-SAH group. Other history findings should be included for supportive evaluation. Whether such a detection rate is seen in other countries or in other diseases should be clarified in a comparative study.
Office of the Higher Education CommissionKhon Kaen UniversityCHE Ph.D. ScholarshipThailand Research FundRTA5580004
ACKNOWLEDGMENTS
This research was funded by grants from the Office of the Higher Education Commission for supporting grant funded under the Strategic Scholarships for Frontier Research Networks for Ph.D. program Thai Doctoral degree (CHE Ph.D. Scholarship) and the Higher Education Research Promotion and National Research University Project of Thailand, Office of the Higher Education Commission through the Health Cluster (SHeP-GMS) and Khon Kaen University, Khon Kaen, Thailand. Penchom Janwan was supported by a CHE Ph.D. Scholarship. Wanchai Maleewong and Pewpan M. Intapan were supported by TRF Senior Research Scholar Grant, Thailand Research Fund grant no. RTA5580004.
References
- 1. Ingall T, Asplund K, Mähönen M, Bonita R. A multinational comparison of subarachnoid hemorrhage epidemiology in the WHO MONICA stroke study. Stroke 2000;31:1054-1061.
- 2. Ammar A, al-Rajeh S, Ibrahim AW, Chowdhary UM, Awada A. Pattern of subarachnoid haemorrhage in Saudi Arabia. Acta Neurochir (Wien) 1992;114:16-19.
- 3. Uysal E, Yanbuloğlu B, Ertürk M, Kilinç BM, Başak M. Spiral CT angiography in diagnosis of cerebral aneurysms of cases with acute subarachnoid hemorrhage. Diagn Interv Radiol 2005;11:77-82.
- 4. Urbach H, Zentner J, Solymosi L. The need for repeat angiography in subarachnoid haemorrhage. Neuroradiology 1998;40:6-10.
- 5. Waikagul J, Diaz Chamacho SP. Gnathostomiasis. In Murrell KD, Fried B eds, Food-borne Parasitic Zoonoses. World Class Parasites. Vol. 11:New York, USA. Springer; 2007, pp 235-261.
- 6. Nawa Y, Katchanov J, Yoshikawa M, Rojekittikhun W, Dekumyoy P, Kusolusuk T, Dorn Wattanakulpanich D. Ocular gnathostomiasis: a comprehensive review. J Trop Med Parasitol 2010;33:77-86.
- 7. Katchanov J, Sawanyawisuth K, Chotmongkol V, Nawa Y. Neurognathostomiasis, a neglected parasitosis of the central nervous system. Emerg Infect Dis 2011;17:1174-1180.
- 8. Sawanyawisuth K, Chlebicki MP, Pratt E, Kanpittaya J, Intapan PM. Sequential imaging studies of cerebral gnathostomiasis with subdural hemorrhage as its complication. Trans R Soc Trop Med Hyg 2009;103:102-104.
- 9. Sangchan A, Sawanyawisuth K, Intapan PM, Mahakkanukrauh A. Outward migration of Gnathostoma spinigerum in interferon-alpha treated hepatitis C patient. Parasitol Int 2006;55:31-32.
- 10. Intapan PM, Khotsri P, Kanpittaya J, Chotmongkol V, Sawanyawisuth K, Maleewong W. Immunoblot diagnostic test for neurognathostomiasis. Am J Trop Med Hyg 2010;83:927-929.
- 11. Kitkhuandee A, Thammaroj J, Munkong W, Duangthongpon P, Thanapaisal C. Cerebral angiographic findings in patients with non-traumatic subarachnoid hemorrhage. J Med Assoc Thai 2012;95(suppl 11):S121-S129. (in press). Full text. e-Journal: http://jmat.mat.or.th
- 12. Sawanyawisuth K, Tiamkao S, Nitinavakarn B, Dekumyoy P, Jitpimolmard S. MR imaging findings in cauda equina gnathostomiasis. AJNR Am J Neuroradiol 2005;26:39-42.
- 13. Sawanyawisuth K, Tiamkao S, Kanpittaya J, Dekumyoy P, Jitpimolmard S. MR imaging findings in cerebrospinal gnathostomiasis. AJNR Am J Neuroradiol 2004;25:446-449.
- 14. Kanpittaya J, Sawanyawisuth K, Intapan PM, Khotsri P, Chotmongkol V, Maleewong W. A comparative study of neuroimaging features between human neuro-gnathostomiasis and angiostrongyliasis. Neurol Sci 2012;33:893-898.
Fig. 1Non-contrast CT axial view showing hyperdense area of subarachnoid hemorrhage (SAH) along the interhemispheric fissure.

Fig. 2Three-dimensional digital subtraction cerebral angiography (DSA) showing the normal posterior circulation artery, vertebral artery, basilar artery, posterior cerebral artery, and superior cerebellar artery.

Fig. 3Three-dimensional digital subtraction cerebral angiography (DSA), lateral view of internal carotid artery and anterior cerebral artery showing subarachnoid hemorrhage from aneurysm at anterior communicating artery.

Table 1.Characteristics of non-traumatic subarachnoid hemorrhage (SAH) patients who were seropositive or seronegative for specific antibodies against Gnathostoma spinigerum by immunoblotting
Table 1.
|
Variables |
Aneurysmal SAH antibody (+) N = 21 (26.2%) |
Aneurysmal SAH antibody (-) N = 59 (73.8%) |
Non-aneurysmal SAH antibody (+) N = 7 (18.4%) |
Non-aneurysmal SAH antibody (-) N = 31 (81.6%) |
P-value |
|
Mean (SD) age, years |
55.0 (8.6) |
53.1 (14.0) |
49.3 (11.2) |
54.4 (13.3) |
0.744a
|
|
Male gender |
13 (61.9) |
23 (39.0) |
4 (57.1) |
15 (48.4) |
0.293b
|
Citations
Citations to this article as recorded by